Overview
The article provides a comprehensive guide for parents on managing Attention-Deficit/Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder (OCD), emphasizing the importance of understanding both conditions and their interrelation. It highlights effective treatment strategies, the significance of thorough assessments for co-occurring conditions, and the need for structured daily routines and support networks, thereby equipping parents with essential tools and resources for navigating these complex disorders.
Introduction
Navigating the complexities of Attention-Deficit/Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder (OCD) presents unique challenges for children and their families. With ADHD characterized by inattention, hyperactivity, and impulsivity, and OCD defined by intrusive thoughts and compulsive behaviors, the intersection of these disorders can significantly impact a child's daily life.
Recent research highlights a concerning overlap, with many children diagnosed with one condition also exhibiting symptoms of the other. This connection underscores the critical need for comprehensive assessment and tailored treatment strategies.
As parents seek effective ways to support their children, understanding the nuances of both disorders becomes essential for fostering a nurturing environment that promotes growth and resilience.
Understanding ADHD and Obsessive-Compulsive Disorder
Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by a range of symptoms, including inattention, hyperactivity, and impulsivity. These traits can significantly disrupt a young person's ability to concentrate on tasks, manage their impulses, and navigate social interactions effectively. Conversely, Obsessive-Compulsive Disorder (OCD) manifests through unwanted, intrusive thoughts known as obsessions and repetitive actions termed compulsions, which individuals feel driven to perform.
Understanding these definitions is crucial for effective management. Research highlights a significant link between ADHD obsessive compulsive disorder and obsessive-compulsive disorder; importantly, relatives impacted by ADHD obsessive compulsive disorder experience a 7.4% higher risk of developing obsessive-compulsive disorder, compared to just 1.3% among individuals without ADHD obsessive compulsive disorder. This interrelation highlights the importance of recognizing how these disorders can co-occur, affecting the daily lives of young individuals.
Masi emphasizes that it is recommended that children diagnosed with OCD be screened for ADHD obsessive compulsive disorder, further supporting the need for comprehensive care. Jenna Nielsen, a Licensed Clinical Social Worker, echoes this sentiment, indicating that addressing both conditions can lead to more effective support. Additionally, a case study titled 'Missed Diagnosis of Co-occurring Conditions' reveals that many individuals with both ADHD obsessive compulsive disorder and attention deficit hyperactivity disorder may only receive a diagnosis for one condition, leading to missed opportunities for comprehensive treatment.
This underscores the critical need for thorough assessments. Furthermore, a nationwide survey found that 19% of U.S. counties lack adequate mental health resources, which complicates the support available for families navigating attention deficit hyperactivity disorder and OCD, highlighting a significant gap in mental health care.
Recognizing the Signs: Symptoms of ADHD and OCD
Children showing signs of Attention Deficit Hyperactivity Disorder often struggle with maintaining focus, experience forgetfulness, exhibit fidgeting behaviors, and may frequently interrupt conversations. These characteristics can significantly impact their daily functioning at home and in school. In contrast, those with Obsessive Compulsive Disorder (OCD) might face persistent and distressing fears related to contamination or potential harm, which can manifest in compulsive behaviors such as excessive washing or checking.
According to Cynthia Reuben, a specialist in youth psychology, overall, 11.3% of individuals aged 5–17 years had ever been diagnosed with attention deficit hyperactivity disorder. This statistic emphasizes the significance of being alert regarding youth's behavior. Significantly, the occurrence of attention deficit hyperactivity disorder diagnosis in adults has been rising due to factors such as pandemic effects and heightened awareness, which together contribute to the increasing numbers of diagnoses among youths.
The proportion of youngsters identified with attention deficit hyperactivity disorder in the US has almost doubled over the last twenty years, with a notable increase in diagnoses among females and minority groups. This trend may indicate improved awareness and access to services; however, it also raises concerns about potential overdiagnosis and unrealistic attentional expectations. Monitoring for symptoms enables parents to seek appropriate support and implement effective intervention strategies, which can significantly improve outcomes for their offspring.
Furthermore, current trends indicate a concerning overlap between attention deficit hyperactivity disorder and ADHD obsessive compulsive disorder symptoms in children, with those ages 12–17 years being more likely to have ADHD obsessive compulsive disorder than those ages 5–11 years across all family income levels. This underscores the need for parents to be informed and proactive in addressing these challenges.
Identifying Risk Factors for ADHD and OCD
Comprehending the risk factors for attention deficit hyperactivity disorder is crucial for parents, as they encompass a range of influences, including:
- Genetic predisposition
- Exposure to toxins during pregnancy
- Premature birth
Recent studies indicate a pooled prevalence of attention deficit hyperactivity disorder at approximately 27% in screening studies, suggesting an urgent need for awareness and diagnosis, particularly in adult populations. As noted by Danielson ML, "Who Provides Outpatient Clinical Care for Adults With Attention Deficit Hyperactivity Disorder?"
"Analysis of Healthcare Claims by Types of Providers Among Private Insurance and Medicaid Enrollees, 2021," this highlights the importance of understanding the healthcare landscape for attention deficit hyperactivity disorder. The increase in attention deficit hyperactivity disorder diagnoses may indicate better awareness and access to services, but it also raises concerns about potential overdiagnosis and unrealistic attentional expectations. For OCD, susceptibility is often influenced by:
- Family history
- Stressful life events
- Specific personality traits
Recognizing these risk factors empowers parents to remain vigilant and seek early intervention when they observe concerning behaviors in their children. Furthermore, a systematic review of adult attention deficit hyperactivity disorder prevalence reinforces the need for increased awareness and diagnosis of this condition in adult populations, particularly in psychiatric settings.
Effective Treatment Strategies for ADHD and OCD
Effective management strategies for Attention Deficit Hyperactivity Disorder often involve a multifaceted approach that includes:
- Behavioral therapy
- Psychoeducation
- Medication options such as stimulants and non-stimulants
Behavioral therapy focuses on modifying specific behaviors through reinforcement and structured support, which can be particularly beneficial for children navigating ADHD symptoms. In contrast, for Obsessive Compulsive Disorder (OCD), Cognitive Behavioral Therapy (CBT) stands out as a highly effective intervention.
This therapy typically incorporates exposure and response prevention techniques, allowing individuals to confront their fears in a controlled environment while learning to resist compulsive behaviors. As mentioned by specialists in the field, clinicians should closely examine the diagnostic factors that may affect outcomes. Amitai Abramovitch, a neuropsychologist at Massachusetts General Hospital, emphasizes the necessity for thorough assessments, particularly regarding impulsivity and risk-taking behaviors, to ensure accurate diagnoses and effective care strategies.
Recent studies indicate a growing recognition of the prevalence of comorbid ADHD obsessive compulsive disorder among OCD patients, with nearly 16.1% of adults with OCD also exhibiting symptoms of this condition. This statistic underscores the need for tailored therapeutic strategies that address both conditions simultaneously. For example, a case study on a 33-year-old male patient with coexisting ADHD obsessive compulsive disorder showed significant improvement following intervention with a combination of extended-release methylphenidate and sertraline.
This emphasizes the significance of a customized care approach that corresponds with each young person's unique requirements. Parents are encouraged to collaborate with healthcare professionals to ensure a comprehensive approach to managing these complex disorders.
Building a Support Network: Resources for Parents
To navigate the complexities of parenting children with ADHD obsessive compulsive disorder, it is essential to explore local and online support groups. Organizations such as CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) and the International OCD Foundation are invaluable resources for families, providing a wealth of information and support for those dealing with ADHD obsessive compulsive disorder, as well as networking opportunities. Engaging with these communities allows parents to share experiences, strategies, and coping mechanisms that can significantly alleviate the challenges they face.
It is vital to acknowledge that individuals diagnosed with ADD have a lower life expectancy than those without the disorder, highlighting the significance of support and effective care. Additionally, as Susan Stutzman, owner and advocate, states in the Parent Matters Podcast, "Connecting with others who understand the journey can make all the difference." Furthermore, connecting with professionals, including therapists and educators, enhances the support system.
Brightside Health creates customized treatment plans for attention disorders, emphasizing the importance of tailored support for families. These specialists can offer customized guidance and efficient approaches that meet the distinct requirements of each individual, ensuring that parents feel empowered and prepared to advocate for their offspring's well-being.
Navigating Co-Occurring ADHD and OCD
Children diagnosed with ADHD obsessive compulsive disorder and OCD often face compounded challenges, including increased anxiety and concentration difficulties, as compulsive behaviors can further impair attention. Research indicates that among children with ADHD obsessive compulsive disorder, approximately 19% also meet the criteria for OCD, as reported by Farrell and colleagues, suggesting a significant overlap in these conditions. However, it's important to note that only 12% of studies have excluded tic disorders, which may inflate co-occurrence rates.
This dual diagnosis of ADHD obsessive compulsive disorder can complicate care, as both disorders share dysfunctions in impulsivity and executive function yet have opposing underlying mechanisms. Additionally, the higher male prevalence in ADHD may artificially inflate ADHD cases in OCD samples, further complicating diagnosis and care. As a result, parents are encouraged to collaborate closely with healthcare providers to devise an integrated care plan that effectively addresses both conditions.
This plan should ensure that interventions for one disorder do not inadvertently exacerbate the other. Maintaining open lines of communication with educators and therapists is essential to create a consistent support system across various environments, ultimately enhancing the overall treatment outcomes. Current strategies highlight the significance of personalized methods, as young individuals with ADHD obsessive compulsive disorder and attention difficulties who also have co-existing conditions tend to exhibit more severe symptoms, necessitating comprehensive care that adjusts to their unique needs.
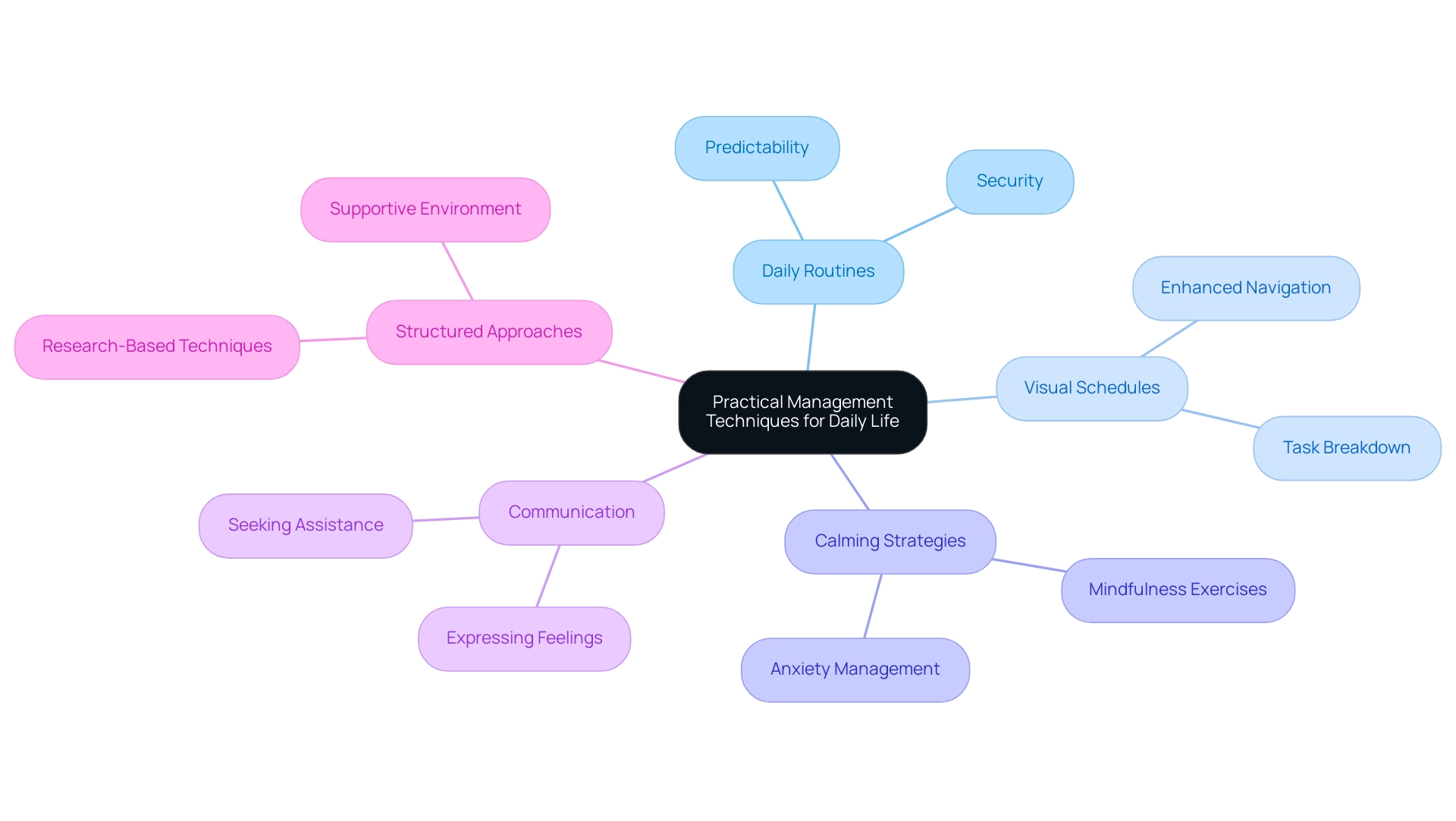
Practical Management Techniques for Daily Life
Establishing daily routines that highlight structure and predictability is crucial for individuals with OCD, promoting a sense of security and stability. Techniques such as utilizing visual schedules and breaking tasks into manageable steps can significantly enhance a young person's ability to navigate daily challenges. Research indicates that a study investigating the use of paroxetine in patients with co-morbid ADHD obsessive compulsive disorder found that the response rates for OCD were significantly less than in patients with OCD alone, highlighting the severity of symptoms and the necessity for structured approaches.
Moreover, youngsters with ADHD obsessive compulsive disorder and accompanying issues, such as behavioral or conduct problems, frequently encounter more intense symptoms than those without extra conditions, as observed by development specialists. Incorporating calming strategies like mindfulness exercises can also be beneficial, providing young individuals with tools to manage anxiety and improve focus. Additionally, brain-mapping studies suggest that shared and disorder-specific brain dysfunctions in both ADHD and ADHD obsessive compulsive disorder impact self-control and decision-making, reinforcing the need for predictable routines.
Maintaining open lines of communication about feelings and challenges empowers young individuals to express themselves and seek assistance when necessary. Child development specialists emphasize that predictable routines can lead to improved emotional regulation, ultimately fostering a more supportive environment for children facing these challenges.
Conclusion
Navigating the complexities of ADHD and OCD requires a multifaceted understanding of both disorders and their interplay. The prevalence of ADHD and its alarming overlap with OCD emphasizes the necessity for comprehensive assessments and tailored treatment plans. Research indicates that children with ADHD often experience symptoms that can complicate the management of OCD, and vice versa. Therefore, recognizing the signs and understanding the risk factors associated with both conditions is crucial for parents and caregivers.
Effective treatment strategies should be holistic, incorporating:
- Behavioral therapies
- Psychoeducation
- Medication that addresses both conditions simultaneously
Collaboration with healthcare professionals and the establishment of a strong support network can significantly enhance the effectiveness of treatment. Engaging with resources such as support groups and educational organizations provides families with valuable insights and emotional support, helping them to navigate the challenges associated with ADHD and OCD.
Ultimately, fostering a nurturing and structured environment is essential for children facing these disorders. Implementing daily routines, utilizing calming techniques, and maintaining open communication can empower children to manage their symptoms effectively. By prioritizing awareness, understanding, and tailored interventions, families can foster resilience and promote a pathway toward improved mental health and well-being for their children.
Frequently Asked Questions
What are the main characteristics of Attention-Deficit/Hyperactivity Disorder (ADHD)?
ADHD is characterized by symptoms of inattention, hyperactivity, and impulsivity, which can disrupt a young person's ability to concentrate on tasks, manage impulses, and navigate social interactions.
How does Obsessive-Compulsive Disorder (OCD) manifest in individuals?
OCD manifests through unwanted, intrusive thoughts known as obsessions and repetitive actions called compulsions, which individuals feel compelled to perform.
Is there a relationship between ADHD and OCD?
Yes, research indicates a significant link between ADHD and OCD. Individuals with ADHD have a 7.4% higher risk of developing OCD compared to 1.3% among those without ADHD.
What is recommended for children diagnosed with OCD?
It is recommended that children diagnosed with OCD be screened for ADHD to ensure comprehensive care.
What did a case study reveal about the diagnosis of ADHD and OCD?
The case study titled 'Missed Diagnosis of Co-occurring Conditions' showed that individuals with both ADHD and OCD often only receive a diagnosis for one condition, leading to missed opportunities for comprehensive treatment.
What challenges exist in accessing mental health resources for ADHD and OCD?
A nationwide survey found that 19% of U.S. counties lack adequate mental health resources, complicating support for families dealing with ADHD and OCD.
What are common symptoms of ADHD in children?
Children with ADHD may struggle with maintaining focus, experience forgetfulness, exhibit fidgeting behaviors, and frequently interrupt conversations.
What are common symptoms of OCD?
Individuals with OCD may face persistent fears related to contamination or potential harm, often leading to compulsive behaviors like excessive washing or checking.
What is the prevalence of ADHD diagnoses among children?
According to statistics, 11.3% of individuals aged 5–17 years have been diagnosed with ADHD, highlighting the importance of monitoring youth behavior.
How has the diagnosis of ADHD changed in recent years?
The occurrence of ADHD diagnoses in adults is rising, influenced by pandemic effects and increased awareness, with a notable increase among females and minority groups.
Are there concerns about the overdiagnosis of ADHD?
Yes, while increased diagnoses may indicate better awareness and access to services, there are concerns about potential overdiagnosis and unrealistic expectations regarding attention.
What trends are observed regarding ADHD and OCD symptoms in adolescents?
Current trends indicate a concerning overlap between ADHD and OCD symptoms in children, particularly in those aged 12–17 years, suggesting that parents should be informed and proactive in addressing these challenges.




