Overview
The article compares Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) by examining their core symptoms, overlapping characteristics, and treatment challenges. It emphasizes the importance of accurate diagnosis and tailored treatment strategies due to the significant symptom overlap, which can complicate care and exacerbate conditions if misdiagnosed.
Introduction
In the intricate landscape of mental health, the coexistence of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) presents a unique set of challenges. Both disorders, while distinct in their core symptoms, often share overlapping behaviors that can complicate diagnosis and treatment.
As individuals navigate the complexities of daily life, the interplay between compulsive actions and attention difficulties can significantly impact their academic, social, and emotional well-being. Recent studies illuminate the prevalence of these conditions, revealing a pressing need for greater awareness and tailored interventions.
With nearly half of children diagnosed with ADHD receiving behavioral treatment, understanding the nuances of these disorders is crucial for fostering effective support systems and enhancing the quality of life for those affected.
Understanding OCD and ADHD: Definitions and Core Symptoms
Obsessive-Compulsive Disorder (OCD) is characterized by the presence of persistent, intrusive thoughts referred to as obsessions, often occurring alongside symptoms of obsessive compulsive disorder ADHD, which involve repetitive actions or mental acts known as compulsions that individuals feel driven to engage in. Common obsessions often revolve around fears of contamination, harm, or the need for symmetry, while compulsions may manifest as excessive cleaning rituals or repetitive checking behaviors. On the other hand, Attention-Deficit/Hyperactivity Disorder is defined by signs of inattention, hyperactivity, and impulsivity.
Individuals with attention deficit hyperactivity disorder frequently face challenges in maintaining focus, completing tasks, and adhering to social norms, often exhibiting restlessness. Recognizing these fundamental signs is crucial for differentiating between the two disorders, despite cases where they may exhibit similar behaviors. The complexity of symptom recognition is underscored by recent studies, which reveal that 21% of adults with a substance use disorder also have attention deficit hyperactivity disorder, indicating a significant overlap that warrants further exploration.
Furthermore, Jenna Nielsen, a Licensed Clinical Social Worker, points out that:
- '19% of U.S. counties lack mental health resources,' stressing the need for improved accessibility to care for individuals with obsessive compulsive disorder ADHD as well as attention deficit hyperactivity disorder.
- A study indicated an average global adult attention deficit hyperactivity disorder prevalence of 3.4%, suggesting that this condition is common among adults, warranting further research and attention to adult diagnosis and treatment.
- In 2021, many children received care for obsessive compulsive disorder ADHD and attention deficit hyperactivity disorder from primary care clinicians, with almost half covered by private insurance and about 1 in 4 children with Medicaid receiving care from a pediatrician, illustrating the importance of understanding these conditions in the current healthcare landscape.
The Overlap: Shared Symptoms and Behaviors of OCD and ADHD
The convergence of symptoms between attention deficit hyperactivity disorder and obsessive compulsive disorder (ADHD) is characterized by substantial overlap, especially in aspects such as inattention and repetitive actions. For instance, compulsive checking actions in individuals with obsessive compulsive disorder (OCD) can reflect the impulsiveness generally seen in attention deficit hyperactivity disorder. This resemblance highlights the complexity of diagnosing and treating these conditions, as both can hinder focus and concentration.
However, it is crucial to note that the motivations behind these behaviors differ. Dr. Mia Armstrong, a prominent MD, emphasizes that parenting a child with attention deficit hyperactivity disorder may take a unique approach, reinforcing the necessity for tailored strategies in treatment. Recent findings indicate that roughly 11.8% of individuals diagnosed with obsessive compulsive disorder also exhibit characteristics of attention deficit hyperactivity disorder, which can worsen the intensity of obsessive compulsive disorder manifestations and lead to a less promising outlook when both conditions are present.
A pertinent case study titled 'Co-occurrence of Attention Disorders and OCD' illustrates this point, as it discusses the treatment outcomes of a patient who was discharged with a new medication regimen and continued to show improvements in both OCD and attention disorder indicators. Furthermore, it is essential to recognize that attention deficit hyperactivity disorder is characterized as an externalizing behavior, affecting interactions with the environment, while OCD is viewed as internalizing, with individuals responding to anxiety by turning inward. Thus, a comprehensive understanding of these shared indicators is essential for parents and clinicians alike, as it aids in developing effective treatment plans that address the unique challenges posed by both conditions.
Navigating Diagnostic Challenges: Misdiagnosis and Overlap
Identifying obsessive compulsive disorder, ADHD, and attention deficit disorder presents significant challenges for clinicians, primarily due to the overlapping characteristics that can obscure the underlying condition. Misdiagnosis not only complicates treatment but can also exacerbate the issues at hand. For example, a child showing compulsive tendencies may be wrongly diagnosed with attention deficit hyperactivity disorder (ADHD), when in reality, the underlying issue is obsessive-compulsive disorder.
This misjudgment can lead to treatment plans that fail to address the actual disorder, potentially worsening the child’s condition. Recent data indicates that about 7% of college students report using non-prescribed stimulants, often in an attempt to manage undiagnosed attention disorders or related issues, highlighting the urgency for accurate diagnoses. Thorough evaluations that assess the complete range of behaviors and signs are essential for obtaining precise diagnoses.
The Lifespan Development of attention deficit hyperactivity disorder symptoms study sheds light on the developmental trajectory of these conditions, revealing that signs resembling attention deficit hyperactivity disorder in children with OCD may diminish as they enter adolescence. This evidence suggests that while dual diagnoses of obsessive compulsive disorder, ADHD, and attention deficit hyperactivity disorder are rare in adults, they often coexist with other disorders, such as chronic tic disorder. As Elena Cox, a senior data reporter, notes, 'The intersection of mental health and educational challenges is often overlooked, leading to significant consequences for individuals.'
Given that 19% of U.S. counties lack adequate mental health resources, the importance of thorough diagnostic practices cannot be overstated, as misdiagnosis can lead to dire consequences. Jenna Nielsen, a Licensed Clinical Social Worker, emphasizes that 'a nuanced understanding of these conditions is essential for effective treatment and support.
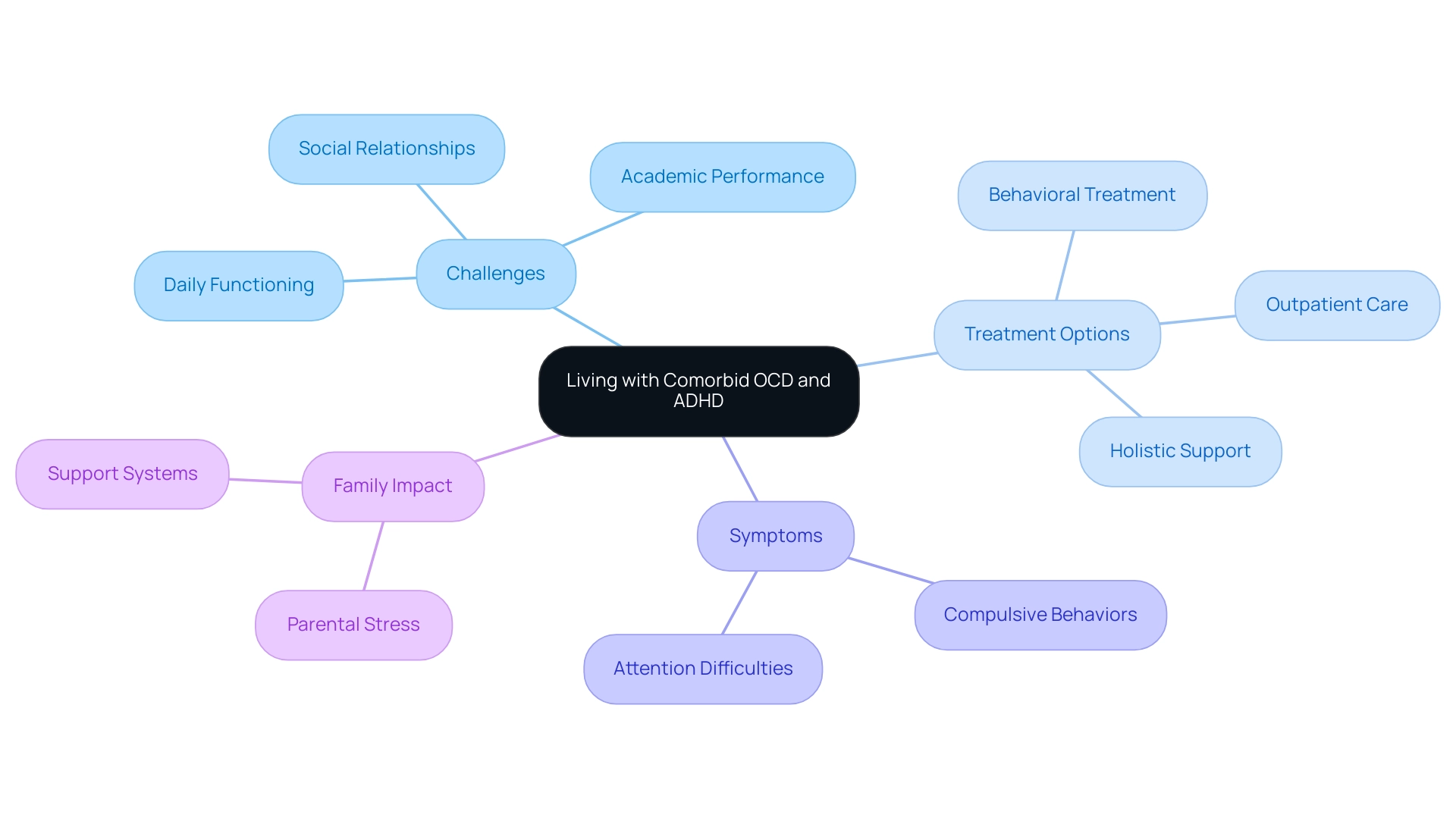
Living with Both: The Impact of Comorbid OCD and ADHD on Daily Life
Navigating life with both obsessive compulsive disorder ADHD and Attention-Deficit/Hyperactivity Condition presents a multifaceted set of challenges for individuals and their families. The interplay between compulsive behaviors associated with obsessive compulsive disorder ADHD and the attention difficulties typical of attention disorders can profoundly disrupt daily functioning, influencing everything from academic performance to social relationships. As recent statistics indicate, 44.4% of children aged 3-17 years received behavioral treatment for attention deficit hyperactivity disorder in the past year, underscoring the need for effective interventions.
It is essential to understand that obsessive compulsive disorder ADHD may produce manifestations that resemble attention deficit hyperactivity disorder, leading to potential misdiagnosis, which can complicate treatment strategies. Parents managing a child exhibiting signs of obsessive compulsive disorder ADHD often experience heightened stress and potential burnout, exacerbated by the complexities of these overlapping conditions. As Danielson ML notes, understanding who offers outpatient clinical care for adults with attention deficit hyperactivity disorder is vital for effective treatment pathways.
Furthermore, the implications of childhood trauma further complicate this landscape, as research suggests a connection between such experiences and the emergence of symptoms related to obsessive compulsive disorder ADHD, as illustrated in the case study titled 'Childhood Trauma and Developmental Conditions.' By fostering support systems that holistically address the unique needs of families affected by these disorders, we can better equip them to navigate these hurdles and promote healthier, more balanced lives.
Conclusion
The coexistence of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) presents significant challenges, particularly in diagnosis and treatment. The distinct yet overlapping symptoms of these disorders can lead to misdiagnosis, complicating the treatment process and potentially worsening the individual’s condition. Understanding the core symptoms of OCD and ADHD is essential, as it allows for more accurate assessments and tailored interventions that address the unique needs of those affected.
The shared symptoms, such as compulsive behaviors and difficulties with attention, highlight the complexity of managing both conditions simultaneously. Recent studies indicate that a notable percentage of individuals with OCD may also exhibit ADHD symptoms, which can exacerbate the severity of their OCD. This overlap necessitates a nuanced approach in treatment strategies, emphasizing the importance of comprehensive evaluations that consider the full spectrum of symptoms and behaviors.
Living with both OCD and ADHD can disrupt various aspects of daily life, from academic performance to social interactions. The stress experienced by families navigating these challenges underscores the necessity for effective support systems and accessible mental health resources. By fostering a deeper understanding of these disorders and their interplay, clinicians and caregivers can better equip themselves to provide the necessary support, ultimately enhancing the quality of life for those affected. Raising awareness and advocating for tailored interventions are vital steps toward improving outcomes for individuals living with both OCD and ADHD.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
OCD is characterized by persistent, intrusive thoughts known as obsessions, which often lead to repetitive actions or mental acts called compulsions that individuals feel compelled to perform.
What are common obsessions and compulsions associated with OCD?
Common obsessions include fears of contamination, harm, or the need for symmetry. Compulsions may manifest as excessive cleaning rituals or repetitive checking behaviors.
How is Attention-Deficit/Hyperactivity Disorder (ADHD) defined?
ADHD is defined by signs of inattention, hyperactivity, and impulsivity, leading individuals to struggle with maintaining focus, completing tasks, and adhering to social norms, often exhibiting restlessness.
What is the significance of recognizing the signs of OCD and ADHD?
Recognizing the fundamental signs of both disorders is crucial for differentiating between them, as they may exhibit similar behaviors.
What does recent research indicate about the overlap between substance use disorders and ADHD?
Recent studies reveal that 21% of adults with a substance use disorder also have ADHD, indicating a significant overlap that requires further exploration.
What did Jenna Nielsen report regarding mental health resources in the U.S.?
Jenna Nielsen noted that 19% of U.S. counties lack mental health resources, highlighting the need for improved accessibility to care for individuals with OCD and ADHD.
What is the global prevalence of ADHD among adults?
A study indicated an average global adult ADHD prevalence of 3.4%, suggesting that this condition is common among adults and warrants further research and attention to diagnosis and treatment.
How do children typically receive care for OCD and ADHD?
In 2021, many children received care for OCD and ADHD from primary care clinicians, with almost half covered by private insurance and about 1 in 4 children with Medicaid receiving care from a pediatrician.




