Overview
The article "How to Manage OCD, ADHD, and Anxiety: A Step-by-Step Guide for Parents" serves as a compassionate resource for parents seeking to support their children through these interconnected mental health challenges. It draws attention to the critical need for early recognition and the development of tailored treatment plans that cater to individual needs. By fostering supportive environments, parents can significantly impact their children's well-being.
Research underscores that comprehensive management approaches not only enhance understanding but also lead to improved outcomes for affected children. This guide aims to empower parents with effective strategies, creating a nurturing space for both parents and children to thrive together. As you navigate this journey, remember that you are not alone—there are resources and communities ready to support you.
Introduction
In a world where mental health issues among children are increasingly prevalent, it is essential to understand the complexities of conditions such as Obsessive-Compulsive Disorder (OCD), Attention-Deficit/Hyperactivity Disorder (ADHD), and anxiety. These disorders often intertwine, presenting a challenging landscape for parents and caregivers who are striving to provide effective support.
Research highlights the significant overlap between these conditions, emphasizing that recognizing symptoms early can lead to better outcomes and an improved quality of life for affected children. This article will explore the definitions, symptoms, and management strategies for OCD, ADHD, and anxiety, offering valuable insights into navigating these intricate challenges. Together, we can foster a supportive environment for children and families alike.
Understanding OCD, ADHD, and Anxiety: Key Definitions and Symptoms
Obsessive-Compulsive Disorder (OCD) is characterized by persistent, intrusive thoughts known as obsessions, along with repetitive behaviors or mental acts called compulsions that individuals feel compelled to perform. For many, this may manifest as excessive hand-washing, repeated checking of locks or appliances, or compulsive counting. In young individuals, such behaviors can significantly disrupt daily activities and social interactions, leaving them feeling isolated and overwhelmed.
Attention-Deficit/Hyperactivity Disorder (ADHD) presents with symptoms such as inattention, hyperactivity, and impulsivity, which can impede a young person's ability to focus on tasks or manage their impulses. This often results in challenges in academic settings and difficulties in maintaining relationships with peers, creating a cycle of frustration and self-doubt.
Anxiety disorders, marked by excessive worry, fear, or nervousness, can lead to avoidance behaviors that further complicate a child's ability to engage in everyday activities. Recent research highlights that 40.3% of patients with OCD may also experience comorbid conditions, including ADHD and anxiety. This underscores the interconnected nature of these disorders, emphasizing that they often do not exist in isolation. Additionally, 59% of adolescents report having positive childhood experiences (PCEs), which are linked to a lower likelihood of diagnosed mental health conditions, reinforcing the importance of nurturing and supportive environments.
Recognizing these symptoms early is crucial for effective management and support. For instance, a study on the duration of untreated illness in OCD revealed that patients with comorbid conditions often experience a significantly longer duration of untreated OCD. Addressing these comorbidities promptly can lead to improved long-term outcomes, allowing young individuals to thrive and flourish.
The study emphasizes that early intervention can significantly shorten the duration of untreated OCD, enhancing the overall prognosis and offering hope to families navigating these challenges.
As we move into 2025, the definitions and symptoms of OCD, ADHD, and anxiety continue to evolve. Experts stress the importance of understanding these conditions as part of a broader spectrum of mental health challenges. Psychologists highlight that recognizing the overlap between these disorders can help individuals and families feel less isolated in their struggles. Dr. Nicholas Farrell, Clinical Director at NOCD, notes, "Recognizing these subtypes can help individuals realize they are not alone in their struggles."
Therefore, nurturing a supportive and informed atmosphere is essential for caregivers grappling with these intricate matters. It is equally important to acknowledge that 17% of teens report experiencing emotional mistreatment by a guardian, which can significantly affect mental health outcomes. By fostering understanding and compassion, we can create a more supportive environment for all families facing these challenges.
Navigating the Challenges: Common Issues in Managing OCD, ADHD, and Anxiety
Navigating the challenges of OCD, ADHD, and anxiety in children can be a daunting journey for parents. The struggle to maintain consistent routines, manage school-related stress, and nurture healthy social interactions often weighs heavily on families. Children facing these conditions frequently encounter hurdles in forming peer relationships, leading to feelings of isolation and loneliness.
For instance, research shows that nearly 50% of youngsters with OCD, ADHD, and anxiety report difficulties in establishing and maintaining friendships, highlighting the social challenges they face.
The neuropsychological aspects of ADHD can complicate matters, as deficits may arise from dysfunctional executive functions or a compromised motivational system. Parents often find themselves in a state of heightened vigilance, constantly monitoring their child's behavior and providing the necessary support. This relentless responsibility can lead to significant stress and fatigue, as they strive to balance parenting with the complexities of their child's needs.
As health behavior expert Riana Elyse Anderson poignantly remarked, "The pandemic really pointed to how challenging it was to manage all these stressors with thinning coping resources."
Acknowledging these challenges is essential for developing effective management strategies. A case study involving a child named T. underscores the value of psychometric evaluations in assessing the severity of symptoms. T. underwent evaluations that revealed clinically significant levels of ADHD and obsessive-compulsive symptoms, which informed tailored treatment recommendations.
Despite his behavioral challenges, T.'s above-average IQ of 122 highlights the potential for success when provided with appropriate support.
As we look to 2025, the landscape of managing these conditions continues to evolve, presenting new challenges for parents. Statistics reveal a rising prevalence of anxiety disorders among youth with OCD, ADHD, and anxiety, further complicating their management. Additionally, while the TPH2 gene has shown a significant link to ADHD, it has not been associated with OCD in meta-analysis, emphasizing the unique biological factors at play.
By recognizing these difficulties and seeking support, parents can better navigate the complexities of their child's mental health journey. Sharing experiences and connecting with others can foster a sense of community, reminding parents that they are not alone in this endeavor.
Diagnosis Matters: Differentiating Between OCD, ADHD, and Anxiety
Understanding the distinctions between OCD, ADHD, and anxiety is vital for effective treatment and management. OCD is primarily marked by persistent obsessions and compulsions, which can significantly disrupt daily life. In contrast, ADHD is characterized by difficulties with attention, hyperactivity, and impulse regulation, often leading to challenges in educational and social settings.
Anxiety, which can coexist with OCD and ADHD, typically manifests as excessive worry and fear, impacting a person's ability to function normally. Recognizing these differences is crucial for parents navigating their children's mental health.
A thorough assessment by a qualified mental health expert is essential for an accurate diagnosis. This evaluation should encompass a comprehensive review of symptoms and their effects on daily functioning. Alarmingly, recent statistics indicate that misdiagnosis rates for these conditions can be quite high, particularly among young individuals.
For instance, many young people with OCD, ADHD, and anxiety are often misdiagnosed with anxiety disorders, leading to inappropriate treatment approaches that fail to address the underlying issues. Additionally, a significant amount of ADHD-related content on social media platforms like TikTok can be misleading, highlighting the importance of seeking trustworthy information.
Real-world examples underscore the necessity of differential diagnosis. In one notable case study, children receiving ADHD treatment from primary care providers often lacked access to specialized services, particularly those on Medicaid. This gap in care emphasizes the need for parents to advocate for comprehensive assessments that consider all potential diagnoses.
As Amitai Abramovitch, PhD, points out, clinicians should assess two primary diagnostic elements that can aid in achieving a more precise diagnosis. Moreover, unrecognized ADHD can profoundly impact mental well-being, social interactions, and professional life, making accurate diagnosis crucial not just for effective treatment but also for improving overall mental health outcomes.
As awareness of these disorders increases, especially through platforms like TikTok, it is essential to navigate the information landscape carefully, as much of it can be misleading. Parents are encouraged to seek out reliable resources and support networks, ensuring they are well-informed and equipped to manage these complex conditions.
Effective Treatment Strategies: Evidence-Based Approaches for Managing Symptoms
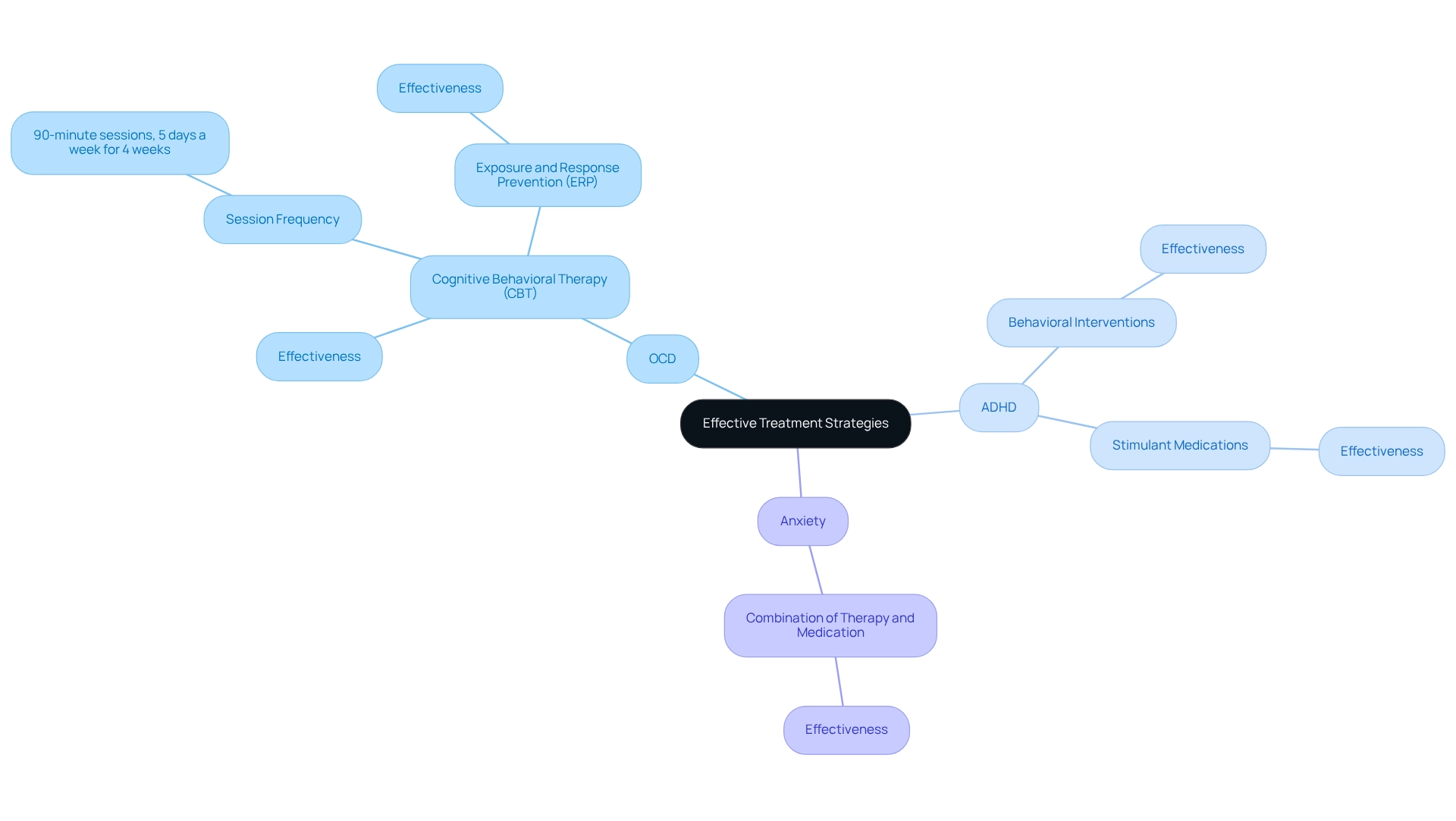
Effectively managing OCD, ADHD, and anxiety requires a multifaceted approach that blends behavioral therapies with medication. Cognitive Behavioral Therapy (CBT), particularly Exposure and Response Prevention (ERP) for OCD, has shown promising results. Research reveals that participants undergoing CBT for OCD typically engage in 90-minute therapy sessions five days a week for four weeks, highlighting the intensive nature of this treatment and its potential for success.
When it comes to ADHD, implementing behavioral interventions alongside stimulant medications can significantly enhance focus and reduce impulsivity, leading to better daily functioning.
In instances of anxiety, especially those involving OCD, ADHD, and anxiety, a combination of therapy and medication often emerges as the most effective strategy. It is crucial for caregivers to collaborate closely with healthcare providers to create a tailored treatment plan that addresses their child's specific needs, particularly concerning OCD, ADHD, and anxiety, ensuring that all facets of their mental health are considered.
The National Institute of Mental Health (NIMH) estimates that 1.2% of adults experience OCD, underscoring the prevalence of this condition and the necessity for effective treatment options. Future research should prioritize equitable access to high-quality CBT interventions while innovating to meet the diverse needs of patients. This focus is vital as the mental health treatment landscape evolves, with findings suggesting that CBT for OCD may involve strengthening compensatory processes across brain networks rather than merely normalizing dysfunctional circuits.
Recognizing that the average age of onset for OCD is around 19 years, but can manifest as early as 2 or 3, highlights the importance of early identification and intervention strategies for those at risk. By understanding these dynamics, parents can more effectively advocate for treatment options that support their child's mental health journey.
The Role of Therapy and Support: Building a Strong Support System
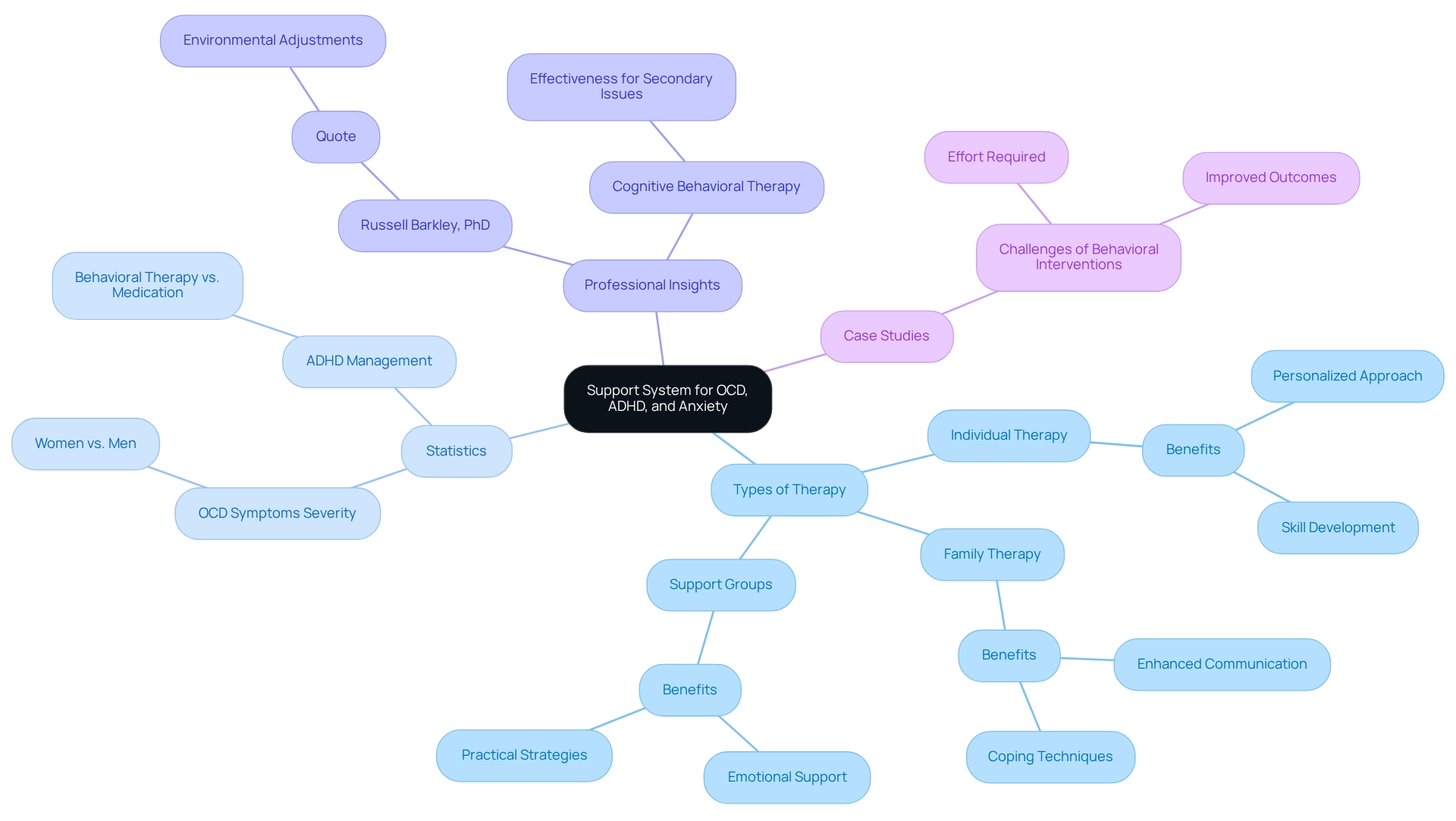
Therapy plays a crucial role in effectively managing OCD, ADHD, and anxiety, offering a multifaceted approach that includes individual therapy, family therapy, and support groups. Engaging in family therapy can significantly enhance communication and coping techniques within the home, fostering a more supportive environment for children facing these challenges. Research indicates that while some young individuals with attention deficit hyperactivity disorder can manage symptoms with only behavioral therapy, many require medication, underscoring the need for tailored strategies.
Russell Barkley, PhD, an ADHD specialist, emphasizes that "ideally, these environmental adjustments will alter the developmental trajectory of the child or adolescent with ADHD."
Support groups serve as invaluable resources for caregivers, allowing them to share experiences and glean insights from others in similar situations. These groups not only offer emotional support but also practical strategies for navigating daily challenges. The impact of such support systems is profound; caregivers frequently express feeling less isolated and more empowered when they connect with others who understand their struggles.
Statistics reveal that women may experience more severe symptoms of OCD than men, highlighting the necessity for targeted support across different demographics. Furthermore, professional insights suggest that family therapy can play a vital role in addressing the complexities of OCD, ADHD, and anxiety, particularly during childhood. A case study titled 'Challenges of Behavioral Interventions' illustrates that while these programs require significant effort from both parents and children, they can lead to improved outcomes, especially in reducing secondary issues related to attention deficit hyperactivity disorder.
Notably, there is less evidence supporting the effectiveness of behavioral training for teenagers with attention deficit hyperactivity disorder, although cognitive behavioral therapy may be beneficial for those with secondary issues.
In conclusion, establishing a robust support system through therapy and community involvement is essential for individuals grappling with OCD, ADHD, and anxiety, as well as their families. By prioritizing these resources, parents can navigate the challenges of OCD, ADHD, and anxiety more effectively, ultimately nurturing a healthier and more resilient family dynamic.
Practical Home Strategies: Daily Management Techniques for Parents
Parents can adopt a variety of effective strategies at home to help manage their children's symptoms of OCD, ADHD, and anxiety. Creating a reliable daily routine is essential, as it offers the framework and consistency that young individuals with these conditions often require. Research indicates that youngsters who adhere to structured routines experience lower anxiety levels, with a mean score of 10.8 and a standard deviation of 6.0 on the Revised Children's Manifest Anxiety Scale. This suggests that routine can significantly impact emotional well-being.
Breaking tasks into smaller, manageable steps is another practical approach that can alleviate feelings of overwhelm. This technique not only makes tasks feel less intimidating but also enables young individuals to gradually achieve their goals, fostering a sense of accomplishment.
Incorporating relaxation techniques, such as deep breathing exercises and mindfulness practices, can also play a vital role in anxiety management. These approaches assist young individuals in forming coping strategies that can be employed in challenging situations, encouraging emotional regulation.
Encouraging open communication about feelings and challenges is essential for creating a supportive environment. This conversation enables young individuals to convey their feelings and request assistance when necessary, strengthening their capacity to handle their symptoms efficiently.
Real-world examples demonstrate the effectiveness of these strategies. For instance, schools that implement behavior monitoring have reported positive outcomes, including improved student engagement and reduced dropout rates. The report titled "Importance of Behavior Monitoring in Schools" highlights that behavior monitoring is essential for detecting and correcting inappropriate behavior, guiding students in setting behavioral goals, and motivating them to change.
Such monitoring not only helps in identifying and correcting inappropriate behaviors but also fosters relationships that support students' emotional needs.
As Maria A. Rogers from the University of Ottawa observes, "The findings provide a summary of the current research on DBs for youth with attention disorders and classroom behavior, with significant implications for clinicians, parents, and educators, who are assisting children with attention disorders." This highlights the importance of organized routines and behavior tracking in effectively managing attention deficit hyperactivity disorder.
Ultimately, the combination of structured routines, task management, relaxation techniques, and open communication can significantly enhance the daily management of OCD, ADHD, and anxiety in youth, paving the way for a more supportive home environment. Consider implementing these strategies and sharing your experiences, as together we can create a nurturing space for our children.
Parent Self-Care: Prioritizing Your Well-Being While Supporting Your Child
Self-care is not just beneficial; it is essential for caregivers navigating the complexities of raising children with OCD, ADHD, and anxiety. By prioritizing mental and physical well-being, caregivers can engage more effectively with their children. Activities that promote relaxation and well-being—such as regular exercise, pursuing hobbies, or connecting with supportive friends and family—are vital for maintaining balance.
Caregiver burnout is a significant concern, as many individuals feel overwhelmed by the demands placed upon them. The financial burden of ADHD, alongside challenges related to OCD and anxiety, costs Americans approximately $42.5 billion annually. This figure underscores the stress many families face and highlights the urgent need for effective self-care strategies.
To combat this, establishing clear boundaries and allowing time for personal reflection can be transformative. Incorporating small, manageable breaks into daily routines can significantly enhance resilience. Inger Burnett-Zeigler, PhD, notes that even brief moments of relaxation can improve mental well-being, enabling caregivers to recharge and better support their children. This practical approach to self-care is crucial for sustaining parental well-being.
It's important to recognize that taking care of oneself is not an act of selfishness; rather, it is a necessary step toward becoming an effective caregiver. As Bernadette Melnyk, Vice President for Health Promotion at Ohio State, wisely states, "Positive parenting involves providing love and warmth while also ensuring structure and guidance." By investing in their own well-being, caregivers can cultivate a more supportive environment for their children, ultimately fostering improved outcomes for the entire family.
Moreover, research suggests that symptoms of attention deficit hyperactivity disorder can improve with therapy. Many young individuals facing OCD, ADHD, and anxiety may overcome these challenges, offering hope to caregivers managing these concerns.
Resources for Parents: Tools and Support for Managing OCD, ADHD, and Anxiety
Navigating the challenges of OCD, ADHD, and anxiety can feel overwhelming for parents, but there is a wealth of resources available to support you on this journey. Organizations like the International OCD Foundation and CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) offer comprehensive educational materials, support groups, and professional referrals tailored specifically for individuals facing these challenges. In 2021, many children received attention for attention disorders from primary care providers, with nearly half insured through private plans obtaining services from a pediatrician. This highlights the growing availability of services for guardians seeking help.
Moreover, online platforms have become invaluable, providing webinars, articles, and forums that foster connections among individuals experiencing similar struggles. Recent statistics reveal that anxiety disorders, including OCD, ADHD, and anxiety, affect approximately 31.9% of adolescents aged 13 to 18. This underscores the significance of these resources in addressing mental health needs. Local mental health professionals also play a crucial role, offering personalized support and guidance that can be pivotal in managing these intertwined conditions. For instance, linkage studies have identified specific chromosomal regions associated with attention deficit hyperactivity disorder and obsessive-compulsive disorder, suggesting a genetic component that may influence treatment approaches.
By utilizing these resources, caregivers can significantly enhance their ability to manage the complexities of OCD, ADHD, and anxiety, ultimately fostering a nurturing environment for their children. The latest tools and assistance available in 2025 include educational materials and support groups specifically tailored for caregivers. Real-world examples of effective support organizations for childhood anxiety demonstrate the collaborative efforts within the community to provide comprehensive care.
Expert opinions emphasize the effectiveness of these tools, reinforcing the idea that informed and connected guardians are better equipped to navigate their children’s mental health challenges. As noted by Danielson ML in 2022, an additional 1 million U.S. children aged 3-17 years had received an ADHD diagnosis compared to 2016, further highlighting the urgent need for robust support systems. ASD Media is dedicated to building a supportive community for parents, empowering them with the knowledge and resources necessary to face these challenges together.
Conclusion
Understanding and managing the complexities of OCD, ADHD, and anxiety in children is essential for creating a nurturing environment that fosters their well-being. This article has illuminated the key definitions and symptoms of these intertwined conditions, highlighting the importance of early recognition and intervention. By grasping the overlapping nature of these disorders, parents and caregivers can more effectively navigate the challenges they present.
Effective management strategies—such as evidence-based therapies, tailored treatment plans, and practical home techniques—are vital in supporting children with these conditions. Establishing consistent routines, engaging in open communication, and prioritizing self-care empower both children and their families. Moreover, accessing reliable resources and support networks can significantly enhance the overall management process, ensuring that parents feel equipped to tackle the challenges they face.
Ultimately, fostering an environment of understanding, support, and proactive engagement can lead to improved outcomes for children grappling with OCD, ADHD, and anxiety. By prioritizing mental health and advocating for effective treatment options, families can create a nurturing atmosphere that promotes resilience and emotional well-being, paving the way for a brighter future.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
OCD is characterized by persistent, intrusive thoughts known as obsessions and repetitive behaviors or mental acts called compulsions. Individuals feel compelled to perform these compulsions, which may include excessive hand-washing, repeated checking, or compulsive counting.
How does OCD affect young individuals?
OCD can significantly disrupt daily activities and social interactions for young individuals, often leaving them feeling isolated and overwhelmed.
What are the symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD)?
ADHD presents with symptoms such as inattention, hyperactivity, and impulsivity, which can impede a young person's ability to focus on tasks and manage their impulses.
What challenges do children with ADHD face?
Children with ADHD often experience difficulties in academic settings and maintaining relationships with peers, leading to frustration and self-doubt.
What are anxiety disorders, and how do they affect children?
Anxiety disorders are marked by excessive worry, fear, or nervousness, which can lead to avoidance behaviors, complicating a child's ability to engage in everyday activities.
Is there a connection between OCD, ADHD, and anxiety disorders?
Yes, research indicates that 40.3% of patients with OCD may also experience comorbid conditions, including ADHD and anxiety, highlighting the interconnected nature of these disorders.
What role do positive childhood experiences (PCEs) play in mental health?
59% of adolescents report having positive childhood experiences, which are linked to a lower likelihood of diagnosed mental health conditions, emphasizing the importance of nurturing environments.
Why is early recognition of symptoms important?
Early recognition of symptoms is crucial for effective management and support, as untreated conditions can lead to longer durations of illness and poorer outcomes.
What is the significance of addressing comorbid conditions?
Addressing comorbidities promptly can lead to improved long-term outcomes for individuals with OCD, allowing them to thrive and flourish.
How can caregivers support children facing these challenges?
Caregivers can foster a supportive and informed atmosphere, which is essential for navigating the complexities of OCD, ADHD, and anxiety in children.
What challenges do parents face when managing these conditions?
Parents may experience significant stress and fatigue as they strive to maintain consistent routines and provide necessary support for their children with these conditions.
How can sharing experiences benefit parents?
Sharing experiences and connecting with others can foster a sense of community among parents, reminding them that they are not alone in their journey.




