Overview
This article aims to help parents understand the symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder (OCD). By recognizing these conditions in their children, parents can take meaningful steps toward support and intervention.
We explore key characteristics of both disorders, their overlaps, and distinct features, while also addressing the risks of misdiagnosis. Understanding these nuances is crucial for effective treatment strategies.
Ultimately, we emphasize the importance of tailored approaches and supportive systems, which can lead to better outcomes in managing ADHD and OCD symptoms. Together, let’s navigate this journey with compassion and care.
Introduction
In a world where mental health challenges among children are increasingly recognized, ADHD and OCD emerge as two of the most prevalent disorders, each presenting its own unique set of symptoms and complexities. For parents, understanding the distinctions between these conditions is crucial as they navigate the often turbulent waters of childhood behavioral issues.
ADHD, characterized by inattention and impulsivity, can easily be confused with the anxiety-driven compulsions of OCD. Research reveals a significant overlap between the two, highlighting the paramount need for accurate diagnosis and tailored treatment strategies.
This article explores the key characteristics, common symptoms, and effective interventions for ADHD and OCD, while also emphasizing the importance of community support and resources for families facing these challenges. By equipping parents with knowledge and tools, the journey toward understanding and managing these disorders can transform into a collaborative and empowering experience.
Defining ADHD and OCD: Key Characteristics
Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by enduring patterns of inattention, hyperactivity, and impulsivity. Key traits include:
- Difficulty sustaining attention
- Excessive fidgeting
- Impulsive decision-making
Recent statistics reveal that among individuals aged 12–17 years, the occurrence of ADHD varies significantly by race:
- 17.0% for White individuals
- 13.0% for Black individuals
- 11.7% for Hispanic individuals
It’s important to note that children aged 5–11 years are less likely to experience ADHD than those aged 12–17 years across all family income levels. This highlights the critical need for early identification of symptoms, as they can present differently across various populations.
In contrast, Obsessive-Compulsive Disorder (OCD) is defined by the presence of obsessions—intrusive thoughts that provoke anxiety—and compulsions, which are repetitive behaviors performed to alleviate that anxiety. Children with OCD often engage in specific rituals, such as excessive handwashing or checking behaviors, to manage their distress. Understanding these key traits is vital for guardians, as it empowers them to recognize possible signs in their children and seek suitable assistance.
Recent studies underscore the simultaneous presence of ADHD and OCD symptoms. Research suggests that children displaying both ADHD and OCD symptoms may be at an increased risk of developing further OCD symptoms. As Nazik Elgaddal from the National Center for Health Statistics observes, "The interaction between attention deficit hyperactivity disorder and obsessive-compulsive disorder can complicate diagnosis and treatment, making it crucial for caregivers to be vigilant and informed." This relationship emphasizes the need for comprehensive assessments that consider both ADHD and OCD symptoms.
Additionally, a case study investigating the occurrence of ADHD by family income shows that children from households under the federal poverty threshold have an occurrence rate of 14.8%, which drops to 10.1% for those at or above 200% of the federal poverty threshold. This trend suggests that socioeconomic factors may influence the manifestation of these disorders.
By understanding the unique yet interconnected symptoms of OCD and related conditions, caregivers can more effectively address their children’s behavioral challenges and support suitable treatment alternatives. At ASD Media, we are committed to fostering collaboration and growth within the ABA therapy industry, providing resources and support that empower parents to unlock the potential of their children.
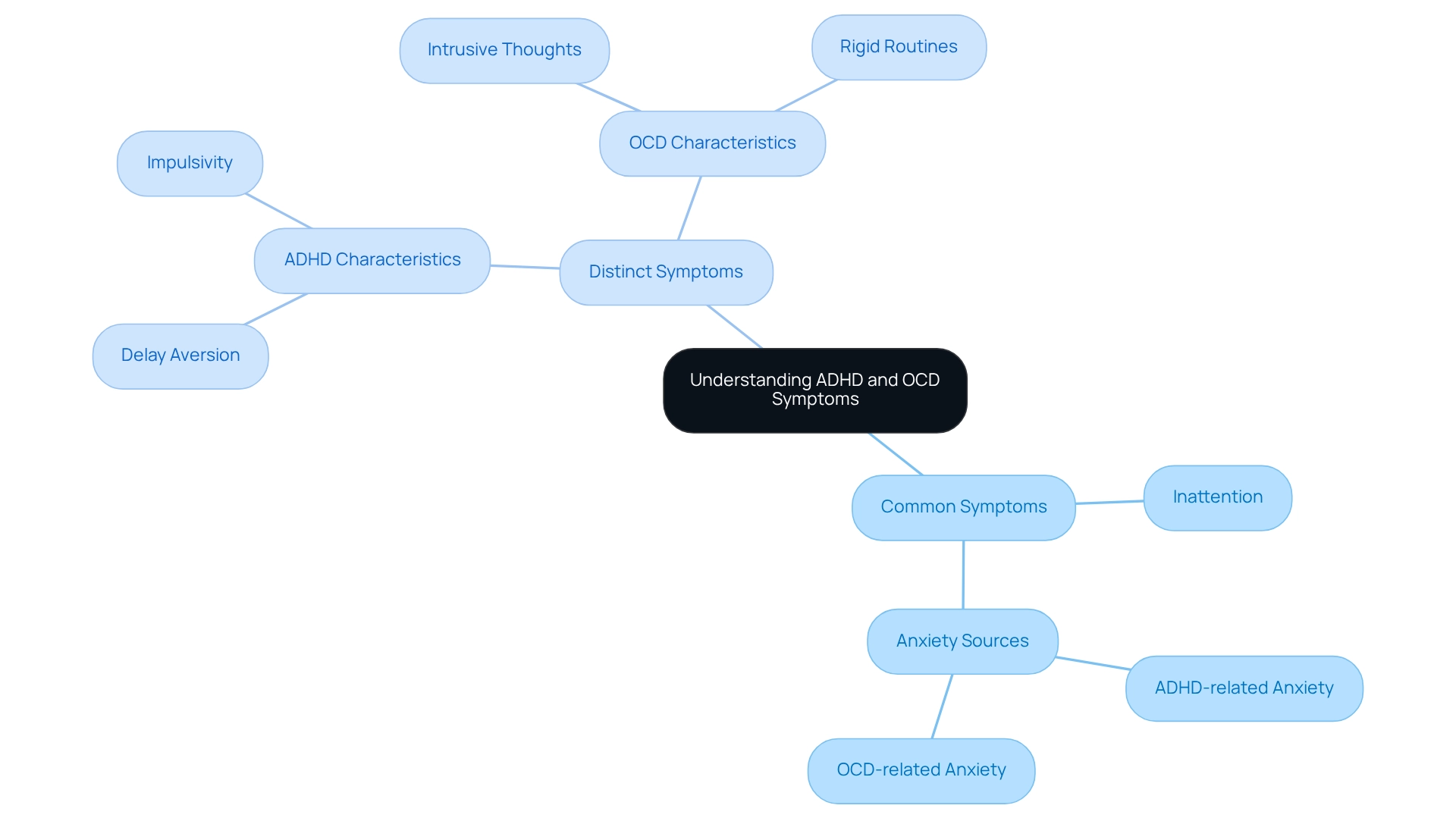
Common Symptoms: Overlaps and Distinctions
ADHD and OCD symptoms can present overlapping issues, particularly inattention and concentration difficulties. For many parents, it’s heartbreaking to see their children struggle with these challenges. Children identified with attention deficit hyperactivity disorder often find it difficult to maintain focus on tasks, leading to feelings of frustration and anxiety. In contrast, youngsters with OCD may become absorbed in intrusive thoughts, diverting them from their activities.
While both conditions can induce anxiety, the sources of this anxiety differ significantly. ADHD-related anxiety typically arises from the challenges associated with attention deficits, whereas OCD-related anxiety is rooted in the distress caused by obsessive thoughts and compulsive behaviors.
Recent studies indicate that a notable percentage of children experience symptoms of both ADHD and OCD, highlighting the importance of understanding their co-occurrence. For instance, research on serotonergic genes has shown that while there are genetic overlaps between attention disorders and OCD, specific genes, such as HTR2A, are more closely linked to OCD. This complexity underscores the need for parents to recognize the distinct characteristics of each condition.
Children with attention deficit hyperactivity disorder may also demonstrate 'Delay Aversion,' where they choose smaller rewards to evade waiting. This behavior can further complicate their decision-making processes. Expert insights reveal that the nature of rituals can also help differentiate between the two disorders. Individuals with OCD typically follow rigid routines, while those with attention difficulties may struggle with detailed tasks and display impulsivity.
As Amitai Abramovitch, PhD, observes, "In contrast to individuals with attention deficit hyperactivity disorder from adolescence, those with OCD are seldom impulsive and do not demonstrate risk-taking behavior." Grasping these subtleties is essential for guardians as they manage their children's symptoms and pursue suitable interventions. By acknowledging the distinctions and commonalities between ADHD and OCD symptoms, caregivers can more effectively advocate for their children and obtain the essential support and resources they need.
Differentiating Between ADHD and OCD Symptoms
To effectively distinguish between attention deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD), it’s essential for parents to closely observe the context and nature of their child's symptoms. ADHD symptoms, such as impulsivity and hyperactivity, often appear consistently across various settings. You might notice behaviors like frequent interruptions during conversations or difficulty remaining seated. In contrast, OCD symptoms tend to be more situational, characterized by compulsions that arise in response to specific obsessions.
For instance, a child with OCD may find themselves repeatedly checking locks or performing rituals due to an overwhelming fear of potential harm. Understanding these distinctions is crucial for parents, especially regarding ADHD and OCD symptoms, as misdiagnosis can significantly affect treatment outcomes. Recent studies indicate that misdiagnosis rates for ADHD and OCD can be as high as 30%, highlighting the importance of careful observation and accurate assessment.
Moreover, a study examining gender ratios in samples of ADHD and OCD emphasizes that the increased occurrence of ADHD in males may artificially inflate the likelihood of identifying such cases within OCD samples. This underscores the need for careful attention to gender ratios in future research. As Andrew G. Guzick from the University of Florida notes, 'When OCD symptomology clearly precedes attention problems, it may be useful to take a 'response-to-intervention' approach to diagnosing ADHD in this population.' By recognizing these nuances, caregivers can seek appropriate support and interventions tailored to their child's unique needs.
At ASD Media, we are committed to fostering collaboration and growth in the ABA therapy industry, providing valuable resources for parents and professionals as they navigate these complex conditions. We encourage you to share your experiences and seek support, as you are not alone on this journey.
The Risks of Misdiagnosis: Understanding ADHD and OCD
Misdiagnosis of ADHD and OCD symptoms poses significant risks, often leading to inappropriate treatment plans that can worsen the symptoms. For instance, when a child is incorrectly identified as having attention deficit hyperactivity disorder, they may be prescribed stimulant medications, which can further exacerbate both ADHD and OCD symptoms. Conversely, a child with OCD might only receive treatment for anxiety, neglecting the crucial compulsive behaviors at play. Recent discussions among healthcare professionals underscore the importance of considering impulsivity and risk-taking behaviors as diagnostic elements, as these traits can help differentiate between ADHD and OCD.
As Amitai Abramovitch, PhD and Research Fellow at the OCD and Related Disorders Program at Massachusetts General Hospital, notes, "Unlike those with attention deficit hyperactivity disorder from adolescence, individuals with OCD are very rarely impulsive and do not display risk-taking behavior."
A case study titled 'Neurobiology of Attention Deficit Hyperactivity Disorder and OCD' reveals both shared and disorder-specific brain dysfunctions, illustrating how different neurobiological processes can lead to similar executive function deficits. This highlights the critical need for accurate diagnosis, as misdiagnosis can significantly impact treatment outcomes. The findings suggest that while ADHD and OCD symptoms share common neuropsychological impairments, they also display unique dysfunctions in specific brain regions, reinforcing the concept of an impulsive–compulsive continuum.
Moreover, expert opinions emphasize the necessity for further research into effective treatment strategies for individuals exhibiting symptoms of both ADHD and OCD. Behavioral therapy has shown promising success rates for ADHD; however, its effectiveness may be compromised if the underlying OCD is not properly addressed. Parents are encouraged to pursue comprehensive evaluations from qualified professionals to ensure their child receives the correct diagnosis and a tailored treatment plan. This approach ultimately fosters better outcomes and enhances quality of life.
This discussion is particularly timely, especially in light of the ADDitude Expert Webinar on OCD that aired on February 11, 2021, which highlighted the ongoing need for awareness and research in this important field.
Effective Treatment Strategies for ADHD and OCD
Navigating the complexities of ADHD and OCD can be challenging for both children and their parents. Effective treatment typically involves a multifaceted approach that combines behavioral therapy, medication, and parent training. Behavioral interventions play a crucial role in helping children improve their organizational skills and regulate impulses, particularly for those with attention deficit hyperactivity disorder. When it comes to OCD, Cognitive Behavioral Therapy (CBT) is recognized as the gold standard, especially with its focus on Exposure and Response Prevention (ERP).
This method empowers children to gradually confront their fears while learning to resist compulsive behaviors, fostering resilience and essential coping strategies.
Recent studies highlight the importance of personalized treatment strategies, particularly when ADHD and OCD symptoms coexist. For instance, a study examining the comorbidity of these disorders in Japanese adults revealed notable differences in clinical features and treatment outcomes between those with both conditions and those with OCD alone. This underscores the necessity for tailored interventions that address the unique challenges each disorder presents.
In practice, it’s vital for parents to collaborate closely with healthcare providers to develop a customized treatment plan that effectively addresses their child's ADHD and OCD symptoms. Current best practices advocate for interventions that are not only evidence-based but also adaptable to the individual’s specific needs. For example, an intervention program that ran for seven consecutive weeks focused on establishing routines, organizing environments, enhancing time management, and developing stress management skills, all tailored to the individual goals of participants.
As our understanding of these disorders evolves, ongoing research remains essential. Experts emphasize the need for further investigation into the neurobiological interactions between ADHD and OCD to enhance treatment options and improve outcomes. As noted by JK, "Further research is needed to better understand the neurobiological interplay between both disorders, refine our nosology of them, and guide treatment options."
By staying informed about the latest developments and actively participating in the treatment process, parents can significantly influence their child’s journey toward managing these complex conditions. Your involvement matters, and together, we can pave the way for a brighter future.
The Role of Tailored Therapy and Support Systems
Customized therapeutic strategies are essential for effectively managing ADHD and OCD symptoms, as they cater to the unique needs of each individual. Individualized treatment plans must consider specific symptoms, family dynamics, and the educational environment. Child psychologists emphasize that a one-size-fits-all approach falls short; instead, personalized strategies can significantly enhance outcomes.
For instance, recent studies indicate that children aged 6–12 who receive customized interventions show marked improvements in managing their symptoms. As Laurie noted, "He was determined to help my son have a better life than he did and he gave me great insight," highlighting the transformative impact of tailored therapy.
Support systems play a pivotal role in this process. Parent training programs and support groups offer invaluable resources and foster community connections. Interacting with other guardians facing similar challenges not only provides practical guidance but also nurtures a sense of inclusion and mutual understanding.
This emotional support is vital, as working caregivers have reported reduced anxiety levels when they are part of a supportive network, underscoring the importance of these connections.
Real-life examples illustrate the effectiveness of these support systems. For example, a case study titled 'Building Deep Friendships Through Shared Experiences' emphasizes how caregivers of children with special needs often experience isolation. By participating in support groups, they can forge meaningful friendships and connections, enriching their parenting journeys.
The benefits of such networks are underscored by statistics indicating that caregivers involved in support groups report higher satisfaction and lower stress levels.
In 2025, the introduction of educational programs co-led by user representatives and health professionals will further enhance understanding of ADHD diagnosis, treatment, and parenting challenges. These initiatives will focus on customized therapy methods, ensuring that guardians are equipped with the knowledge and resources necessary to support their children effectively. Ultimately, the importance of personalized treatment for ADHD and OCD cannot be overstated, as it lays the foundation for better management of symptoms and improved quality of life for both children and their families.
Building a Supportive Community: Resources for Parents
Establishing a nurturing community is vital for caregivers navigating the complexities of attention deficit hyperactivity disorder and obsessive-compulsive disorder. Access to resources like local support groups, online forums, and educational workshops can greatly enhance the experience for parents, offering both valuable information and emotional support. Organizations such as CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) and the International OCD Foundation play a crucial role in providing resources, advocacy, and opportunities for community connection.
Statistics reveal that approximately 22% of adolescents have engaged in yoga over the past year, pointing to a growing interest in holistic approaches that can complement traditional therapies for managing symptoms of ADHD and OCD. Participating in practices like yoga can foster mindfulness and emotional control, which are beneficial for young individuals facing these challenges. By engaging with these resources, parents can share their experiences, learn from others, and alleviate feelings of isolation.
As James F. Leckman, M.D., from the Child Study Center at Yale University School of Medicine, notes, "In contrast, individuals with OCD along with attention deficit hyperactivity disorder lived in families with notably higher levels of family dysfunction than did the unaffected comparison subjects." This highlights the emotional hurdles families encounter and the necessity of a strong support network. Case studies indicate that children diagnosed with both ADHD and OCD symptoms often experience heightened emotional difficulties.
For example, research shows that the OCD-plus-ADHD group displayed significantly more emotional impairment compared to other diagnostic groups, reinforcing the importance of community resources.
In 2025, fostering a supportive community for caregivers of individuals with ADHD and OCD remains a priority. Engaging with local support groups not only offers a platform for sharing strategies but also cultivates a sense of belonging among families facing similar challenges. This collaborative environment empowers parents to advocate effectively for their children, ensuring they receive the essential support and resources to thrive.
Conclusion
Understanding ADHD and OCD is essential for parents navigating the complexities of childhood behavioral issues. This article sheds light on the key characteristics of both disorders, highlighting that ADHD is defined by inattention and impulsivity, whereas OCD is marked by intrusive thoughts and compulsive behaviors. Recognizing these distinctions is crucial, as misdiagnosis can lead to inappropriate treatment and exacerbate symptoms, underscoring the need for accurate assessments.
The overlapping symptoms of ADHD and OCD can complicate diagnosis. Parents are encouraged to observe the context of their child's behaviors. ADHD symptoms tend to be consistent across various settings, while OCD symptoms are often situational. This nuanced understanding empowers parents to advocate effectively for their children, ensuring they receive appropriate interventions tailored to their unique needs.
Effective treatment strategies for ADHD and OCD embrace a multifaceted approach, including behavioral therapy, medication, and parent training. Collaboration between parents and healthcare providers is vital in developing individualized treatment plans. Additionally, the role of community support is invaluable; access to resources, support groups, and educational programs can greatly enhance the parenting experience and foster resilience.
As our understanding of these disorders continues to evolve, ongoing research and community engagement remain critical. By fostering a supportive network and utilizing available resources, parents can empower themselves and their children, paving the way for improved management of ADHD and OCD. Ultimately, this effort enhances the quality of life for the entire family.
Frequently Asked Questions
What is Attention-Deficit/Hyperactivity Disorder (ADHD)?
ADHD is characterized by enduring patterns of inattention, hyperactivity, and impulsivity. Key traits include difficulty sustaining attention, excessive fidgeting, and impulsive decision-making.
How does the occurrence of ADHD vary by race among individuals aged 12–17 years?
The occurrence of ADHD among individuals aged 12–17 years is 17.0% for White individuals, 13.0% for Black individuals, and 11.7% for Hispanic individuals.
Are children aged 5–11 years more or less likely to experience ADHD compared to those aged 12–17 years?
Children aged 5–11 years are less likely to experience ADHD than those aged 12–17 years across all family income levels.
What is Obsessive-Compulsive Disorder (OCD)?
OCD is defined by the presence of obsessions, which are intrusive thoughts that provoke anxiety, and compulsions, which are repetitive behaviors performed to alleviate that anxiety. Children with OCD may engage in specific rituals, such as excessive handwashing or checking behaviors.
What is the relationship between ADHD and OCD symptoms?
Recent studies indicate that children can display symptoms of both ADHD and OCD, and those with both may be at an increased risk of developing further OCD symptoms. The interaction between the two can complicate diagnosis and treatment.
How does family income influence the occurrence of ADHD?
A case study shows that children from households under the federal poverty threshold have an occurrence rate of 14.8% for ADHD, which drops to 10.1% for those at or above 200% of the federal poverty threshold, suggesting socioeconomic factors may influence the manifestation of ADHD.
What are the differences in anxiety sources between ADHD and OCD?
ADHD-related anxiety typically arises from challenges associated with attention deficits, while OCD-related anxiety is rooted in distress caused by obsessive thoughts and compulsive behaviors.
What is "Delay Aversion" in children with ADHD?
Delay Aversion refers to a tendency where children with ADHD choose smaller rewards to avoid waiting, complicating their decision-making processes.
How can caregivers differentiate between ADHD and OCD symptoms?
Caregivers can differentiate by noting that individuals with OCD typically follow rigid routines, while those with ADHD may struggle with detailed tasks and display impulsivity. Additionally, children with ADHD are more likely to be impulsive and engage in risk-taking behavior compared to those with OCD.




