Overview
This article aims to help parents understand the symptoms of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD). By shedding light on these complex conditions, we hope to empower parents as they navigate their children's challenges. Recognizing overlapping symptoms is crucial, as it can often lead to difficulties in accurate diagnosis. Parents may feel overwhelmed, but being informed allows them to advocate effectively for their children's needs.
Understanding these conditions is not just about recognizing symptoms; it's about acknowledging the emotional journey that families face. Parents often find themselves questioning what they can do to support their children. Effective treatment strategies exist, and informed parents can access the necessary support systems. Together, we can create a nurturing environment where children thrive.
If you are a parent grappling with these issues, remember that you are not alone. We encourage you to share your experiences and seek out resources that can provide the guidance you need. By connecting with others and accessing support, you can make a significant difference in your child's life.
Introduction
Navigating the intricate landscape of childhood mental health can feel overwhelming, especially for parents who are trying to make sense of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD). These conditions, each with their own unique yet sometimes overlapping symptoms, pose significant challenges not just for the children affected but also for the families who love and support them. As parents embark on this journey of understanding, it is essential to recognize the differences between OCD's persistent obsessions and compulsions and ADHD's impulsivity and inattention.
This article seeks to illuminate the definitions, symptoms, and treatment approaches for OCD and ADHD, providing valuable insights and resources designed to empower parents in advocating for their children's needs. By nurturing a deeper understanding of these conditions, families can pave the way for effective management and support, ensuring that their children can thrive despite the hurdles they may encounter. Together, we can foster an environment where understanding leads to action, and where every child receives the care they deserve.
Defining OCD and ADHD: Key Concepts for Parents
Obsessive-Compulsive Disorder (OCD) can be overwhelming for both children and their parents. It is characterized by persistent, intrusive thoughts known as obsessions, which often lead to repetitive behaviors or mental acts called compulsions. These compulsions are typically performed in an attempt to alleviate the anxiety caused by the obsessions. Common obsessions may include fears of contamination, harm, or the need for symmetry, while compulsions can manifest as excessive cleaning, checking, or counting behaviors.
The impact of OCD on a child's daily functioning can be significant. Symptoms often begin around age 11, but treatment typically starts around age 13, which is an average of two years after symptoms first appear. This delay can be frustrating and concerning for parents. Research shows that OCD patients exhibit reduced grey matter in several brain regions, including the prefrontal cortex, highlighting the neurobiological underpinnings of the disorder.
In contrast, Attention-Deficit/Hyperactivity Disorder (ADHD) presents its own set of challenges. This neurodevelopmental condition is defined by a continuous pattern of inattention, hyperactivity, and impulsivity. Children with ADHD may find it challenging to focus on tasks, follow instructions, or remain seated, which can adversely affect their academic performance and social interactions. The occurrence of ADHD among youngsters is significant, with estimates indicating that around 5% are diagnosed with this condition.
Additionally, the 7-repeat allele of the DRD4 gene has a significant association with ADHD (OR 1.33, 95% CI 1.15-1.54), indicating a genetic component to its development. Understanding these definitions is crucial for parents as they navigate the complexities of these disorders.
For instance, a case study titled "Etiology of OCD in Youth" examines the neurobiological and metacognitive-behavioral factors contributing to the development of OCD in young individuals. It discusses genetic predispositions and environmental influences, as well as the role of dysfunctional thought patterns. This emphasizes the need for comprehensive treatment approaches that address these underlying issues.
Andreas Warnke, a writer in the field, states, "The findings highlight the significance of treating obsessive-compulsive disorder early," underscoring the urgency of addressing these disorders in youngsters. By identifying the symptoms of OCD and ADHD and the underlying factors linked to these conditions, parents can better assist their kids in handling these challenges and pursuing suitable interventions.
This foundational knowledge empowers parents to advocate effectively for their children, ensuring they receive the necessary support and resources. Remember, you are not alone in this journey; seeking help and understanding is the first step toward brighter days ahead.
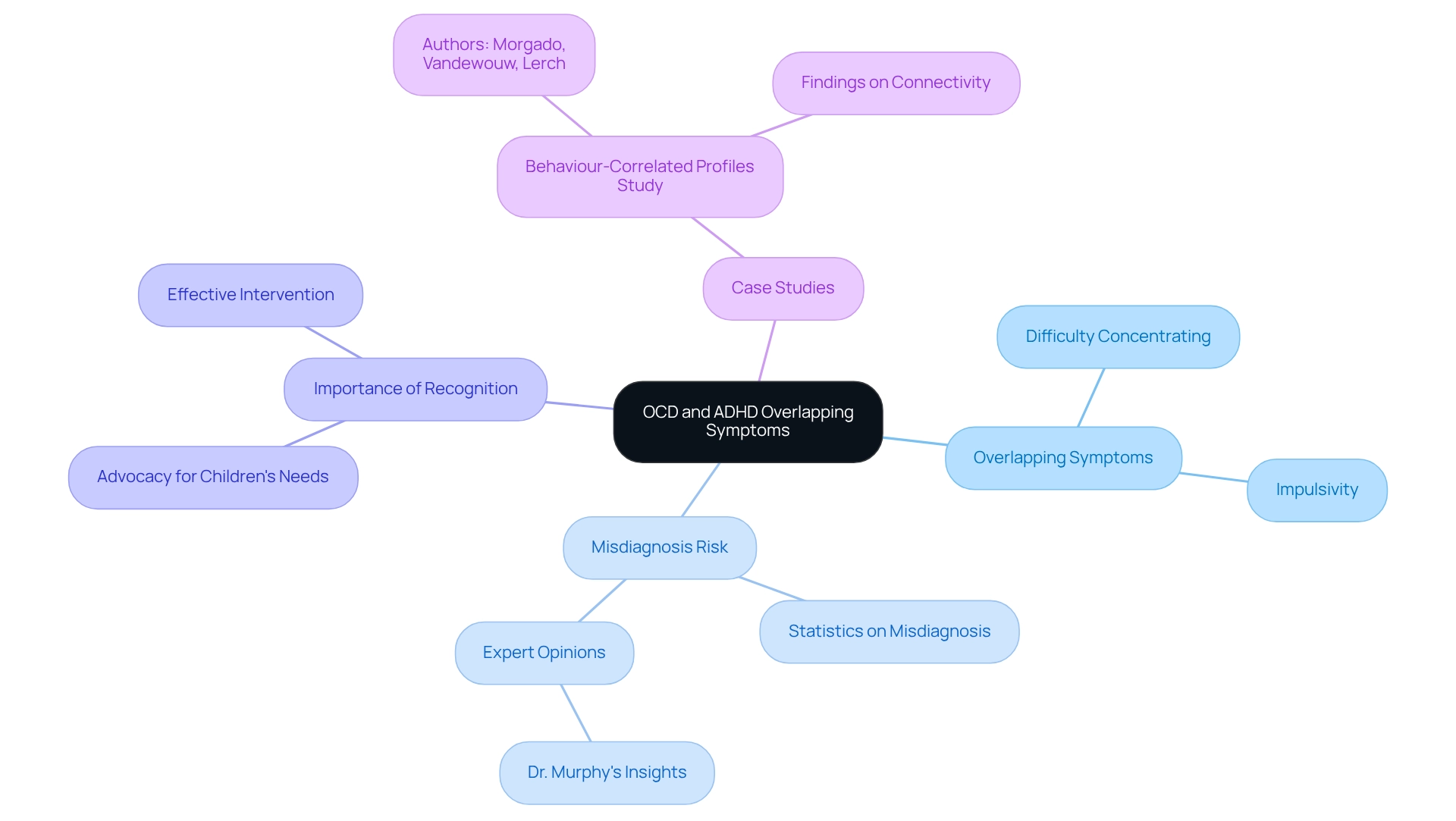
Recognizing Overlapping Symptoms: OCD and ADHD in Focus
Both OCD and attention deficit disorder can present overlapping symptoms, making it essential for parents to recognize these signs to prevent misdiagnosis. Common symptoms include difficulty concentrating and impulsivity. For example, a youth with obsessive-compulsive disorder may become so engrossed in their compulsions that they appear inattentive, while a young person with attention deficit hyperactivity disorder might struggle to focus due to distractibility.
Research indicates that misdiagnosis between these two conditions is not uncommon; OCD can lead to symptoms that mimic another disorder, complicating the diagnostic journey. Statistics reveal that a significant percentage of young individuals diagnosed with attention deficit hyperactivity disorder may also exhibit symptoms of OCD, contributing to potential misdiagnosis. Experts stress the importance of understanding the nuances of OCD and ADHD symptoms.
Psychologists specializing in youth have noted that the compulsive behaviors associated with OCD can often be confused with the impulsiveness linked to ADHD. This misunderstanding can result in inappropriate care strategies that fail to address the young person's actual needs. Murphy has pointed out the complexities involved in diagnosing these conditions, underscoring the critical nature of accurate diagnosis for effective intervention.
Case studies, such as the one conducted by Morgado, Vandewouw, and Lerch, highlight the unique behavior-correlated profiles of connectivity in youngsters with neurodevelopmental disorders. These findings deepen our understanding of how OCD and attention disorders can coexist and impact a young person's behavior, emphasizing the need for further research into management strategies for OCD patients with coexisting attention disorders. In summary, acknowledging the symptoms of OCD and ADHD is vital for parents.
By recognizing these similarities and the risk of misdiagnosis, parents can advocate more effectively for their children's needs, ensuring they receive the appropriate support and care.
The Comorbidity Factor: How Common Are OCD and ADHD Together?
Research indicates that approximately 11.8% of youth diagnosed with Obsessive-Compulsive Disorder (OCD) also exhibit symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD). This significant overlap can complicate management strategies, as the impulsivity associated with ADHD often disrupts the structured routines essential for managing the symptoms of both conditions. For instance, children with ADHD may struggle to adhere to the regular methods necessary to alleviate the symptoms of OCD and ADHD, leading to increased frustration and challenges in both areas.
Moreover, the risk of ADHD among parents and siblings of children with ADHD is heightened by two to eight times, underscoring the familial nature of these conditions and their implications for care. Understanding the potential comorbidity of OCD and ADHD symptoms is vital for parents, as this awareness empowers them to advocate effectively for their child's unique needs. Findings from studies on adults reveal that the symptoms of OCD and ADHD present significant differences in clinical characteristics and outcomes, suggesting that experiences in childhood may mirror those in adulthood.
Furthermore, clinicians are encouraged to consider impulsivity and risk-taking behavior as diagnostic factors. This insight can inform parents about the nuances in diagnosis and care strategies. By recognizing the interplay between these disorders, parents can collaborate with healthcare professionals to develop comprehensive care plans that address the symptoms of OCD and ADHD, ultimately enhancing their child's overall well-being. Emphasizing multimodal approaches can lead to more effective treatment strategies, ensuring that all aspects of a young person's health are thoughtfully considered.
Navigating Diagnostic Challenges: Understanding Co-occurrence
Diagnosing OCD and attention deficit hyperactivity disorder can be quite challenging, especially because the symptoms of these conditions often overlap. Imagine a young person struggling with both OCD and ADHD, where inattention arises from persistent obsessive thoughts—these can easily be misidentified as attention deficit hyperactivity disorder. On the flip side, the impulsivity that is commonly seen in ADHD may be misunderstood as compulsive behavior linked to OCD.
This diagnostic confusion highlights the critical need for thorough evaluations by qualified professionals who specialize in these disorders. Research indicates that individuals diagnosed with both OCD and ADHD experience greater levels of impairment compared to those with OCD alone or healthy controls. A study involving ninety-three unaffected comparison individuals underscores the importance of precise diagnosis and tailored treatment strategies. Alarmingly, misdiagnosis rates can be high, with many children receiving incorrect labels initially, which can lead to ineffective interventions.
Experts stress the importance of distinguishing between these two conditions. Child psychiatrists often point out that while both disorders can present similar symptoms, the underlying motivations are quite different. For instance, compulsive actions in OCD are driven by anxiety and a need to alleviate discomfort, whereas impulsiveness in ADHD typically stems from difficulties with self-control.
A comprehensive evaluation should encompass detailed behavioral assessments, interviews with parents and teachers, and standardized rating scales. This approach enables clinicians to accurately differentiate between OCD and ADHD, paving the way for effective treatment strategies. Key data sources, such as the MarketScan® databases and the National Survey of Children's Health, offer valuable insights into the prevalence and misdiagnosis rates of these disorders.
Consider the case of T., a young boy diagnosed with attention deficit hyperactivity disorder and generalized anxiety disorder. His experience sheds light on the complexities of these diagnoses. From an early age, T. exhibited significant anxiety, which led to obsessive-compulsive symptoms that severely impacted his functioning at home and school.
He expressed his distress poignantly, saying, "I do not know what is happening to me; I do not feel like myself." Despite engaging in psychotherapy, he continued to struggle with intrusive thoughts and compulsions, highlighting the need for ongoing support and intervention. T.'s story exemplifies the importance of recognizing the interplay between ADHD and OCD, reinforcing the necessity for careful and comprehensive diagnostic processes.
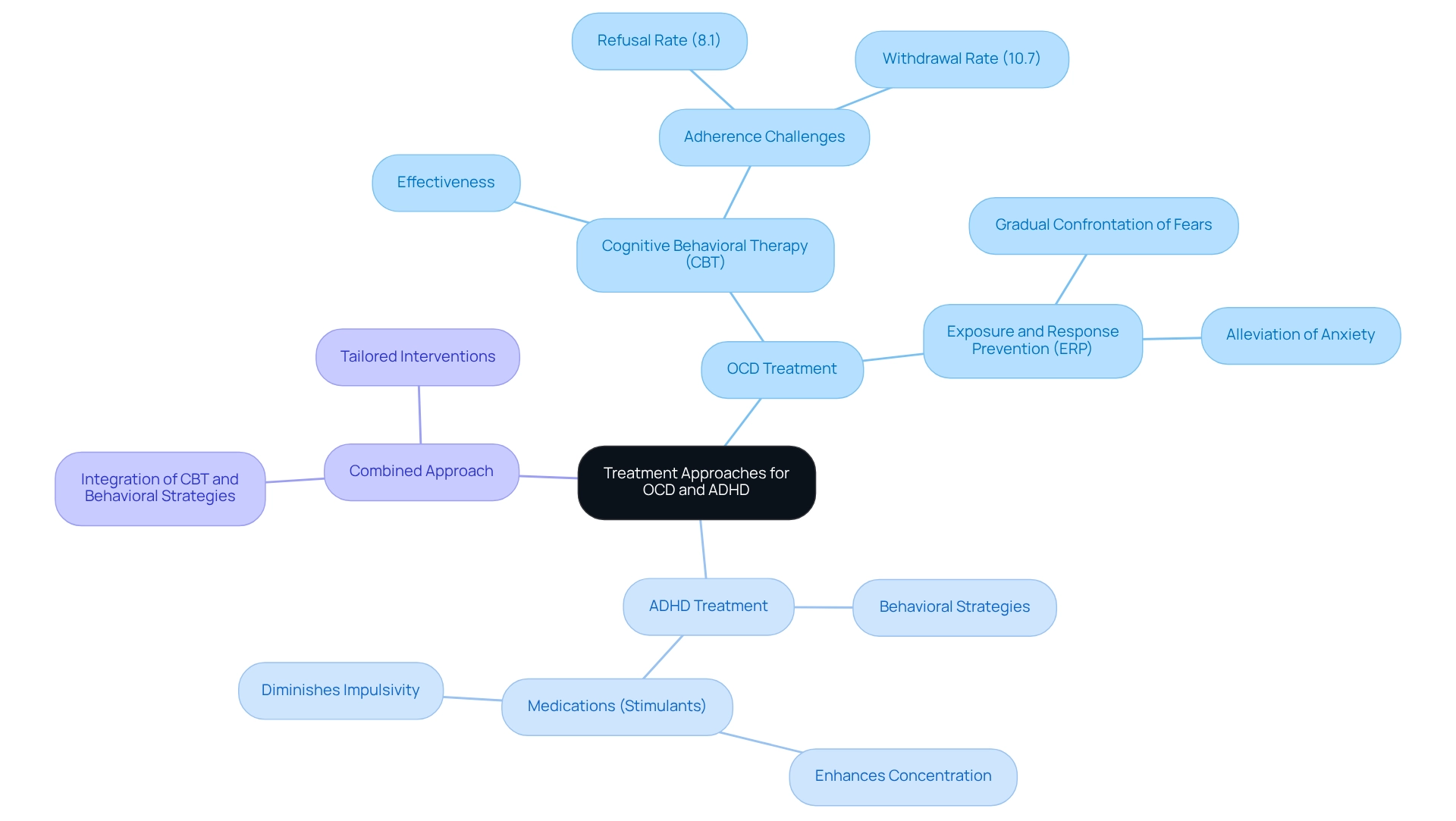
Treatment Approaches: Managing OCD and ADHD Effectively
Effective intervention for Obsessive-Compulsive Disorder (OCD) often centers around Cognitive Behavioral Therapy (CBT), especially the Exposure and Response Prevention (ERP) technique. This compassionate approach encourages children to gradually confront their fears, significantly alleviating anxiety and compulsive behaviors. Meanwhile, Attention-Deficit/Hyperactivity Disorder (ADHD) is typically managed with a combination of behavioral strategies and medications, such as stimulants, which are known to enhance concentration and diminish impulsivity.
When OCD and ADHD symptoms coexist, a combined approach becomes essential. This strategy thoughtfully integrates elements from both CBT and behavioral interventions, tailored to meet the unique challenges each disorder presents. For instance, a recent study evaluating a telephone-administered CBT program for OCD revealed that both in-person and remote therapy options were effective, highlighting the adaptability in service delivery.
The trial included 80 participants aged 11 to 18 and employed the Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS) to assess outcomes, underscoring the significance of evidence-based practices in therapy. Moreover, research indicates that while CBT is widely regarded as the first-line therapeutic strategy for pediatric OCD, as noted by Haitao Zhang, there remains a pressing need for higher quality trials to fully confirm its efficacy. In a review of treatment outcomes, it was observed that 8.1% of participants in a CBT group refused treatment, and 10.7% withdrew, suggesting that although CBT is effective, adherence can be a challenge.
Insights from therapists highlight the importance of combining treatment strategies for OCD and ADHD symptoms, as this dual approach may lead to improved outcomes. By addressing both conditions simultaneously, parents and professionals can better support young individuals in managing their symptoms and enhancing their overall quality of life. If you have experiences or thoughts to share, we encourage you to connect with us in the comments or through our newsletter, as your insights can help foster a supportive community.
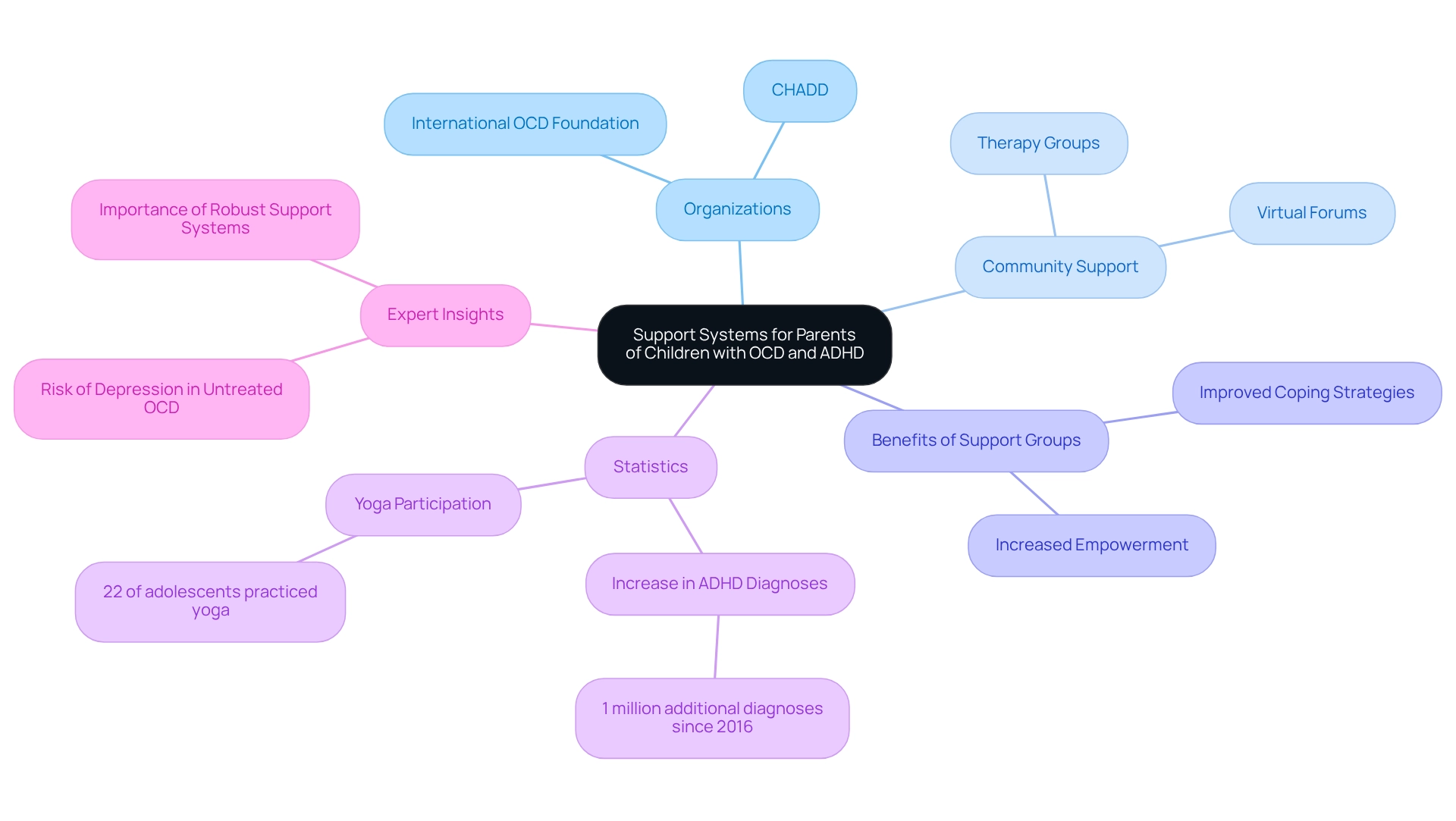
Building Support Systems: Resources for Parents of Children with OCD and ADHD
Parents navigating the challenges of OCD can find a wealth of resources designed to support their journey. Organizations such as the International OCD Foundation and CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) serve as vital sources of information and community support, helping to understand the symptoms of OCD and ADHD. They offer educational materials and guidance tailored to these conditions. Additionally, community therapy groups and virtual forums provide essential avenues for parents to exchange experiences, tactics, and emotional assistance, greatly alleviating feelings of isolation.
Support groups specifically for parents of youngsters with OCD have shown positive results. Statistics indicate that parents who engage in these groups report increased feelings of empowerment and improved coping strategies. For instance, a significant 22% of teenagers have participated in yoga, a practice that can be beneficial for managing stress and anxiety. This underscores the importance of comprehensive approaches in care plans.
Case studies reveal that numerous youngsters aged 3–17 years received attention for attention deficit hyperactivity disorder primarily from pediatricians and nurse practitioners, highlighting the necessity for accessible support systems. However, disparities exist, particularly for youth with Medicaid, who are less likely to receive specialized ADHD treatment. This accentuates the importance of establishing strong support networks to bridge these gaps in care.
As noted by Danielson ML in 2022, an additional 1 million U.S. youngsters aged 3-17 years received a diagnosis of attention deficit hyperactivity disorder compared to 2016, emphasizing the growing need for effective support systems. Moreover, individuals with OCD are at risk of developing depression if left untreated, highlighting the urgency of obtaining support and resources. Expert insights suggest that fostering a robust support system is essential for families dealing with the symptoms of OCD and ADHD.
By connecting with local and online resources, parents can gain valuable information and foster a sense of community that enhances their ability to advocate for their children. Engaging with support organizations equips parents with the tools they need to navigate the complexities of these conditions effectively.
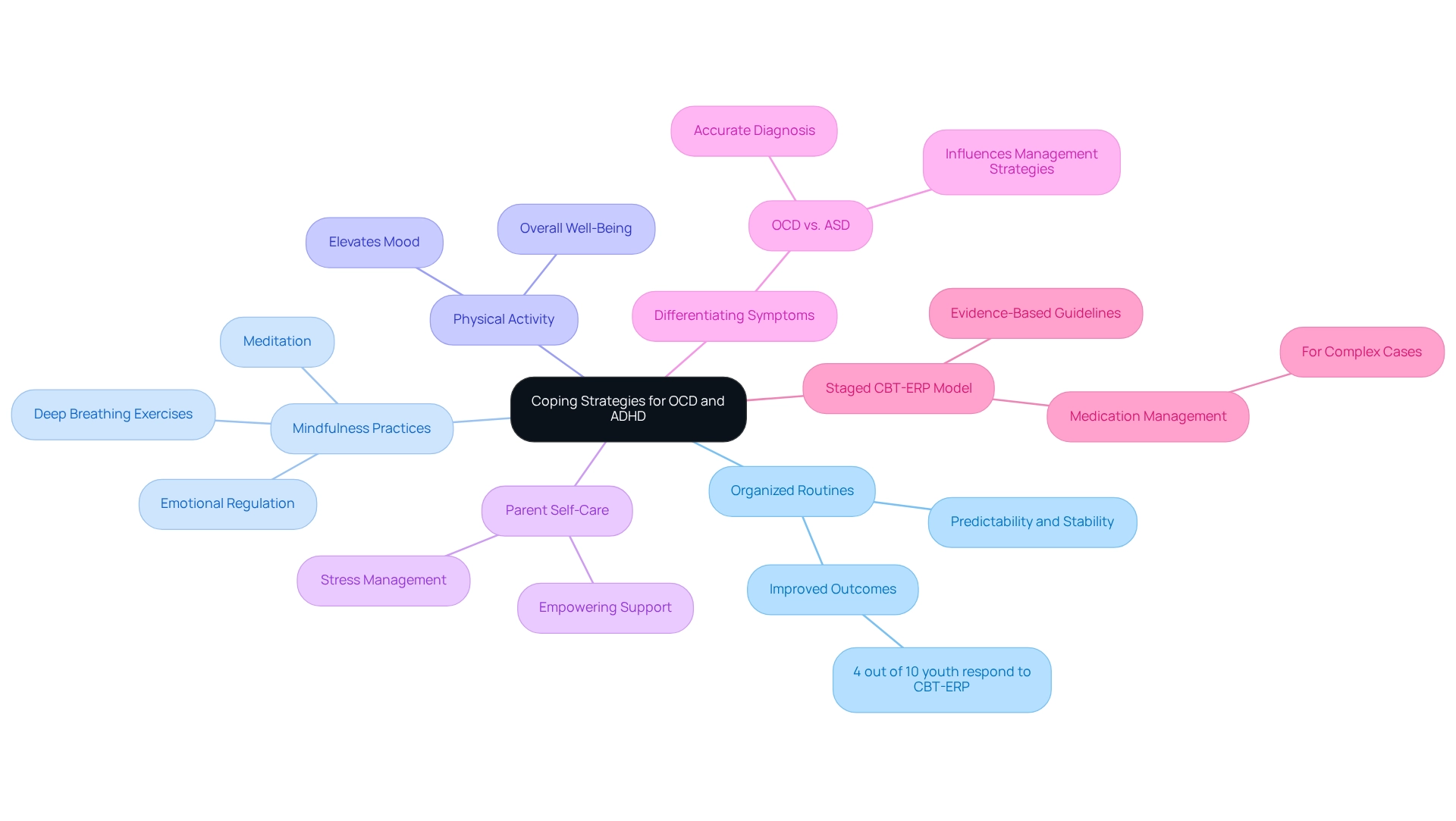
Coping Strategies and Lifestyle Adjustments for Families
Families can adopt a range of effective coping strategies to help manage the symptoms of OCD and ADHD. One particularly beneficial approach is creating organized routines, which provide predictability and stability for individuals with OCD, thereby helping to alleviate anxiety. Research shows that structured routines can lead to significantly improved outcomes, with studies indicating that 4 out of 10 youth experience early and sustained responses to cognitive-behavioral therapy (CBT) after just seven sessions.
In addition, a comparative study on functional impairment in youth with OCD highlights that those with symptoms of both OCD and ADHD face considerable challenges in functioning and school performance. This underscores the importance of implementing effective coping strategies. Mindfulness practices, such as meditation and deep breathing exercises, can also play a vital role in reducing anxiety and enhancing focus. These techniques have proven effective in managing the symptoms of OCD and ADHD, promoting emotional regulation and concentration.
Regular physical activity is another essential component; it not only elevates mood but also contributes to overall well-being, making it a crucial part of a comprehensive management plan. Furthermore, parents should make their own self-care a priority to effectively manage stress levels. This self-care is essential, as it empowers parents to better support their children through various challenges.
Real-world examples show that families who implement these lifestyle changes often report improved dynamics and reduced symptoms. It’s also important for parents to distinguish between OCD and ASD symptoms to ensure accurate diagnosis and treatment, as this understanding can significantly influence management strategies. In more complex cases, a staged CBT-ERP model of care may include medication management, following evidence-based guidelines.
As noted by Maria Pontillo, the authors declare that they have no competing interests, reinforcing the importance of evidence-based approaches in managing these conditions. By nurturing a supportive environment and utilizing these strategies, families can navigate the complexities of OCD and ADHD symptoms more effectively.
Conclusion
Navigating the challenges of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) requires a nuanced understanding of both conditions. This article has outlined the distinct characteristics of OCD, marked by persistent obsessions and compulsions, and ADHD, characterized by impulsivity and inattention. Recognizing the symptoms and the potential for misdiagnosis is crucial for parents. By understanding the overlapping symptoms and the complexities involved in diagnosing these disorders, parents can advocate more effectively for their children, ensuring they receive the appropriate support and treatment.
The significant comorbidity between OCD and ADHD presents additional challenges, as many children may experience symptoms of both disorders. This overlap necessitates a comprehensive treatment approach that addresses the unique needs of each condition. Effective management often involves a combination of cognitive-behavioral therapy, behavioral interventions, and sometimes medication. Parents are encouraged to seek out resources and support systems, such as local organizations and online communities, to enhance their understanding and coping strategies.
Ultimately, fostering a supportive environment at home, implementing structured routines, and prioritizing self-care are essential components in helping children manage these conditions. By embracing a proactive approach and utilizing the insights shared in this article, families can navigate the complexities of OCD and ADHD, empowering their children to thrive despite the challenges they may face.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
OCD is a mental health condition characterized by persistent, intrusive thoughts (obsessions) that lead to repetitive behaviors or mental acts (compulsions) performed to alleviate anxiety caused by these obsessions.
What are some common obsessions and compulsions associated with OCD?
Common obsessions may include fears of contamination, harm, or the need for symmetry. Compulsions can manifest as excessive cleaning, checking, or counting behaviors.
At what age do symptoms of OCD typically begin, and when does treatment usually start?
Symptoms of OCD often begin around age 11, but treatment typically starts around age 13, which is an average of two years after symptoms first appear.
How does OCD impact a child's daily functioning?
The impact of OCD on a child's daily functioning can be significant, affecting their ability to engage in normal activities and interactions due to the distress caused by their obsessions and compulsions.
What are the neurobiological factors associated with OCD?
Research indicates that OCD patients exhibit reduced grey matter in several brain regions, including the prefrontal cortex, highlighting the neurobiological underpinnings of the disorder.
What is Attention-Deficit/Hyperactivity Disorder (ADHD)?
ADHD is a neurodevelopmental condition characterized by a continuous pattern of inattention, hyperactivity, and impulsivity, which can adversely affect a child's academic performance and social interactions.
What is the prevalence of ADHD among children?
Estimates suggest that around 5% of children are diagnosed with ADHD.
Is there a genetic component to ADHD?
Yes, the 7-repeat allele of the DRD4 gene has a significant association with ADHD, indicating a genetic component to its development.
Why is it important for parents to understand OCD and ADHD?
Understanding these disorders helps parents navigate their complexities, recognize symptoms, and advocate effectively for appropriate interventions and support for their children.
How can OCD and ADHD symptoms overlap?
Symptoms of OCD and ADHD can overlap, such as difficulty concentrating and impulsivity. For instance, a child with OCD may appear inattentive due to being engrossed in compulsions, while a child with ADHD may struggle to focus due to distractibility.
What are the risks of misdiagnosing OCD and ADHD?
Misdiagnosis between these two conditions is not uncommon, as OCD can lead to symptoms that mimic ADHD, complicating the diagnostic process and potentially resulting in inappropriate care strategies.
What should parents do to ensure their child receives appropriate support?
Parents should recognize the similarities and risks of misdiagnosis between OCD and ADHD, which enables them to advocate more effectively for their children's needs and ensure they receive the appropriate support and care.




