Overview
This article aims to shed light on the understanding and management of ADHD-related compulsive behavior, highlighting the importance of recognizing symptoms and implementing effective treatment strategies. It draws attention to the connection between ADHD and compulsive behaviors, acknowledging the challenges that come with diagnosis.
Furthermore, it emphasizes the necessity for comprehensive management approaches, which include:
- Behavioral therapy
- Medication
- Robust support systems for families
These elements are crucial in promoting better outcomes for individuals affected by these conditions. By fostering awareness and providing targeted resources, we can create a supportive environment that encourages healing and growth.
Introduction
In a world where attention spans are shrinking and distractions abound, understanding Attention-Deficit/Hyperactivity Disorder (ADHD) is more important than ever. This neurodevelopmental disorder, marked by persistent inattention, hyperactivity, and impulsivity, impacts millions, including a substantial number of adults.
As awareness of ADHD increases, so does the recognition of its complexities, especially when it intersects with compulsive behaviors and conditions like Obsessive-Compulsive Disorder (OCD). This article invites you to explore the multifaceted nature of ADHD, highlighting its symptoms, the challenges of diagnosis, and the intricate relationship with compulsive behaviors.
By examining effective management strategies and the significance of support systems, we aim to empower families and professionals to navigate the complexities of ADHD with deeper understanding and compassion.
Defining ADHD: Symptoms and Characteristics
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition that many parents and professionals encounter, characterized by persistent patterns of inattention, hyperactivity, and impulsivity. Key symptoms often include:
- Difficulty maintaining focus in tasks or play activities.
- Frequent careless errors in schoolwork or other activities.
- Struggles in arranging tasks and activities.
- Fidgeting or tapping hands or feet.
- Interrupting or intruding on others.
Recognizing these symptoms is essential for effectively identifying ADHD and navigating its associated challenges. Recent research reveals that ADHD impacts a significant portion of the population, with estimates suggesting that approximately 16.13 million adults in the U.S. have the condition, as noted by Jill Johnson. Moreover, a striking statistic indicates that 51.2% of individuals over 50 are likely to receive a diagnosis of ADHD, highlighting the condition's commonality among older adults.
In 2021, it was emphasized that care for minors aged 3–17 is primarily overseen by primary care providers, with nurse practitioners and psychiatric nurses playing essential roles. However, disparities exist, particularly for children on Medicaid, who are less likely to access specialized care. This situation underscores the importance of various healthcare specialists in providing comprehensive management of ADHD.
Looking ahead to 2025, an impressive 98% of adults with the condition are expected to recognize beneficial attributes linked to it, including creativity and empathy. This shift in perception highlights the importance of understanding ADHD not merely as a collection of difficulties but also as a wellspring of distinctive abilities. Current webinars have addressed crucial topics such as speech therapy in ADHD management and the spread of misinformation related to the condition, emphasizing the need for accurate information and support.
In summary, understanding the symptoms and traits of ADHD is vital for promoting effective management strategies and enhancing outcomes for individuals impacted by this condition. By acknowledging both the challenges and the unique benefits of ADHD, parents and professionals can better assist those navigating this complex disorder. Sharing experiences and seeking support can make a meaningful difference in this journey.
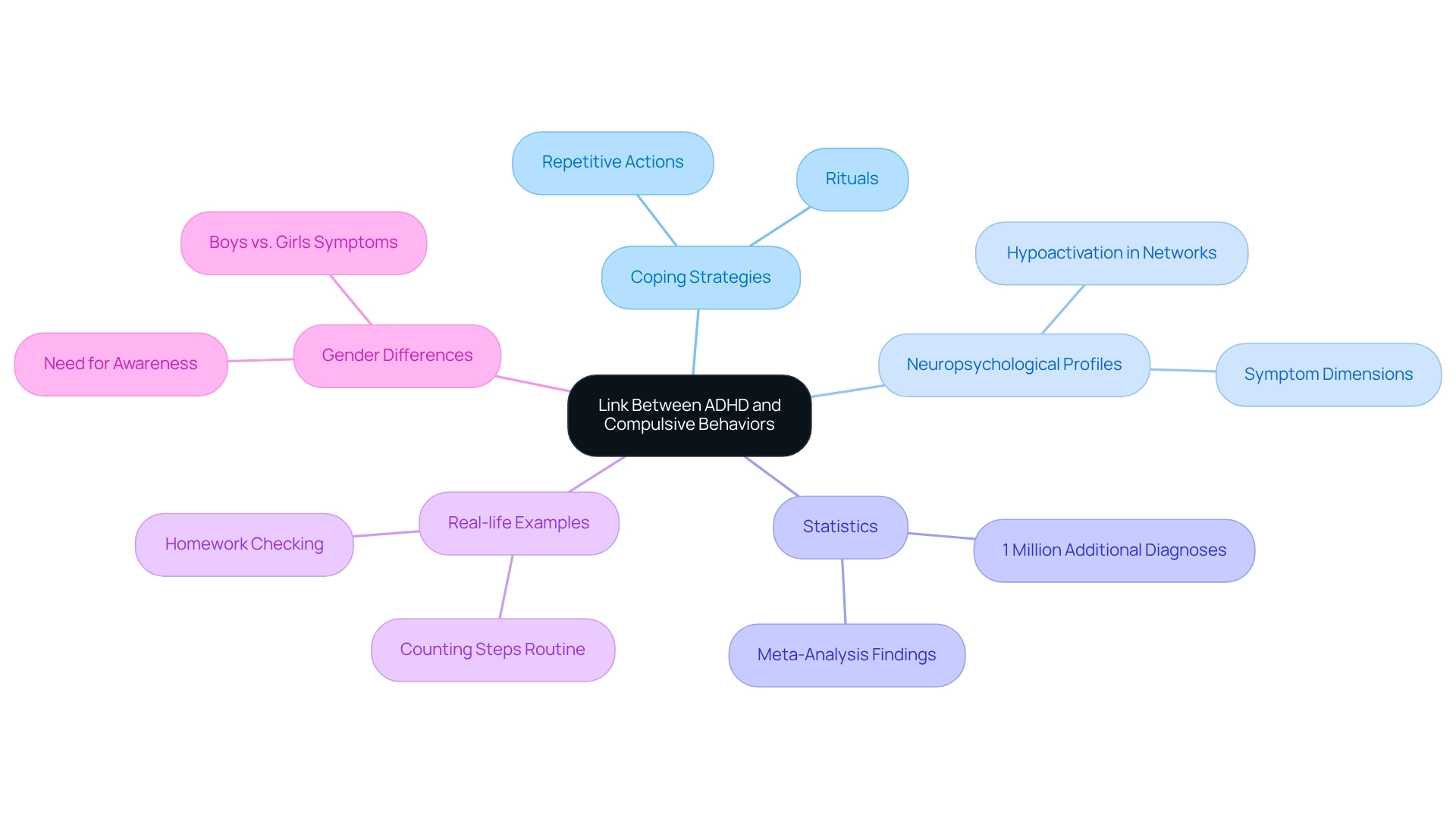
The Link Between ADHD and Compulsive Behaviors
Studies suggest a notable link between attention deficit hyperactivity disorder (ADHD) and compulsive behavior, which individuals may adopt as coping strategies to manage impulsivity or anxiety. These patterns often manifest as repetitive actions or rituals that provide temporary relief from discomfort. For instance, a child with ADHD might repeatedly check their homework or meticulously organize their desk to ease feelings of chaos or anxiety.
This tendency is not merely a quirk; it reflects underlying neuropsychological profiles that vary based on symptom dimensions in both ADHD and compulsive behavior. Recent studies have highlighted that individuals with ADHD often experience hypoactivation in fronto-parietal executive function networks, contributing to ADHD compulsive behavior. Understanding this neuropsychological element is essential in comprehending how ADHD presents and influences actions.
In 2022, Danielson ML reported that an additional 1 million U.S. youth aged 3-17 years had received a diagnosis of ADHD compared to 2016, underscoring the growing acknowledgment of this condition and its complexities. Real-life examples illustrate how compulsive actions can serve as strategies for managing symptoms of this disorder. For example, a young person may establish a routine of counting steps before entering a room, helping them feel more in command of their surroundings. Understanding these actions is crucial for creating effective intervention strategies that address both ADHD and compulsive behavior.
Furthermore, case studies indicate gender differences in the expression of ADHD symptoms, with boys frequently exhibiting more pronounced behaviors like hyperactivity, while girls may demonstrate more understated compulsive tendencies. This disparity emphasizes the necessity for heightened awareness and understanding of how ADHD manifests differently among genders, ensuring that all children receive appropriate diagnosis and support. By acknowledging the connection between ADHD and compulsive behavior, parents and experts can more effectively tailor their strategies to promote positive outcomes.
Challenges in Diagnosing ADHD with Compulsive Behaviors
Diagnosing attention deficit hyperactivity disorder (ADHD) can be particularly challenging, especially when ADHD compulsive behavior is involved. These behaviors often closely resemble the symptoms of obsessive-compulsive disorder (OCD), leading to potential misdiagnoses that can have significant implications for treatment outcomes. Research indicates concerning rates of misdiagnosis for both ADHD and OCD, highlighting disparities particularly among minoritized groups. Many individuals in these groups frequently experience underdiagnosis, despite exhibiting elevated symptom rates.
This underrecognition is compounded by racial and gender biases, which call for a more equitable approach to diagnosis and treatment. To accurately differentiate between ADHD and OCD, clinicians must conduct thorough evaluations that include behavioral assessments and detailed interviews with parents and teachers. Such comprehensive assessments are crucial, as misdiagnosis can result in ineffective treatment plans, complicating the management of both conditions.
In 2025, the focus on overdiagnosis by healthcare professionals has created additional barriers to care, especially for individuals with ADHD and OCD. This underscores the necessity for a holistic approach to patient treatment. Statistics reveal that situational factors accounted for 2.0% of non-responses among primary respondents in the National Comorbidity Survey Replication (NCS-R). This statistic emphasizes the complexities involved in gathering accurate diagnostic information, which is essential for effective treatment.
Expert insights suggest that broader inquiries can yield more comprehensive information, enabling clinicians to explore the nuances of each case more thoroughly—particularly when distinguishing between ADHD and OCD. Case studies illustrate the real-world consequences of these diagnostic challenges. For instance, research on disparities in ADHD diagnosis shows that Black individuals and girls often face significant obstacles in obtaining appropriate diagnoses, even when they display symptoms that warrant attention. This highlights the urgent need for awareness and training among healthcare providers to recognize and address these biases, ensuring that all individuals receive fair treatment.
In conclusion, the overlap between ADHD and ADHD compulsive behavior presents unique diagnostic challenges that require careful consideration and a commitment to equitable treatment practices. By fostering a deeper understanding of these complexities, parents and professionals can navigate the intricacies of ADHD management more effectively. Encouraging open dialogue and sharing experiences can further enhance the support network for those affected.
Understanding Comorbidity: ADHD and OCD
The co-occurrence of attention deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD) presents significant challenges for families navigating these conditions. For many individuals grappling with both disorders, symptoms can worsen, leading to heightened impulsivity and compulsive behaviors. For instance, a child diagnosed with ADHD might resort to compulsive checking as a coping mechanism for their inattention, illustrating the complex interplay between these two conditions.
Recent studies reveal that the rates of comorbidity between ADHD and OCD are notably high. Some estimates suggest that up to 30% of individuals with ADHD also exhibit symptoms of OCD. This statistic can be alarming for parents, highlighting the need for vigilance and understanding.
Research has raised critical concerns about the methodologies used in studies examining ADHD-OCD comorbidity, particularly regarding gender biases and recruitment practices. A case study titled "Methodological Concerns in ADHD-OCD Research" pointed out significant biases, urging for more representative samples and careful consideration of confounding factors. Addressing these issues is essential for validating the co-occurrence of these disorders and enhancing our understanding, especially among adults.
The latest findings underscore the importance of comprehensive studies, particularly within community samples, to shed light on the developmental trajectory and treatment implications of ADHD-OCD comorbidity. Parents may find comfort in knowing that ongoing research aims to improve understanding and support.
Expert opinions suggest that the distinct characteristics of ADHD and OCD symptoms merit further investigation to ensure accurate diagnosis. The Executive Overload Model proposes that certain ADHD symptoms in individuals with OCD may actually reflect behavioral expressions of OCD-related neurocognitive deficits. As Dr. Amitai Abramovitch notes, this perspective highlights the need for tailored treatment strategies that address both disorders simultaneously, ultimately improving outcomes for those affected by this intricate relationship.
Additionally, the Yale Brown Obsessive Compulsive Scale (Y-BOCS), which scores from 0 to 40, offers a quantitative measure for understanding OCD severity in individuals with ADHD. This tool emphasizes the necessity for nuanced approaches in treatment, ensuring that families receive the support they need.
If you or someone you know is navigating the complexities of ADHD and OCD, consider reaching out for professional guidance. Sharing experiences and seeking support can make a world of difference.
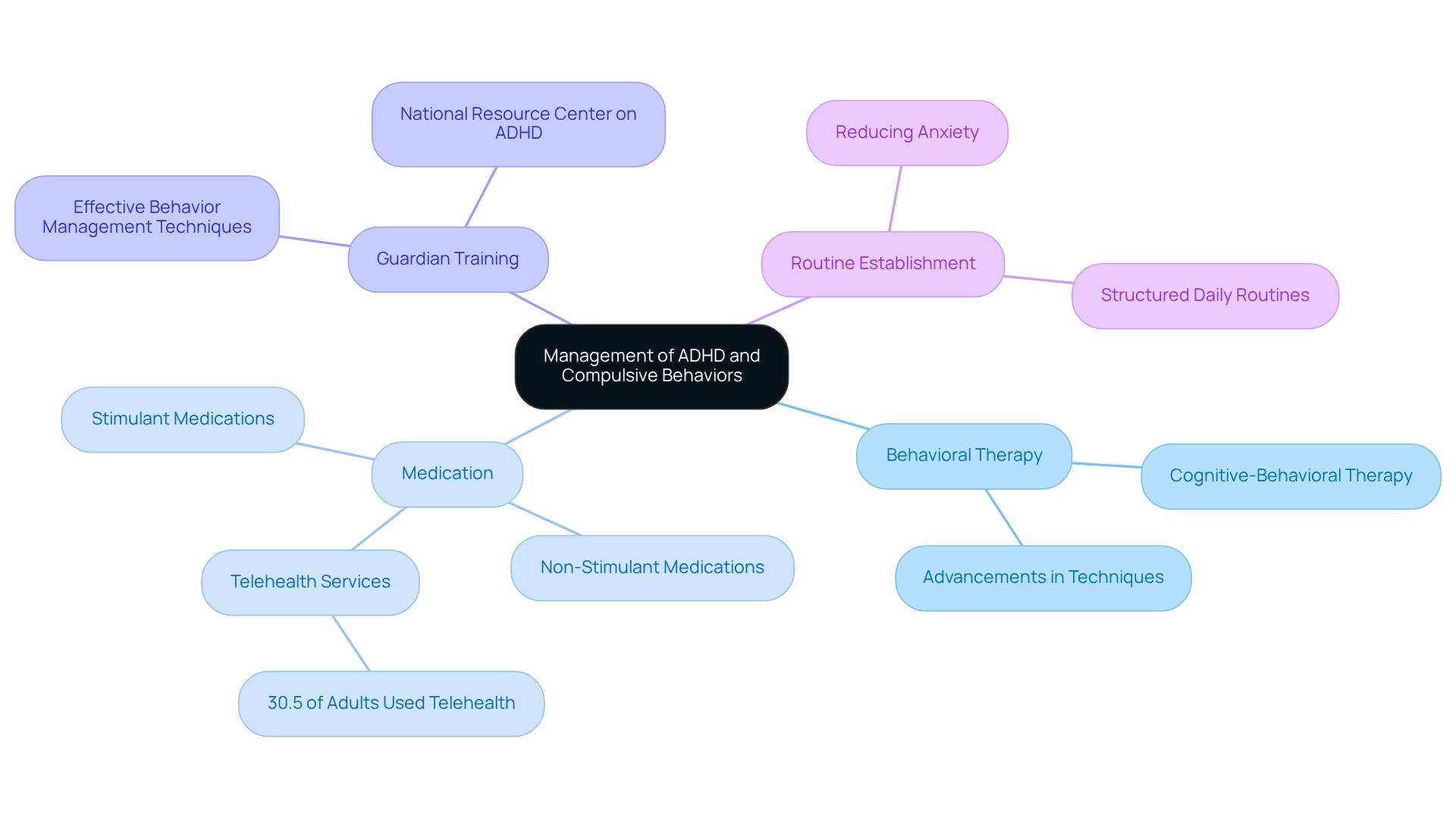
Effective Treatment Strategies for ADHD and Compulsive Behaviors
Managing ADHD and compulsive behaviors requires a compassionate, multifaceted approach that can truly make a difference in the lives of children and their families.
- Behavioral Therapy: Structured behavioral interventions are essential in helping children learn to manage their symptoms. Techniques like cognitive-behavioral therapy (CBT) have shown success in reducing impulsivity and ADHD-related compulsive behaviors, enabling children to develop crucial coping strategies. Recent advancements in behavioral therapy techniques have further enhanced their effectiveness in 2025. As Magnus W. poignantly observes, "Still, without treatment, the individuals continue to deteriorate and eventually end up in financial, legal, and social difficulties," underscoring the urgent need for effective management strategies.
- Medication: Both stimulant and non-stimulant medications play a vital role in alleviating symptoms of attention deficit hyperactivity disorder, which can also help reduce compulsive behaviors. Statistics indicate that many adults with ADHD have utilized telehealth services for prescriptions, highlighting the growing accessibility of medication management since March 2020. This trend emphasizes the importance of medication as part of a comprehensive treatment plan. However, noncompliance with medications remains a common challenge in ADHD management, making ongoing support and education essential.
- Guardian Training: Educating guardians on effective behavior management techniques is crucial. Training programs empower parents to implement strategies that support their child's development, fostering a collaborative environment that enhances treatment outcomes. The National Resource Center on Attention Deficit Hyperactivity Disorder is an invaluable resource, offering evidence-based information and support for families navigating these challenges. This resource is particularly important considering that the lifetime prevalence of ADHD among U.S. adolescents aged 13 to 18 years is 8.7%, with nearly half of all cases exhibiting severe impairment.
- Routine Establishment: Establishing regular daily routines can significantly benefit individuals with ADHD. A structured environment helps them feel more secure, reducing anxiety and, in turn, lessening behaviors associated with ADHD compulsive behavior. By integrating routine into daily life, parents can create a predictable framework that supports their child's emotional and behavioral needs.
Together, these strategies form a comprehensive approach to managing attention deficit hyperactivity disorder and its related compulsive behaviors, ultimately enhancing the quality of life for affected individuals and their families. Your journey in supporting your child is important, and these strategies can help pave the way for a brighter future.
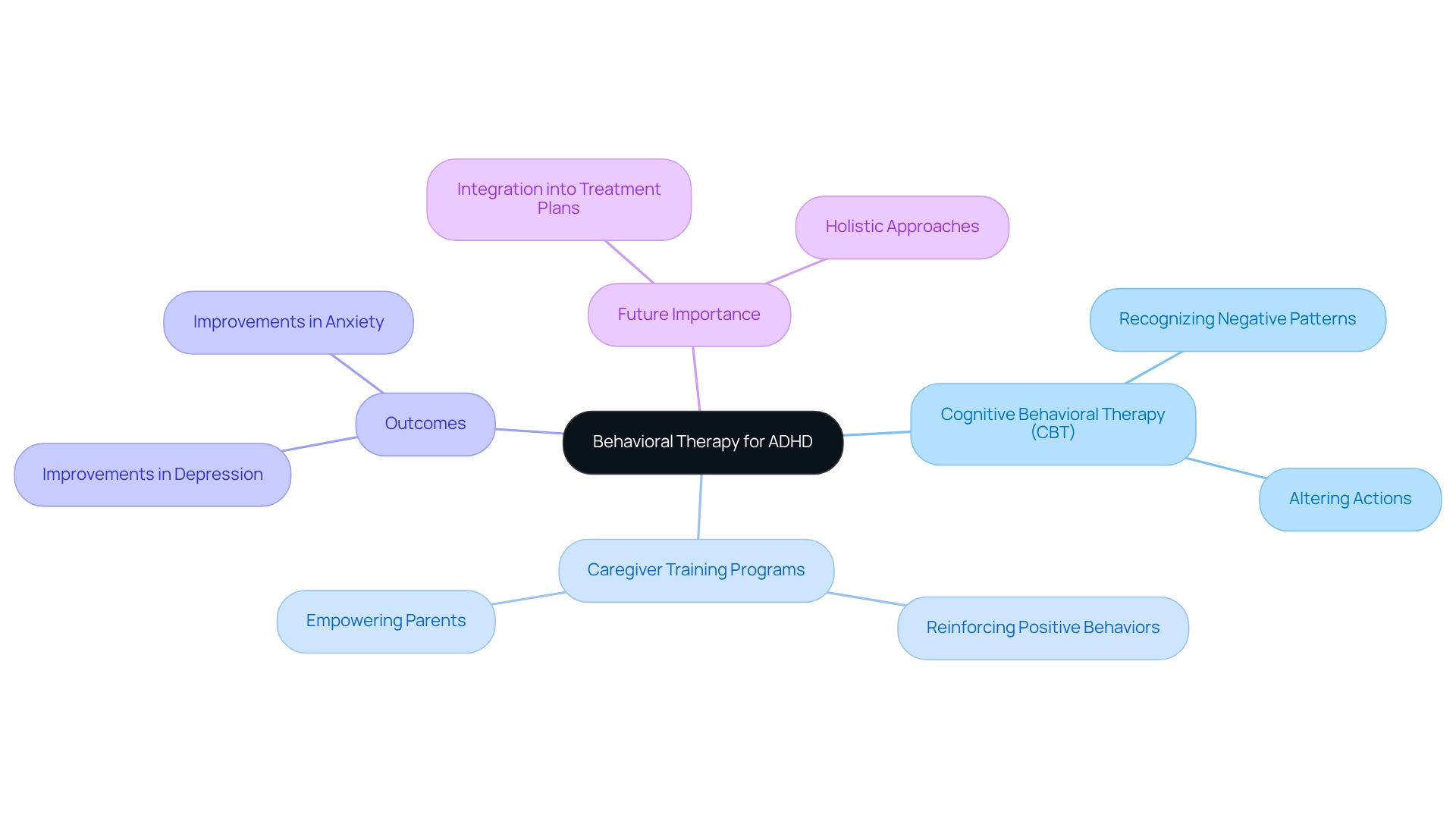
The Role of Behavioral Therapy in Managing ADHD
Behavioral therapy plays a vital role in the treatment of attention deficit hyperactivity disorder (ADHD) and its associated compulsive behaviors. Methods such as Cognitive Behavioral Therapy (CBT) have proven effective in helping individuals recognize and alter negative thought patterns and actions. A meta-analysis, which included both controlled and uncontrolled studies, revealed that CBT has a moderate effect size compared to other non-pharmacological treatments for ADHD, underscoring its significance in symptom management.
Moreover, caregiver training programs are essential in equipping guardians with effective strategies to reinforce positive behaviors and directly address challenges. These programs not only empower parents but also foster a supportive environment that encourages behavioral modification. For instance, research titled "Secondary Outcomes of CBT" indicates that individuals engaged in CBT reported notable improvements in self-reported depression and anxiety—common emotional concerns associated with ADHD.
As we look ahead to 2025, the importance of behavioral therapy is increasingly emphasized by experts in the field, who advocate for its integration into comprehensive treatment plans. By focusing on behavioral change, individuals with ADHD can develop effective coping strategies to manage compulsive behaviors, ultimately enhancing their ability to manage symptoms and improve their overall quality of life. This holistic approach not only addresses the primary symptoms of ADHD but also promotes emotional well-being, establishing it as a cornerstone of effective management.
As highlighted by ASD Media, empowering caregivers and professionals with effective strategies for managing difficult behaviors and enhancing social skills development is crucial in this journey. Together, we can create a nurturing environment that supports both individuals with ADHD and their families.
Building Support Systems for Parents and Caregivers
Creating a strong support network is vital for guardians and caregivers of children with ADHD. This support can take various forms that are essential for navigating the challenges faced.
- Support Groups: Participating in local or online support groups enables parents to connect with others who face similar challenges. These groups provide a platform for sharing experiences, exchanging insights, and fostering a sense of community. In 2025, the significance of these groups is highlighted by the fact that they not only reduce feelings of isolation but also empower caregivers with practical strategies for managing ADHD-related behaviors. As Maya Rathnasabapathy poignantly expressed, "I worry for myself; no one can look after my offspring if I am not there." That is my biggest fear of my life.
- Professional Resources: Collaborating with professionals such as therapists, educators, and behavioral specialists can offer invaluable guidance. These specialists can assist guardians in navigating the intricacies of attention disorders, offering customized approaches that cater to unique requirements. For example, recent statistics show that 80 percent of youngsters with attention deficit hyperactivity disorder receive school-based assistance, 40 percent undergo social-skills training, 31 percent engage in caregiver training, and 20 percent receive cognitive behavioral therapy, emphasizing the essential role of educational professionals in a young person's development.
- Educational Workshops: Participating in workshops centered on attention deficit hyperactivity disorder provides guardians with crucial information and efficient techniques to assist their children. These workshops frequently address a variety of subjects, from behavioral management strategies to comprehending the subtleties of attention deficit hyperactivity disorder and its coexisting conditions, including ADHD compulsive behavior. Engaging in continuous learning helps parents feel more confident and capable in their caregiving roles.
Real-world examples illustrate the effectiveness of these support systems. For instance, a case study analyzing the influence of media exposure on attention deficit hyperactivity disorder outcomes showed that greater media consumption is linked to intensified symptoms of the condition. This discovery highlights the necessity for knowledgeable parenting approaches, which can be cultivated through involvement in support groups and workshops, aiding in reducing the impacts of media exposure on attention deficit hyperactivity disorder symptoms.
The benefits of these support systems are profound. They not only offer emotional support but also cultivate resilience among caregivers, empowering them to better advocate for their offspring. The ongoing pressure of raising a child with attention deficit hyperactivity disorder can result in physical health problems for mothers, further highlighting the importance of a robust support network to cope with ADHD compulsive behavior.
By building these connections, parents can mitigate this stress, ultimately enhancing their own well-being and that of their children.
Empowering Families: Proactive Management of ADHD
Enabling families to take a proactive stance in handling attention deficit hyperactivity disorder (ADHD) and its associated compulsive behaviors is vital for promoting positive outcomes. This can be accomplished through several essential strategies:
- Education: Providing families with thorough information about ADHD is crucial. Understanding the condition helps clarify its implications and reduces stigma, which is particularly important given the substantial societal misunderstandings surrounding ADHD. As highlighted by Cross River Therapy, despite the prevalence of ADHD, a significant level of stigma still exists.
- Skill Development: Teaching young individuals effective coping strategies and self-regulation methods is essential. These skills not only enhance their ability to manage symptoms independently but also foster resilience in the face of challenges. Programs like the Improving Parenting Skills Adult Attention Deficit Hyperactivity Disorder (IPSA) have shown promising outcomes, with caregivers reporting improved child-rearing abilities and high participation rates (an average attendance of 84% of sessions). This suggests the viability of such initiatives. Comparisons from pre-to-post evaluations indicated positive changes in targeted parenting skills, highlighting the need for further evaluation in a randomized controlled trial.
- Open Communication: Creating an environment of open dialogue within the family is fundamental. Encouraging young individuals to express their needs and challenges nurtures a supportive atmosphere where understanding and empathy can flourish. This approach not only strengthens family bonds but also empowers youngsters to advocate for themselves. It's important to recognize that 62.5% of parents reported experiencing some form of detrimental, potentially harmful event during the study, underscoring the challenges families face in managing ADHD.
By implementing these strategies, families can cultivate a supportive environment that significantly enhances their ability to address attention deficits and ADHD compulsive behaviors, ultimately leading to better outcomes for children. Engaging therapists who specialize in ADHD and fostering strong parent-therapist relationships further reinforces these efforts, ensuring families receive the support they need to navigate the complexities of ADHD effectively.
Conclusion
Understanding ADHD and its interplay with compulsive behaviors is essential for fostering effective management and support for those affected. This article delves into the symptoms and characteristics of ADHD, emphasizing the importance of recognizing its presence in both children and adults. The prevalence of ADHD, particularly among older adults, highlights the need for comprehensive awareness and appropriate intervention strategies.
The connection between ADHD and compulsive behaviors underscores the complexity of diagnosis and treatment. Misdiagnosis remains a challenge, especially when symptoms overlap with those of Obsessive-Compulsive Disorder (OCD). Acknowledging these intricacies is vital for healthcare providers to ensure equitable and effective treatment for all individuals, regardless of their background.
Moreover, this article outlines effective management strategies, including:
- Behavioral therapy
- Medication
- Parent training
These collectively contribute to improved outcomes for individuals with ADHD. Establishing robust support systems for families is equally important, providing emotional relief and practical strategies to navigate the challenges of ADHD.
Ultimately, empowering families through education, skill development, and open communication fosters a proactive approach to managing ADHD. By embracing both the challenges and strengths associated with ADHD, parents and professionals can create nurturing environments that enhance the quality of life for affected individuals. Understanding and compassion are key in navigating the complexities of this disorder, paving the way for positive outcomes and a brighter future for those living with ADHD.
Frequently Asked Questions
What is Attention-Deficit/Hyperactivity Disorder (ADHD)?
ADHD is a neurodevelopmental condition characterized by persistent patterns of inattention, hyperactivity, and impulsivity.
What are the key symptoms of ADHD?
Key symptoms of ADHD include difficulty maintaining focus, frequent careless errors in tasks, struggles in organizing activities, fidgeting or tapping, and interrupting others.
How prevalent is ADHD in the population?
Approximately 16.13 million adults in the U.S. have ADHD, with 51.2% of individuals over 50 likely to receive a diagnosis.
Who primarily oversees the care for children with ADHD?
Care for minors aged 3–17 is primarily overseen by primary care providers, with significant roles played by nurse practitioners and psychiatric nurses.
What disparities exist in ADHD care for children on Medicaid?
Children on Medicaid are less likely to access specialized care for ADHD, highlighting the need for various healthcare specialists in managing the condition.
What shift in perception regarding ADHD is expected by 2025?
By 2025, it is expected that 98% of adults with ADHD will recognize beneficial attributes linked to the condition, such as creativity and empathy.
What recent topics have been addressed in webinars about ADHD?
Webinars have focused on topics like speech therapy in ADHD management and the spread of misinformation related to the condition.
How is compulsive behavior related to ADHD?
Compulsive behavior may be adopted as coping strategies to manage impulsivity or anxiety in individuals with ADHD, manifesting as repetitive actions or rituals.
What recent findings relate to ADHD and compulsive behavior?
Studies indicate that individuals with ADHD often experience hypoactivation in executive function networks, which contributes to compulsive behavior.
What gender differences exist in the expression of ADHD symptoms?
Boys typically exhibit more pronounced hyperactive behaviors, while girls may show more understated compulsive tendencies, emphasizing the need for awareness in diagnosis and support.




