Overview
Caring for a child with OCD comorbidity and ADHD can feel overwhelming, but understanding the unique characteristics and interactions of both disorders is a crucial first step. Did you know that approximately 21% of youth with OCD also exhibit ADHD symptoms? This overlap can complicate both diagnosis and treatment, making it essential for parents to be informed and proactive.
Effective management involves tailored treatment strategies, such as cognitive-behavioral therapy and medication. Early intervention is vital, and collaboration among caregivers can significantly support your child's development and well-being. Remember, you are not alone in this journey—connecting with other parents facing similar challenges can provide invaluable support.
Consider reaching out to professionals or support groups that specialize in these disorders. Together, we can create a nurturing environment that fosters growth and resilience in our children.
Introduction
Navigating the complexities of childhood mental health can feel overwhelming, particularly when two disorders intersect in a child's life. Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) often co-occur, presenting a unique set of challenges that complicate both diagnosis and treatment.
With symptoms such as intrusive thoughts, compulsive behaviors, inattention, and impulsivity, the overlapping characteristics of these conditions can create confusion for parents and healthcare providers alike. As research continues to shed light on the prevalence and interplay between OCD and ADHD, understanding their key traits becomes essential for effective intervention.
This article explores the defining features of each disorder, the impact of their comorbidity, and the strategies that can empower families to successfully navigate these challenges together.
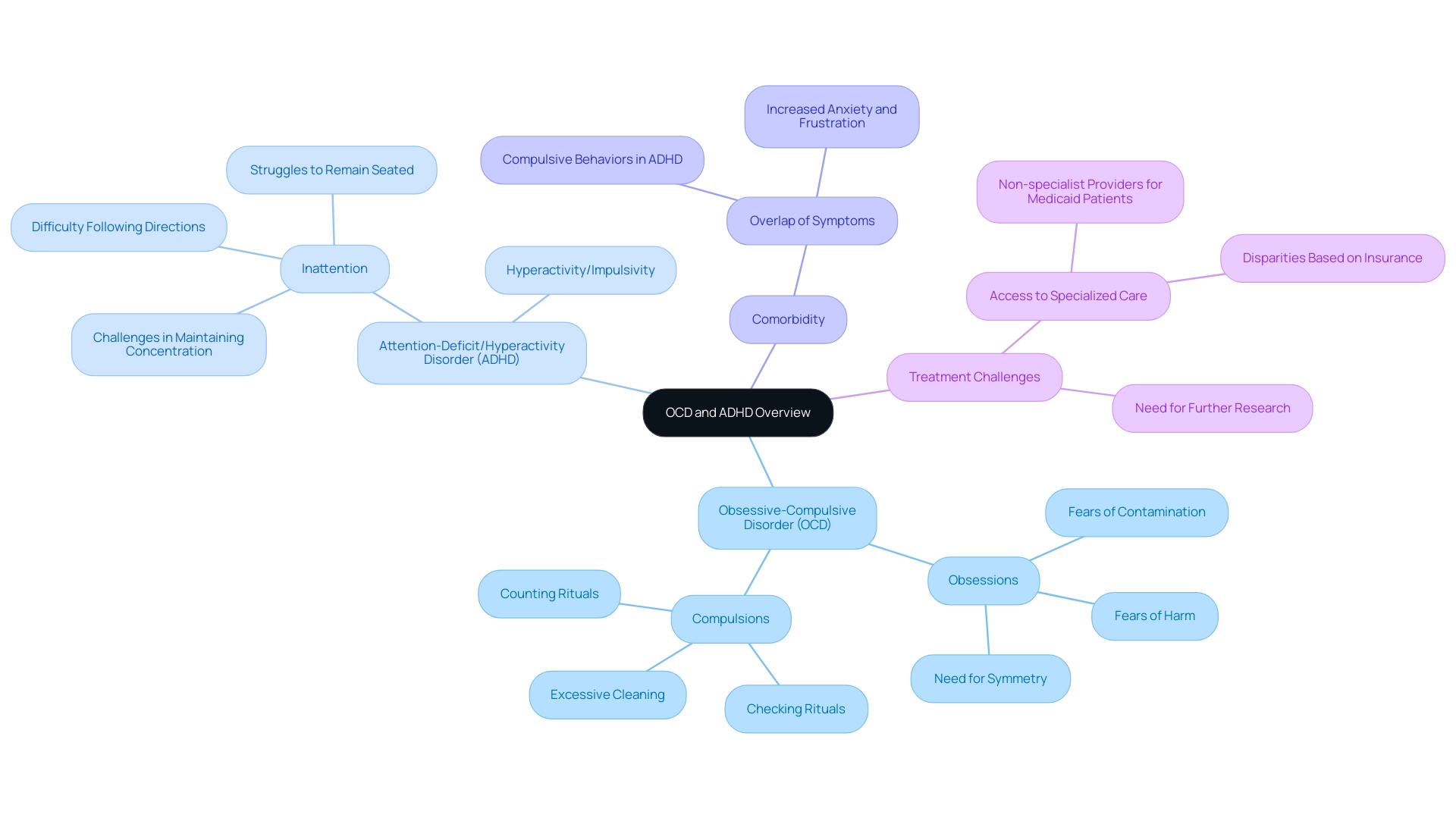
Defining OCD and ADHD: Key Characteristics and Symptoms
Obsessive-Compulsive Disorder (OCD) reveals itself through persistent, intrusive thoughts known as obsessions, coupled with repetitive behaviors or mental acts called compulsions. Common obsessions often revolve around fears of contamination, harm, or the need for symmetry. In contrast, compulsions may include excessive cleaning, checking, or counting rituals. Meanwhile, Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by a pattern of inattention, hyperactivity, and impulsivity.
Children with ADHD frequently encounter challenges in maintaining concentration, following directions, and remaining seated. These difficulties can lead to significant academic and social hurdles, leaving both children and their families feeling overwhelmed.
Understanding the interaction between these two disorders is crucial. Studies suggest that the incidence of ADHD has increased over the years, with notable rises since the 1950s, a time marked by the standardization of educational systems. By 2025, it is estimated that many youth diagnosed with ADHD will also demonstrate OCD comorbidity, complicating their treatment and management.
Experts emphasize the importance of recognizing the overlapping symptoms associated with OCD comorbidity in young individuals. For instance, children with attention issues may exhibit compulsive behaviors resembling OCD, such as repetitive actions or rituals, which can exacerbate their challenges. A recent examination of healthcare claims data from 2021 revealed that many young patients receiving ADHD treatment were managed by primary care providers, highlighting disparities in access to specialized care based on insurance categories.
This situation underscores the need for further investigation into effective treatment approaches for youth with OCD comorbidity and ADHD. Many youths on Medicaid received care from non-specialist providers, indicating potential gaps in access to specialized treatment for attention disorders.
Real-world examples illustrate the complexities faced by young individuals diagnosed with both disorders. A child exhibiting symptoms of OCD comorbidity with ADHD may grapple with impulsivity while feeling compelled to perform certain rituals. This struggle can lead to heightened anxiety and frustration. As Magnus W. poignantly noted, "Still, without treatment, individuals continue to deteriorate and eventually face financial, legal, and social difficulties."
As we move forward, understanding the key traits and signs of OCD and ADHD will be vital in developing effective interventions and support systems for affected youth. Together, we can foster a nurturing environment that addresses their unique needs and challenges.
The Prevalence of Comorbidity: Understanding the Intersection of OCD and ADHD
Research shows that the comorbidity of OCD and ADHD in youth is significant, with approximately 21% of individuals diagnosed with OCD also exhibiting symptoms of ADHD. Conversely, the prevalence of ADHD among youth with OCD can reach as high as 25.5%. This overlap complicates both diagnosis and treatment, as the symptoms of one disorder can obscure or intensify those of the other.
For clinicians, a thorough assessment approach is essential to identify both conditions, ensuring that children receive the comprehensive care they need. Impulsivity, in particular, may serve as a significant indicator of this comorbidity.
A noteworthy study titled "Impact of Childhood Attention Deficit Hyperactivity Disorder Symptoms on OCD in Adults" sheds light on this issue. It examines the prevalence of childhood ADHD symptoms in adults diagnosed with OCD. Conducted from February 2018 to February 2019 with 100 OCD patients aged 18-45, the study found that 44% had a history of childhood attention deficit symptoms. Those exhibiting both childhood and current adult ADHD symptoms reported higher levels of depression, anxiety, and impulsivity.
Even individuals whose childhood ADHD symptoms did not persist into adulthood displayed more severe OCD symptoms and greater comorbid anxiety and depression. These findings underscore the importance of understanding the interaction between OCD and ADHD, especially in young individuals.
As Menije Boduryan-Turner, PsyD, points out, "OCD greatly affects a person’s life due to intrusive thoughts, anxiety, and uncertainty." As research continues to evolve, it is crucial for parents and professionals to stay informed about the latest statistics and insights regarding these comorbidities, particularly as we approach 2025.
While there is no cure for OCD, symptoms can be managed through psychotherapy, medication, or both. Understanding these dynamics can significantly enhance the efficacy of interventions and support strategies for those affected. If you find yourself navigating these challenges, know that support is available, and you are not alone on this journey.
Shared Symptoms: How OCD and ADHD Interact and Overlap
The presence of OCD comorbidity with ADHD can profoundly impact a youth's ability to concentrate and focus, often leading to confusion in both diagnosis and treatment. For instance, a child with attention deficit hyperactivity disorder may struggle to maintain attention on tasks, while a child with OCD may become overwhelmed by obsessive thoughts, resulting in distraction. This dynamic can create a frustrating cycle where the compulsive behaviors linked to OCD interfere with the impulsivity typical of ADHD.
Recent statistics show that misdiagnosis is a common concern, as overlapping symptoms can result in unsuitable approaches, such as stimulant medications that may worsen OCD symptoms. Experts stress the importance of a tailored approach, especially in cases of OCD comorbidity with ADHD. For example, a combined treatment plan incorporating SSRIs for OCD and stimulants for ADHD may prove beneficial, with many individuals noticing improvements from SSRIs within eight to 12 weeks.
However, careful monitoring is essential due to the complex interactions between these medications. Psychologists specializing in youth emphasize that recognizing the unique manifestations of each disorder can lead to more accurate diagnoses and better outcomes for children facing these challenges. Amitai Abramovitch, a neuropsychologist, highlights that, unlike individuals with ADHD, those with OCD are rarely impulsive and do not engage in risk-taking behavior.
By fostering teamwork among caregivers, educators, and healthcare professionals, we can create a supportive environment that meets the intricate needs of youth with OCD comorbidity and ADHD. This collaborative approach aligns with ASD Media's mission to enhance the implementation of ABA therapy and improve outcomes for children. Together, we can make a difference in the lives of these young individuals and their families.
Diagnostic Challenges: Differentiating Between OCD and ADHD
Differentiating between OCD and attention deficit hyperactivity disorder (ADHD), particularly when OCD coexists with ADHD, can be quite challenging due to their overlapping symptoms, especially concerning attention-related difficulties. While both disorders may present attention issues, it’s important to recognize that their underlying causes are distinct. For instance, individuals with OCD typically do not exhibit the impulsivity that is a hallmark of ADHD.
This distinction is crucial for accurate diagnosis and aligns with ASD Media's mission to empower parents and professionals in understanding these complexities. Clinicians are encouraged to conduct thorough evaluations that encompass behavioral assessments and interviews with parents and teachers. Such comprehensive approaches are essential for effectively identifying the presence of one or both disorders. Additionally, it is vital to rule out other conditions that may present similarly, including anxiety disorders and learning disabilities.
Statistics indicate that around 15% of adults with OCD report mild impairment, underscoring the significance of precise diagnosis and care. Misdiagnosis can lead to unsuitable care strategies, which may exacerbate symptoms. For example, a case study on age-specific approaches for ADHD highlights the necessity of customized strategies; behavior therapy is suggested as the primary option for children under 6, while a combination of behavior therapy and medication is recommended for those aged 6 and older. This illustrates the practical implications of accurate diagnosis in creating effective care plans.
Experts in the field, such as Amitai Abramovitch, PhD, emphasize the need for clinicians to examine key diagnostic factors to establish a more accurate diagnosis. He states, "We recommend that clinicians examine two major diagnostic factors that may aid in establishing a more accurate diagnosis." This insight is particularly relevant in light of the evolving understanding of these disorders, including OCD comorbidity with ADHD and the associated challenges.
By addressing these diagnostic challenges, clinicians can better support individuals navigating the complexities of OCD and ADHD. If you’re a parent or professional seeking to understand these conditions more deeply, consider reaching out for resources or support that can guide you through this journey.
Treatment Strategies: Managing Comorbid OCD and ADHD in Children
Effectively managing OCD comorbidity with ADHD and attention deficit disorder requires a multifaceted treatment approach tailored to the unique needs of each child. Cognitive-behavioral therapy (CBT), particularly exposure and response prevention (ERP), has emerged as a cornerstone in treating OCD, demonstrating significant efficacy in reducing symptoms. For attention deficit hyperactivity disorder, behavioral interventions combined with medication can effectively alleviate symptoms, allowing for improved functioning in daily life.
A comprehensive pharmacotherapy plan often includes:
- Selective serotonin reuptake inhibitors (SSRIs) for OCD, which help regulate mood and anxiety.
- Stimulant medications that enhance focus and attention.
This dual approach addresses the complexities of both disorders. Recent studies indicate that OCD comorbidity with ADHD significantly influences clinical features and treatment outcomes in adults.
Collaboration among therapists, parents, and educators is essential in creating a supportive environment that fosters the child's development. For instance, a study involving 93 adult patients with OCD comorbidity with ADHD revealed notable differences in clinical features between those with and without attention deficit hyperactivity disorder. This highlights the importance of tailored interventions. Specifically, the study found that patients with attention deficit hyperactivity disorder characteristics exhibited distinct clinical profiles, which required personalized care approaches.
Furthermore, prospective comparisons of treatment outcomes over six months indicated that responses varied significantly based on the presence of attention deficit hyperactivity disorder, underscoring the need for individualized approaches.
Statistics indicate that almost 1 in 5 youth with Medicaid received attention deficit hyperactivity disorder care from nurse practitioners and psychiatric nurses. This reflects the increasing acknowledgment of the necessity for specialized support in managing OCD comorbidity with ADHD. As CN noted, "Effective management through psychotherapy, medication, or a combination of both can lead to significant improvements in quality of life for young individuals facing these challenges." Real-world examples of effective CBT for youth with OCD demonstrate the potential for positive outcomes when interventions are appropriately applied.
As we approach 2025, ongoing research and case studies will continue to inform best practices and enhance treatment strategies for young individuals facing these challenges.
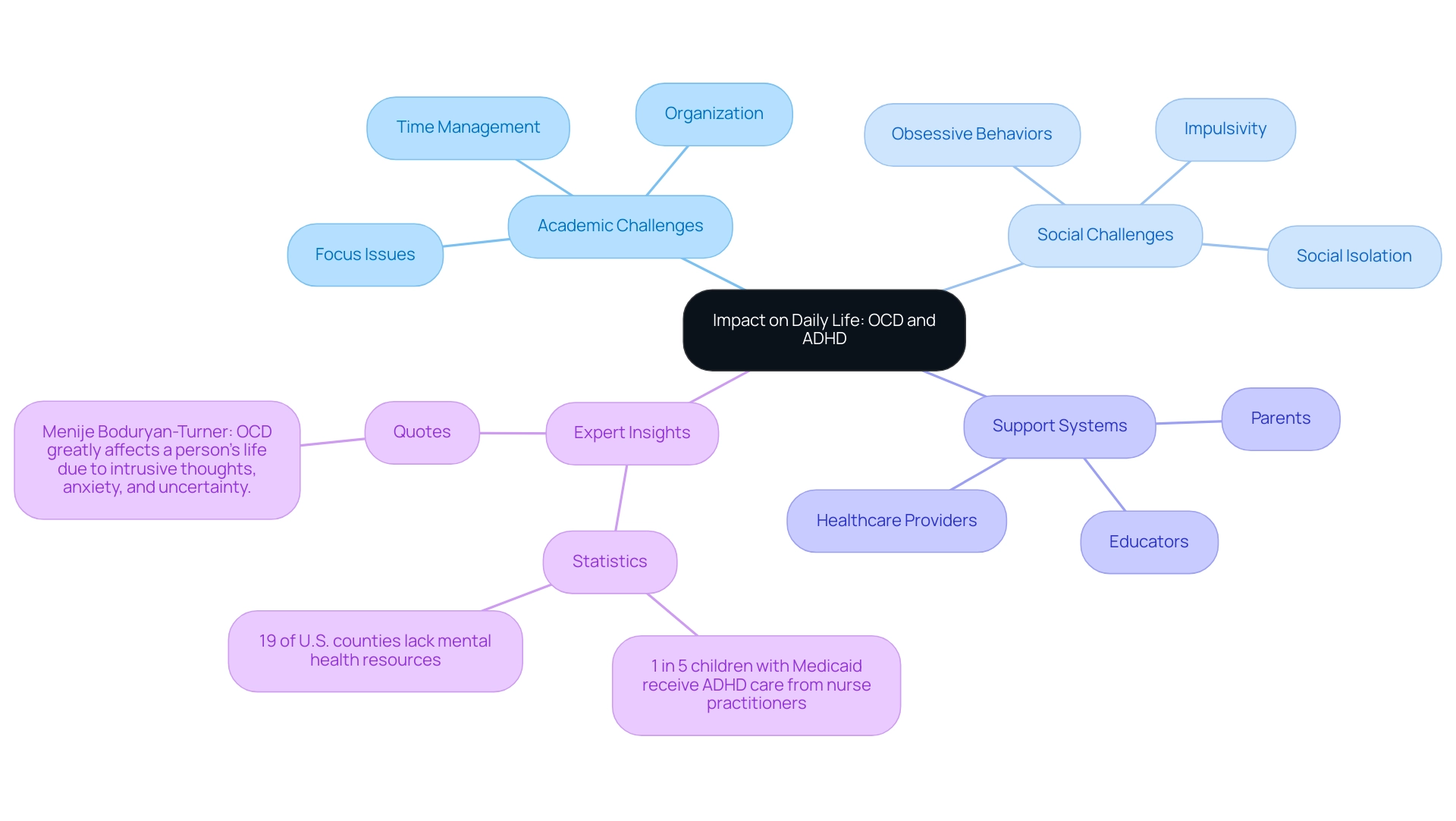
Impact on Daily Life: Navigating Challenges with OCD and ADHD
Children grappling with the dual challenges of OCD often face profound difficulties in their everyday lives. These struggles can significantly hinder academic performance, as research indicates that students with OCD often wrestle with focus, organization, and time management—skills essential for success in school. For example, nearly 1 in 5 youngsters receiving Medicaid care for ADHD are treated by nurse practitioners and psychiatric nurses, highlighting the critical need for comprehensive support systems within educational settings.
Moreover, it’s crucial to recognize that 19% of U.S. counties lack adequate mental health resources, further exacerbating the challenges these young individuals encounter.
Social interactions are equally affected, as children may exhibit impulsivity or obsessive behaviors that can alienate their peers. This social isolation can intensify feelings of anxiety and uncertainty, complicating their ability to form meaningful relationships. Statistics indicate that by 2025, youth with OCD will face increased challenges in both academic and social spheres, underscoring the need for a cooperative strategy between parents and educators.
As Dr. Menije Boduryan-Turner poignantly notes, "OCD greatly affects a person’s life due to intrusive thoughts, anxiety, and uncertainty," emphasizing the significant impact these conditions have on daily functioning. To cultivate an environment that fosters success, it is essential for parents and educators to collaborate in creating structured settings that promote effective coping strategies. Real-life examples illustrate the academic and social hurdles these individuals face, such as difficulties in group projects or challenges in maintaining friendships due to their symptoms.
Additionally, a case study on healthcare providers for attention deficit hyperactivity disorder treatment highlights the essential role of primary care clinicians in managing these conditions, with many young patients receiving care from pediatricians. Expert opinions stress the importance of customized interventions that cater to the specific needs of youth with OCD comorbidity ADHD, ensuring they receive the necessary support to thrive both academically and socially. Furthermore, research suggests that low serotonin synthesis capacity may contribute to OCD, providing insight into the biological factors at play.
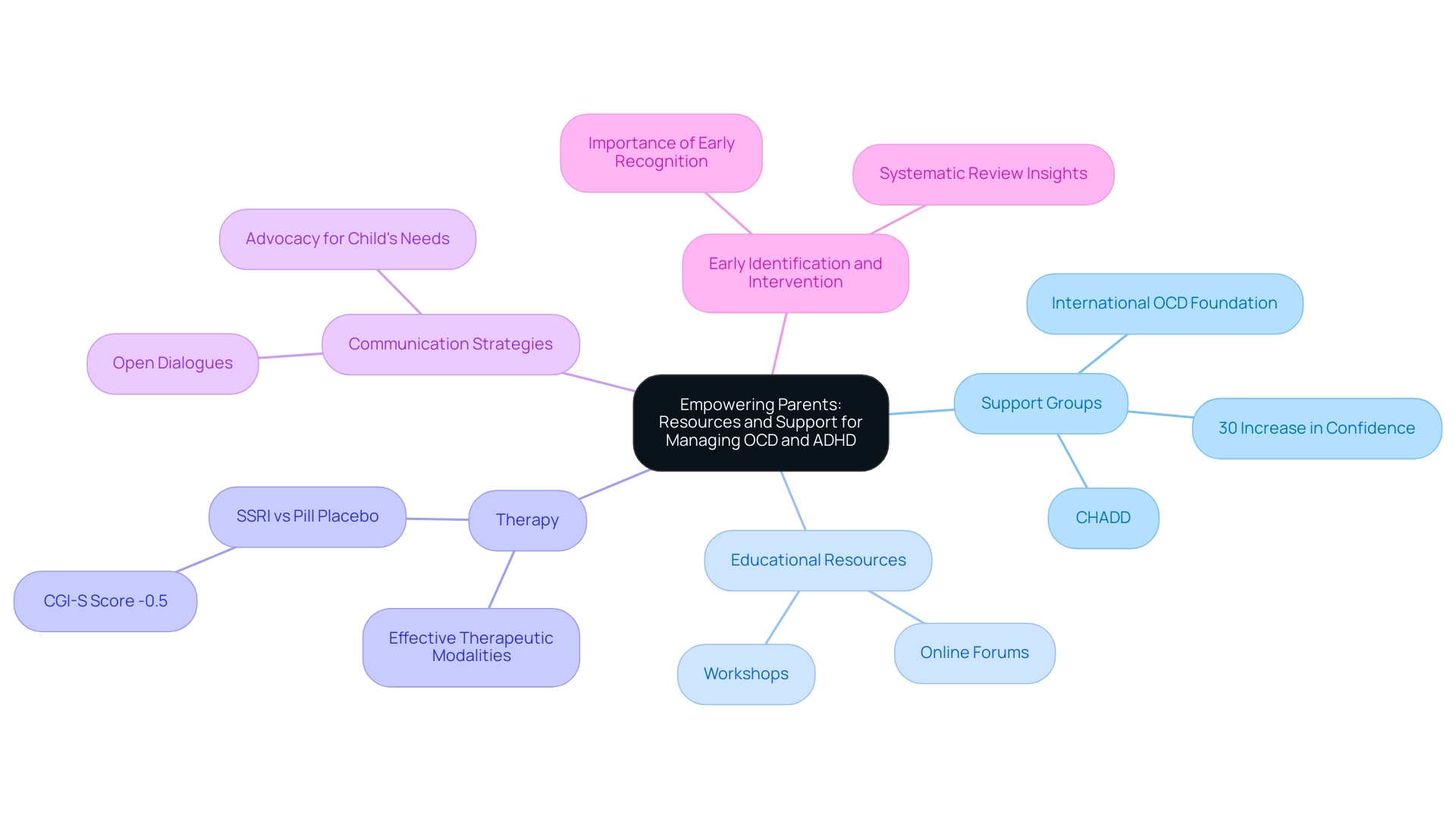
Empowering Parents: Resources and Support for Managing OCD and ADHD
Parents play a crucial role in navigating the complexities of OCD comorbidity with ADHD in their children. By engaging with support groups, utilizing educational resources, and accessing therapy, they can significantly enhance their ability to manage these conditions effectively. Organizations like the International OCD Foundation and CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) offer tailored resources specifically designed for families facing these challenges.
Recent statistics reveal that participation in support groups can lead to improved outcomes for families. For instance, studies show that parents involved in organized support networks report a 30% increase in their confidence when managing their child's symptoms. These groups not only provide emotional support but also share practical strategies that have proven effective in real-world situations.
Moreover, effective communication strategies are essential for parents to engage meaningfully with their children and healthcare professionals. By fostering open dialogues, parents can better advocate for their child's needs, ensuring they receive appropriate interventions. Resources such as workshops and online forums can equip parents with the skills necessary to navigate these important conversations.
As we look to 2025, the emphasis on early identification and intervention remains critical. A systematic review highlighted the importance of recognizing OCD comorbidity with ADHD symptoms early to prevent long-term developmental disruptions. This underscores the need for parents to be vigilant and proactive in seeking help. The review also assessed the comparative effects and harms of intervention strategies for OCD in youngsters and teenagers, emphasizing the necessity of effective therapeutic modalities.
Additionally, the pooled estimate for SSRI versus pill placebo in CGI-S score was reported as -0.5, indicating a significant impact that parents should consider when exploring options for managing their child's symptoms. By leveraging available resources and support systems, parents can create a nurturing environment that fosters their child's growth and well-being. Dr. Adam, who contributed to the systematic review, emphasized the importance of early identification and effective intervention, reinforcing the need for parents to utilize these insights in their advocacy efforts.
Transparency is also crucial; the systematic review acknowledged funding from AHRQ and PCORI, ensuring that parents are aware of the sources behind the recommendations they follow.
Future Directions: Emerging Research and Treatment Opportunities for OCD and ADHD
Recent studies are shedding light on the neurobiological connections between OCD and attention deficit hyperactivity disorder (ADHD), revealing that overlapping brain pathways may significantly impact treatment outcomes. For instance, emerging research indicates that nearly 15.8 million adults with ADHD are beginning to recognize the positive aspects of their condition, such as creativity and empathy. These insights can inform therapeutic approaches for children facing similar challenges. As Jill Johnson, a coach specializing in ADHD, shares, "As a coach specializing on this topic, I believe the future is bright."
This perspective highlights the potential for positive outcomes in treatment. Furthermore, in 2021, many young individuals received ADHD treatment from primary care providers, with nearly half of privately insured youth and about 1 in 4 Medicaid recipients obtaining care from a pediatrician. Significantly, almost 1 in 5 young individuals with Medicaid received ADHD treatment from nurse practitioners and psychiatric nurses, emphasizing the range of care options available.
Innovative therapies, including mindfulness-based interventions and digital therapeutics, are currently being explored for their potential effectiveness in alleviating symptoms of disorders such as OCD and ADHD. It is important to note that while there is no cure for OCD, symptoms can be managed through psychotherapy, medication, or a combination of both. As these treatment modalities gain traction, it becomes increasingly vital for parents and professionals to stay informed about the latest findings and therapeutic options.
This knowledge can empower caregivers to make informed decisions that enhance the care and support provided to children with OCD and ADHD comorbidity, ultimately fostering a more nurturing environment for their development.
Conclusion
Navigating the intersection of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) can be daunting for children and their families. The overlapping symptoms of these disorders often complicate diagnosis and treatment, making it vital for parents and healthcare providers to grasp their distinct characteristics. With a notable percentage of children diagnosed with OCD also exhibiting ADHD symptoms, and vice versa, recognizing and addressing this comorbidity is crucial.
Effective management calls for a multifaceted approach that includes evidence-based therapies, such as Cognitive-Behavioral Therapy (CBT), alongside appropriate medication. Collaboration among parents, educators, and healthcare professionals is essential in fostering a supportive environment tailored to each child's unique needs. By nurturing open communication and utilizing available resources, families can navigate the complexities of these disorders more effectively.
As research continues to evolve, staying informed about the latest findings and treatment options empowers parents and caregivers to advocate for their children. Emphasizing early identification and intervention can significantly enhance outcomes, allowing children to flourish academically and socially despite the challenges posed by OCD and ADHD. Ultimately, a proactive and informed approach will enrich the quality of life for those affected, paving the way for brighter futures.
Frequently Asked Questions
What are the main characteristics of Obsessive-Compulsive Disorder (OCD)?
OCD is characterized by persistent, intrusive thoughts known as obsessions, and repetitive behaviors or mental acts called compulsions. Common obsessions include fears of contamination, harm, or the need for symmetry, while compulsions may involve excessive cleaning, checking, or counting rituals.
How is Attention-Deficit/Hyperactivity Disorder (ADHD) defined?
ADHD is characterized by a pattern of inattention, hyperactivity, and impulsivity. Children with ADHD often struggle to maintain concentration, follow directions, and remain seated, leading to significant academic and social challenges.
What is the relationship between OCD and ADHD in youth?
Studies indicate a significant comorbidity between OCD and ADHD in youth, with approximately 21% of individuals diagnosed with OCD also exhibiting ADHD symptoms, and up to 25.5% of youth with ADHD showing symptoms of OCD. This overlap complicates both diagnosis and treatment.
Why is it important to recognize the overlapping symptoms of OCD and ADHD?
Recognizing overlapping symptoms is crucial because children with attention issues may display compulsive behaviors similar to OCD, which can worsen their challenges. Understanding these interactions can help in developing effective treatment strategies.
What are the implications of the increase in ADHD diagnoses since the 1950s?
The rise in ADHD diagnoses may be linked to the standardization of educational systems. By 2025, many youth diagnosed with ADHD are expected to also demonstrate OCD comorbidity, complicating their treatment and management.
What gaps exist in the treatment of youth with OCD and ADHD?
Many youths on Medicaid receive care from non-specialist providers, indicating potential gaps in access to specialized treatment for attention disorders. This situation highlights the need for further investigation into effective treatment approaches.
How do the symptoms of ADHD and OCD affect treatment?
The symptoms of one disorder can obscure or intensify those of the other, making it essential for clinicians to conduct thorough assessments to identify both conditions and ensure comprehensive care.
What recent findings have been made regarding childhood ADHD symptoms and OCD in adults?
A study found that 44% of adults with OCD had a history of childhood ADHD symptoms. Those with both childhood and current ADHD symptoms reported higher levels of depression, anxiety, and impulsivity.
What are the treatment options for OCD?
While there is no cure for OCD, symptoms can be managed through psychotherapy, medication, or a combination of both. Understanding the dynamics of OCD and ADHD can enhance the efficacy of interventions and support strategies.
What should parents and professionals do to stay informed about OCD and ADHD?
It is important for parents and professionals to stay updated on the latest research and statistics regarding these comorbidities, particularly as we approach 2025, to better support affected youth.




