Overview
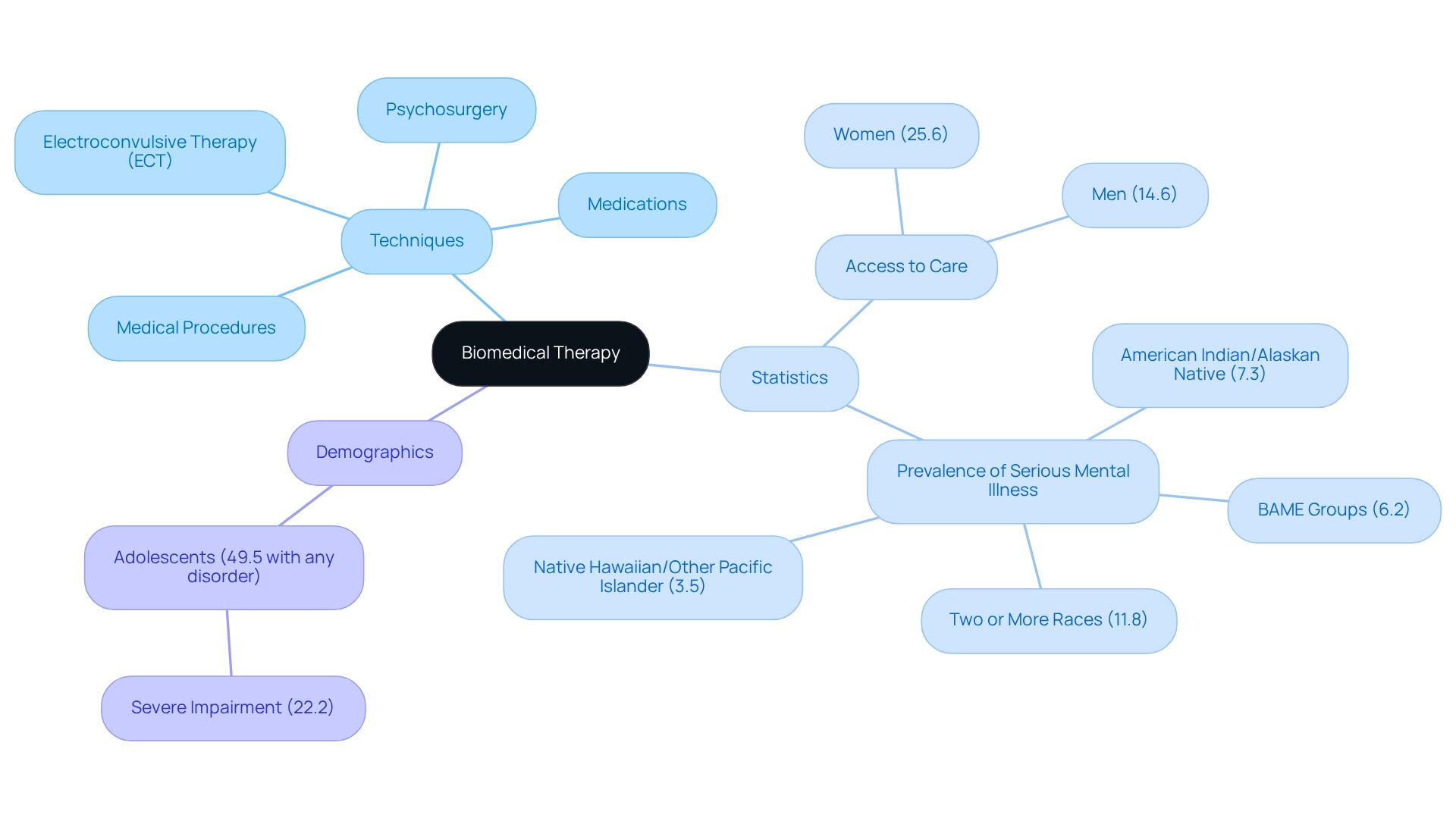
Biomedical therapy is a compassionate treatment approach that uses physiological methods, like medications and medical procedures, to help address psychological disorders by targeting their biological roots. This article sheds light on various techniques, such as pharmacotherapy and electroconvulsive therapy, illustrating how these interventions play a crucial role in managing mental health conditions effectively. By highlighting their importance, we aim to improve patient outcomes across diverse populations, fostering hope and support for those navigating these challenges.
Introduction
In the journey to support those facing mental health disorders, biomedical therapy has emerged as a vital approach, weaving together physiological methods with compassionate psychological care. This multifaceted treatment paradigm not only includes medications and medical procedures but also highlights the biological foundations of mental health conditions. As we witness a growing prevalence of mental health issues, it becomes essential to understand the nuances of biomedical therapy—spanning from pharmacotherapy to innovative techniques like electroconvulsive therapy.
With statistics revealing significant treatment gaps across various demographics, the urgency for tailored interventions that resonate with diverse populations has never been more pressing. This article invites you to delve into the intricacies of biomedical therapy, exploring its methods, effectiveness, and the promising future trends that aim to reshape mental health care.
Defining Biomedical Therapy: An Introduction
Understanding biomedical therapy is essential for addressing psychological disorders effectively. This approach encompasses a variety of techniques that utilize physiological methods to tackle these challenges. Primarily, it involves medications, medical procedures, and other biological interventions aimed at alleviating psychological symptoms. Unlike conventional psychotherapy, which focuses on behavioral and cognitive aspects, biomedical therapy emphasizes the biological foundations of psychological conditions.
This approach operates under the belief that many psychological disorders have physiological origins that can be effectively treated through medical interventions. It includes various care methods such as pharmacotherapy, which uses medications to manage symptoms; electroconvulsive therapy (ECT), a procedure that can provide relief for severe depression; and psychosurgery, which involves surgical procedures for specific psychological conditions. These elements highlight the significance of biomedical therapy in mental health care.
Recent studies reveal that approximately 25.6% of women and 14.6% of men accessed mental health care in the past year, underscoring the ongoing need for effective biomedical interventions (Terlizzi, 2020). The prevalence of serious mental illness (SMI) also varies across different demographics. For instance, the highest rates are observed among adults identifying as two or more races (11.8%) and American Indian/Alaskan Native adults (7.3%). In contrast, the lowest percentage of individuals receiving treatment is found in BAME groups, at just 6.2%. These statistics emphasize the importance of understanding biomedical therapy, which must include tailored approaches that meet the unique needs of diverse populations.
The National Survey on Drug Use and Health (NSDUH) utilized multimode data collection techniques due to the COVID-19 pandemic, providing valuable context to these statistics. Furthermore, case studies like the National Comorbidity Survey Adolescent Supplement indicate that nearly 49.5% of adolescents aged 13-18 experience some form of disorder, with 22.2% facing severe impairment. This data highlights the critical need for focused biomedical interventions to support youth psychological well-being.
As the field of biomedical intervention continues to evolve, ongoing research and development are vital to enhancing the effectiveness of these treatments. By fostering a deeper understanding of biomedical therapy, we can work towards better outcomes for individuals facing psychological challenges. If you or someone you know is struggling, consider exploring these options and seeking support tailored to your needs.
Methods and Techniques in Biomedical Therapy
What is biomedical therapy? It encompasses a variety of methods and techniques aimed at enhancing psychological outcomes through physiological interventions. Let’s explore some key strategies that can make a meaningful difference:
- Pharmacotherapy: This is the most prevalent form of biomedical treatment, employing medications to alleviate symptoms associated with psychological disorders. Common classes of medications include antidepressants, antipsychotics, and mood stabilizers. Recent findings suggest that pharmacotherapy significantly impacts therapeutic efficacy, with an effect size of 0.94 (95% CI 0.59–1.29) for depression severity as a predictor for pharmacotherapy results. This underscores the vital role medication plays in managing psychological conditions. Notably, studies indicate that women are more likely than men to have sought medication for their psychological well-being (21.2% vs. 11.5%) and to have engaged in counseling or therapy with a psychological professional (12.1% vs. 7.9%) in the past year, reflecting significant trends in care utilization.
- Electroconvulsive Therapy (ECT): ECT involves delivering small electric currents to the brain to induce a brief seizure, offering substantial relief for those grappling with severe depression and other psychological challenges. Current trends show a resurgence in the application of ECT, particularly for treatment-resistant depression, highlighting its effectiveness in clinical settings.
- Psychosurgery: While less common in modern practice, psychosurgery refers to surgical interventions on the brain aimed at addressing severe psychological disorders. This method is typically reserved for cases where other therapies have failed, emphasizing its role as a last resort.
- Transcranial Magnetic Stimulation (TMS): TMS is a non-invasive procedure that employs magnetic fields to stimulate nerve cells in the brain, primarily targeting depression. This innovative approach has gained traction due to its favorable safety profile and effectiveness, especially for individuals who do not respond to traditional treatments.
These approaches illustrate the essence of biomedical therapy, focusing on physiological interventions that aim to modify brain chemistry or structure to enhance psychological outcomes. Moreover, case studies have shown that combining peer support interventions with pharmacotherapy can improve adherence to care and overall effectiveness. Participants who received peer support during ERP therapy completed more therapy hours and reported better outcomes, emphasizing the importance of a comprehensive strategy for psychological care. This is particularly crucial in light of the alarming statistic that suicide was the second leading cause of death among adolescents aged 10-14 in 2021.
The integration of psychotherapy and pharmacotherapy is often preferred, as the combination of these methods can yield improved outcomes for individuals facing psychological challenges. If you or someone you know is navigating these difficulties, consider exploring these treatment options and discussing them with a healthcare professional who can provide guidance tailored to your needs.
The Role of Pharmacotherapy in Treatment
Pharmacotherapy stands as a cornerstone of biomedical therapy, serving as a primary option for various psychological disorders. Medications are thoughtfully designed to target specific neurotransmitters in the brain, which play a crucial role in the development of these disorders. For instance, selective serotonin reuptake inhibitors (SSRIs) are crafted to elevate serotonin levels, effectively alleviating symptoms of depression.
In contrast, antipsychotic medications work to manage symptoms of schizophrenia by modulating dopamine activity.
However, the effectiveness of pharmacotherapy can vary significantly; individual reactions to care may differ widely. Recent findings reveal that approximately 7.1% of children in major urban areas are prescribed medication for psychological concerns, with this figure rising to 12.1% in rural settings. This disparity emphasizes the importance of understanding the context in which pharmacotherapy is administered.
Notably, white children are the most likely to receive psychological support, while Asian children are the least likely, highlighting the urgent need for equitable access to care.
Moreover, exploring what biomedical therapy entails shows that pharmacotherapy's role extends beyond mere symptom management. Recent research highlights the effectiveness of mood stabilizers in treating bipolar disorder, with studies indicating that certain medications can lead to significant improvements in mood regulation. For example, case studies suggest that while tricyclic antidepressants (TCAs) may be less effective than psychotherapy, SSRIs demonstrate considerable positive effects on mental well-being outcomes.
A study titled "Impact of Treatment Type on Efficacy" assessed the effects of various psychotherapy and pharmacotherapy types on outcomes, revealing that therapy with TCAs was less effective than psychotherapy, while non-directive supportive counseling was also found to be less efficacious compared to pharmacotherapy.
Expert insights further illuminate the significance of pharmacotherapy in treating depression and anxiety disorders. Mental wellness experts, including Roger J. Zoorob, MD, emphasize that despite the availability of effective solutions, certain childhood anxiety disorders may persist into adulthood, necessitating a comprehensive strategy that incorporates medication alongside psychotherapy.
As the landscape of psychological care evolves, staying informed about the latest advancements in antidepressants and their applications is essential. The integration of pharmacotherapy with other therapeutic methods not only enhances efficacy but also empowers patients and practitioners to navigate the complexities of care more effectively.
Targeted Disorders: What Conditions Can Biomedical Therapy Address?
Biomedical treatment has proven beneficial for various psychological disorders, each requiring tailored strategies to achieve optimal results. In fact, 10.1% of U.S. adults have sought counseling or therapy from a mental health professional, underscoring the importance of mental health treatment in our society.
- Depression: This condition is often addressed through a combination of antidepressants and psychotherapy, leading to significant symptom reduction. Studies reveal that around 30% of individuals with depression respond well to pharmacotherapy alone, while many find greater relief through an integrated approach that includes therapy.
- Anxiety Disorders: Medications such as benzodiazepines and selective serotonin reuptake inhibitors (SSRIs) are frequently prescribed to manage anxiety symptoms. Research shows that SSRIs can alleviate anxiety symptoms in up to 60% of patients, establishing them as a core component of care.
- Bipolar Disorder: Effective management of bipolar disorder relies on mood stabilizers and antipsychotic medications, which are essential for controlling the manic and depressive episodes characteristic of the condition. Experts emphasize the importance of medication adherence to prevent relapse and maintain stability.
- Schizophrenia: Antipsychotic medications play a crucial role in managing symptoms such as hallucinations and delusions. Care protocols indicate that approximately 70% of patients experience a decrease in symptoms with appropriate pharmacotherapy.
- Obsessive-Compulsive Disorder (OCD): A combination of SSRIs and cognitive-behavioral techniques often proves effective. Evidence suggests that this dual approach can lead to symptom improvement in over 50% of individuals with OCD.
- Post-Traumatic Stress Disorder (PTSD): Both medications and counseling are employed to alleviate trauma-related symptoms. Recent statistics indicate that pharmacotherapy can be effective for about 40% of PTSD patients, especially when combined with trauma-focused therapy.
The consequences of psychological disorders, including suicide and disability, highlight the necessity for effective care alternatives. The report titled 'Mental Health Status in America' reveals that over 50 million adults face psychological disorders, with many not receiving the care they need. Additionally, 6.34% of young individuals in the U.S. reported a substance use disorder in the past year, amounting to over 1.5 million youth, which emphasizes the importance of addressing psychological issues in younger populations.
As Benjamin Zablotsky, Ph.D., noted, "Overall, as the extent of urbanization declined, the proportion of adults who had taken medication for their psychological well-being rose, while the percentage who had received counseling or support diminished." This observation highlights the connection between urbanization and access to care, further illustrating the role of biomedical therapy in tackling complex mental health issues and its vital contribution to enhancing patient outcomes across various disorders.
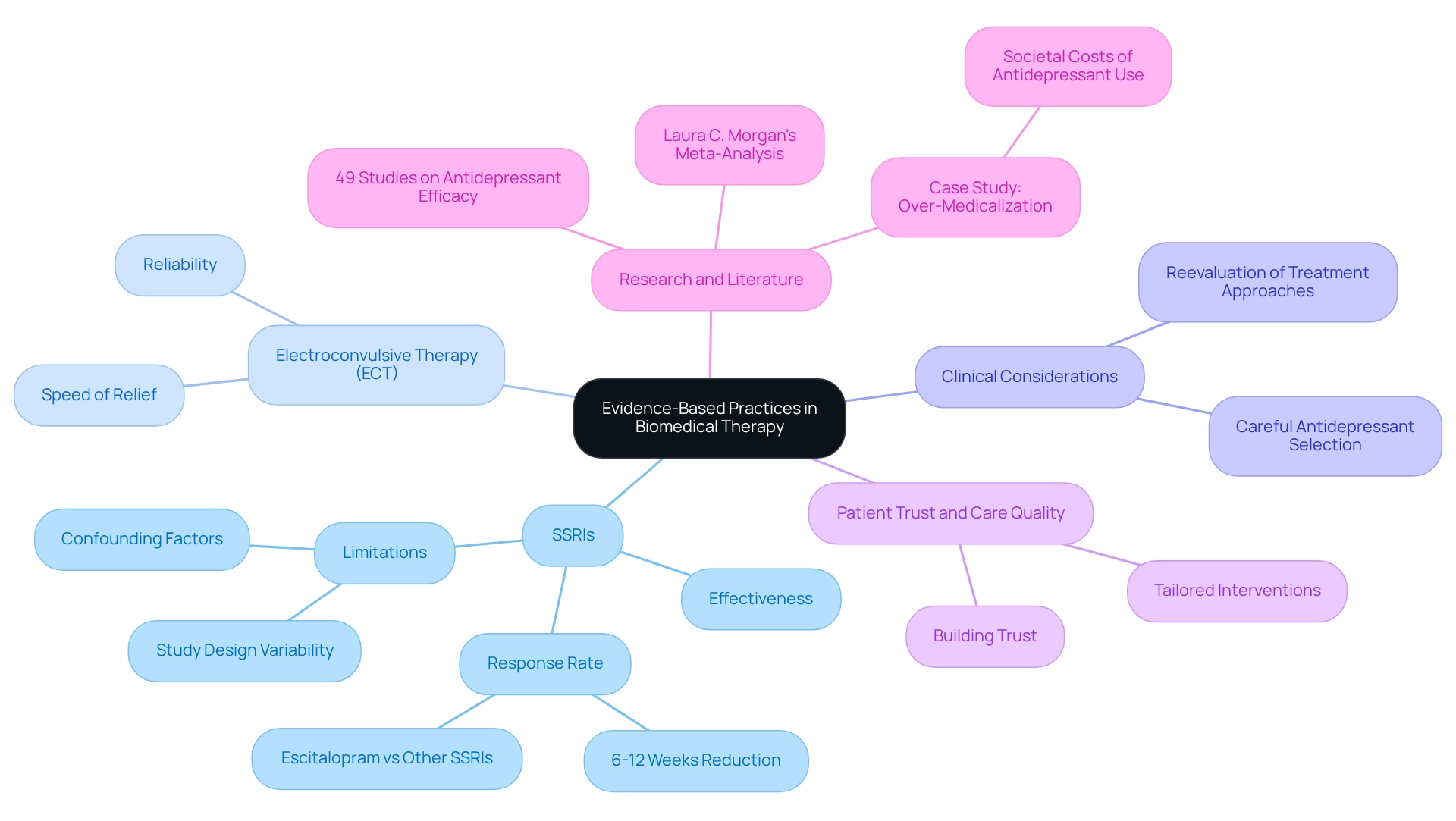
Evidence-Based Practices in Biomedical Therapy
Understanding what biomedical therapy entails is crucial, especially as evidence-based practices play a significant role in biomedical intervention. These practices ensure that methodologies are firmly rooted in rigorous scientific research. Recent meta-analyses have shown the effectiveness of selective serotonin reuptake inhibitors (SSRIs) in treating depression and anxiety disorders, revealing a noteworthy response rate among patients. For instance, research indicates that SSRIs can lead to a significant reduction in depressive symptoms within 6 to 12 weeks of therapy. However, it’s important to acknowledge the recognized lack of response at endpoint for Escitalopram compared to other SSRIs.
This underscores the importance of carefully selecting antidepressants in clinical settings. Moreover, electroconvulsive therapy (ECT) has emerged as a reliable and swift option for severe depression, providing essential relief for patients who may not respond to traditional pharmacological treatments. By incorporating these evidence-based practices, we not only enhance outcomes but also build trust between patients and healthcare providers.
By relying on established methodologies, practitioners can tailor interventions to meet the unique needs of their patients, ultimately improving the quality of care in mental health services. Understanding biomedical therapy also involves recognizing the growing adoption of evidence-based practices among healthcare providers and the shift towards scientifically validated approaches. This transition is particularly important in light of concerns about over-medicalization and the appropriate use of antidepressants, as highlighted in recent case studies. One case study points to the societal costs associated with antidepressant use, suggesting that a reassessment of care methods is necessary to ensure responsible prescribing practices.
Additionally, a literature search confirmed the inclusion of 49 studies comparing antidepressant efficacy, supporting claims about the effectiveness of SSRIs. However, it’s vital to recognize the limitations in study designs and potential confounding factors, as noted in recent research, to provide a balanced view of the evidence backing pharmacological interventions. As Laura C. Morgan emphasized in her meta-analysis, understanding the relative advantages and disadvantages of second-generation antidepressants is essential for making informed decisions in care.
Integrating Biomedical Therapy with Other Treatment Approaches
Combining biomedical interventions with other methods, such as psychotherapy, exemplifies the essence of biomedical therapy in providing a holistic approach to effectively address psychological disorders. For instance, the combination of pharmacotherapy and cognitive-behavioral therapy (CBT) has demonstrated significant improvements in treatment outcomes for individuals grappling with depression and anxiety. This integrative approach not only tackles biological symptoms through medication but also incorporates therapeutic interventions to target cognitive and behavioral patterns.
Moreover, collaborative care models that involve multidisciplinary teams play a crucial role in offering patients tailored support that meets their unique needs. These models encourage the integration of psychological and physical wellness services, enabling a more comprehensive assessment of psychological issues within primary care settings. As psychological challenges continue to rise, healthcare providers increasingly prefer adopting such models, recognizing their potential to enhance patient care.
A case study on the integrated behavioral wellness model highlights this trend, indicating that while implementing this model requires training and systemic modifications, it is favored by doctors and is anticipated to improve patient care, especially as psychological issues become more prevalent in our communities.
Current data reveals that the percentage of adults aged 18–44 residing in nonmetropolitan areas who received mental health assistance rose from 20.0% in 2019 to 25.2% in 2021. This underscores the growing acknowledgment of the importance of mental health care. By understanding the interplay among biological, psychological, and social elements, healthcare providers can devise more effective care strategies that enhance overall well-being, ultimately leading to better outcomes for patients. Real-world examples illustrate that combining pharmacotherapy with CBT not only alleviates symptoms but also nurtures resilience and coping strategies, paving the way for long-term recovery.
As Ben Fisher, creator of the video blog 'A String Of Hope,' emphasizes, "His dedication to sharing narratives of hope and resilience has positioned him as a credible and esteemed figure in the addiction recovery community," highlighting the importance of lived experiences in shaping effective support strategies. Furthermore, individuals with dual diagnosis disorders may face challenges such as severe mood swings and cognitive difficulties, further underscoring the necessity for a unified approach to psychological care.
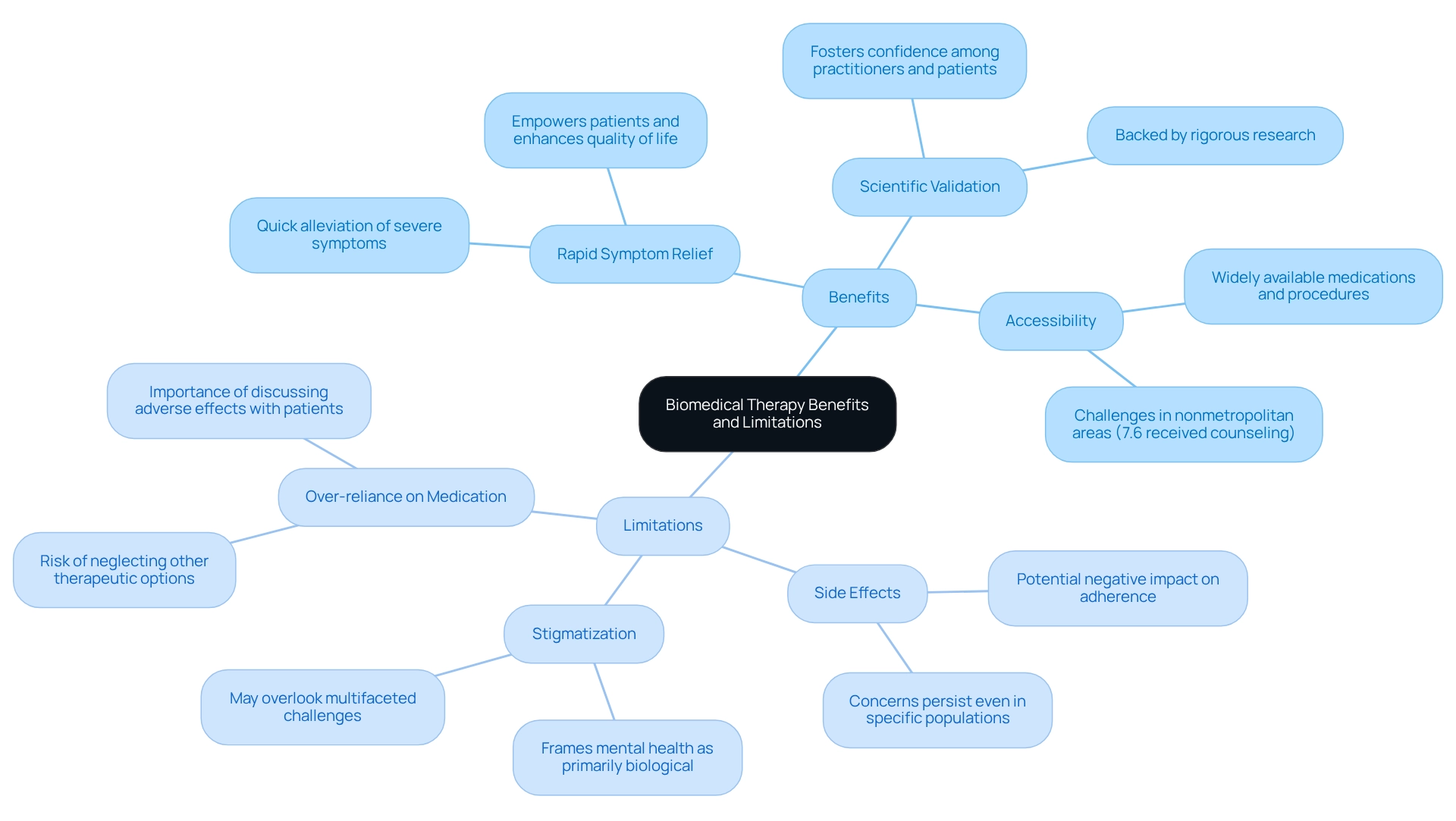
Benefits and Limitations of Biomedical Therapy
Biomedical therapy offers a variety of benefits that can profoundly influence mental health treatment.
- Rapid Symptom Relief: Many biomedical interventions, particularly medications, are crafted to deliver quick alleviation of severe symptoms. This swift response can empower patients, helping them regain functionality and enhancing their quality of life.
- Scientific Validation: The effectiveness of biomedical treatments is often backed by rigorous research, providing a solid foundation for their use in clinical settings. This scientific backing fosters confidence among both practitioners and patients.
- Accessibility: Medications and various biomedical procedures are typically widely available, ensuring that a diverse patient population can access these vital treatments. However, it's crucial to acknowledge that only 7.6% of adults residing in nonmetropolitan areas received counseling, underscoring the challenges faced by patients in these regions.
Yet, it is equally important to recognize the limitations tied to biomedical therapy:
- Side Effects: A significant concern arises from the potential side effects of many psychiatric medications, which can negatively impact patient adherence and overall well-being. Dima M. Qato observed that concerns regarding side effects persisted even when studies focused solely on adults with hypertension, emphasizing the importance of considering these effects in decision-making.
- Stigmatization: The biomedical model may unintentionally perpetuate stigma surrounding mental health disorders, often framing these conditions primarily as biological issues rather than multifaceted challenges.
- Over-reliance on Medication: There exists a risk that patients might become overly reliant on pharmacotherapy, potentially overlooking other essential therapeutic alternatives, such as psychotherapy, which can be crucial for comprehensive care. The case study titled 'Clinical Implications of Adverse Effects' illustrates how clinicians can weigh the robustness and quality of research evidence when discussing care options with patients, particularly concerning adverse effects that may vary in severity.
Moreover, recent discoveries emphasize the need for doctors to discuss the potential for depression with patients prescribed medications that may have depression as a possible adverse effect, further highlighting the necessity for a balanced approach.
Understanding the essence of biomedical therapy, along with its advantages and drawbacks, is vital for both patients and practitioners as they navigate the complexities of mental health care. The ongoing dialogue surrounding the effectiveness and implications of biomedical interventions continues to evolve, bringing renewed hope for the development of innovative psychiatric medications that may enhance outcomes while addressing these challenges.
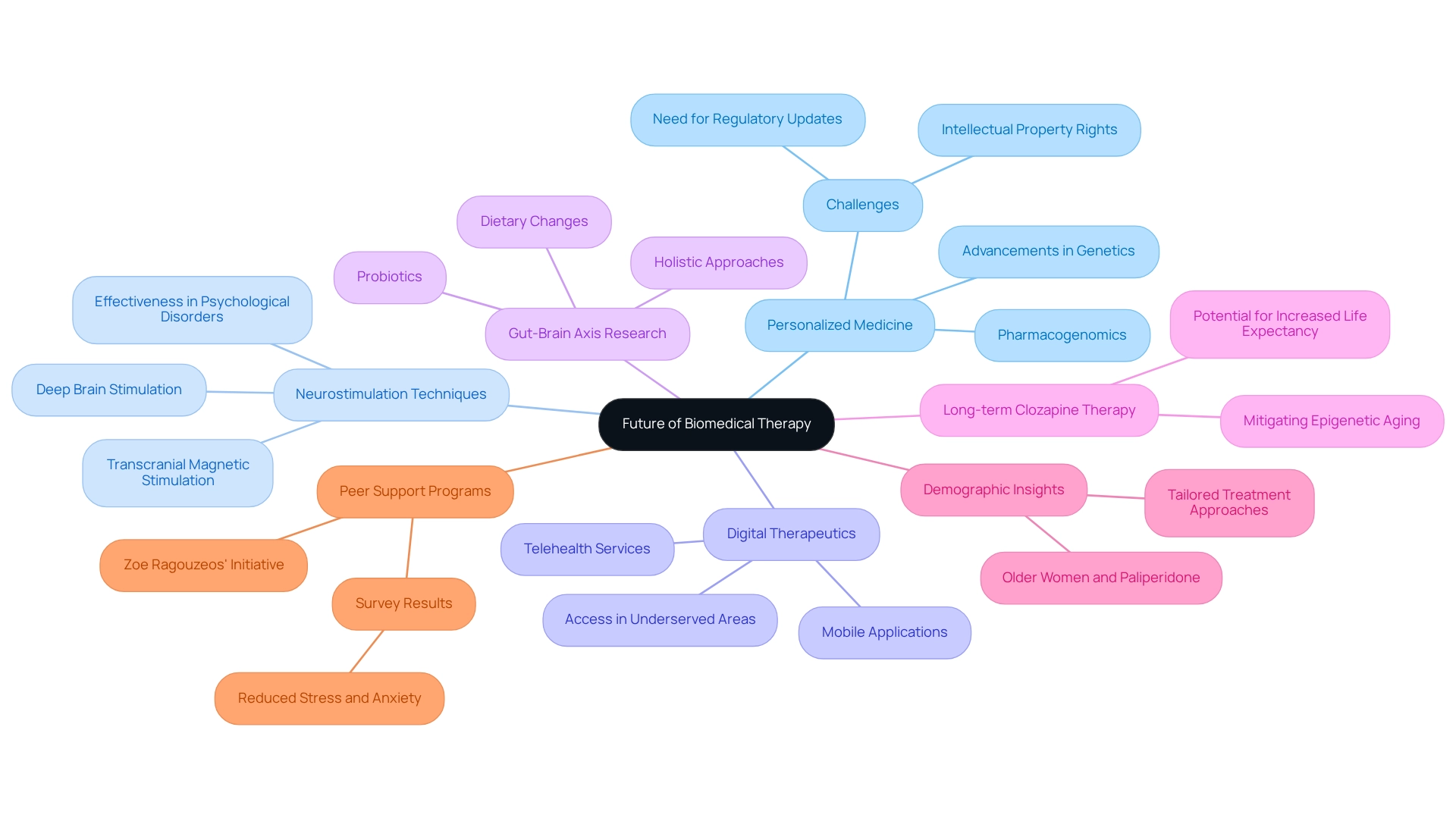
The Future of Biomedical Therapy: Trends and Innovations
The future of biomedical therapy is poised for transformative advancements, driven by ongoing research and technological innovations. As we explore these key emerging trends, it becomes clear that they not only promise to enhance patient care but also address the emotional and psychological needs of individuals seeking support.
- Personalized Medicine is at the forefront of this evolution. With advancements in genetics and pharmacogenomics, tailored treatments are being developed that consider individual genetic profiles. This approach aims to improve effectiveness while minimizing side effects, ultimately enhancing patient outcomes. However, it's important to acknowledge the challenges, such as intellectual property rights concerns, that may limit access to these advancements. This highlights the need for updates to regulatory laws, ensuring that everyone can benefit from personalized medicine.
- Next, we have Neurostimulation Techniques. Methods such as deep brain stimulation and transcranial magnetic stimulation are gaining recognition as potential therapies for a broader range of psychological disorders. Research shows that these techniques can significantly alleviate symptoms in individuals who have not responded to conventional treatments, underscoring their potential in medical settings.
- The rise of Digital Therapeutics is also noteworthy. The integration of technology in psychological care, through mobile applications and telehealth services, is transforming access to biomedical therapies. These digital solutions not only foster greater patient involvement but also provide essential support for those seeking wellness resources, especially in underserved areas. This shift emphasizes the importance of understanding what biomedical therapy can offer.
- Moreover, ongoing Research on the Gut-Brain Axis is revealing fascinating connections between gut health and psychological well-being. Emerging evidence suggests that dietary changes and probiotics may offer new avenues for treatment, highlighting the need for holistic approaches in mental health care.
- Recent findings regarding Long-term Clozapine Therapy are particularly significant. Evidence suggests that this therapy may mitigate epigenetic aging in male patients with psychotic disorders, potentially extending life expectancy. This underscores the importance of considering long-term treatment strategies within the realm of biomedical therapy.
- Additionally, Demographic Insights reveal that older women have higher concentrations of long-acting injectable paliperidone compared to younger women and men of all ages. This finding emphasizes the necessity for tailored approaches that account for demographic differences in treatment.
- Lastly, Peer Support Programs are emerging as innovative methods to enhance psychological well-being. The program initiated by Zoe Ragouzeos at New York University exemplifies the power of organized support. As Ragouzeos insightfully noted, "It is our responsibility to find ways to engage students in helping each other and ensure they have the right resources to support one another safely."
These trends reflect a significant shift towards more comprehensive and personalized strategies in wellness care, showcasing an evolving understanding of the complexities surrounding psychological disorders. As the landscape of biomedical therapy continues to evolve, integrating these advancements promises to enhance care quality and improve outcomes for individuals facing mental health challenges.
Conclusion
The exploration of biomedical therapy reveals its essential role in addressing mental health disorders through various methods, including:
- Pharmacotherapy
- Electroconvulsive therapy
- Psychosurgery
This multifaceted approach not only underscores the biological foundations of mental health issues but also highlights the need for tailored interventions that cater to diverse populations. As we consider the statistics, it becomes clear that significant treatment gaps persist, particularly among marginalized groups, emphasizing the urgent need for effective and equitable mental health care.
Integrating biomedical therapy with psychotherapy and other treatment modalities further enhances its effectiveness. This combination allows healthcare providers to address both the physiological and psychological aspects of mental health disorders. Evidence-based practices continue to validate the efficacy of these approaches, ensuring that treatments are grounded in rigorous research. However, it is crucial to stay mindful of the limitations and potential side effects associated with biomedical interventions, as well as the risk of over-reliance on medication.
Looking ahead, the future of biomedical therapy is promising, characterized by innovations such as:
- Personalized medicine
- Neurostimulation techniques
- Digital therapeutics
These developments aim to create more individualized and accessible treatment options, ultimately improving outcomes for those affected by mental health disorders. As the landscape of mental health care evolves, our commitment to integrating advanced methodologies with compassionate care will be vital in shaping a more effective and inclusive approach to mental health treatment. Together, we can foster a community that supports one another in navigating these challenges.
Frequently Asked Questions
What is biomedical therapy?
Biomedical therapy is an approach that utilizes physiological methods to address psychological disorders. It includes various techniques such as medications, medical procedures, and other biological interventions aimed at alleviating psychological symptoms.
How does biomedical therapy differ from conventional psychotherapy?
Unlike conventional psychotherapy, which focuses on behavioral and cognitive aspects, biomedical therapy emphasizes the biological foundations of psychological conditions, operating under the belief that many psychological disorders have physiological origins that can be treated through medical interventions.
What are some common methods used in biomedical therapy?
Common methods in biomedical therapy include pharmacotherapy (medications), electroconvulsive therapy (ECT), psychosurgery, and transcranial magnetic stimulation (TMS).
What is pharmacotherapy?
Pharmacotherapy is the most prevalent form of biomedical treatment that employs medications to alleviate symptoms associated with psychological disorders. Common medication classes include antidepressants, antipsychotics, and mood stabilizers.
What is electroconvulsive therapy (ECT) and when is it used?
ECT involves delivering small electric currents to the brain to induce a brief seizure, providing substantial relief for those with severe depression and other psychological challenges, especially for treatment-resistant depression.
What is psychosurgery and when is it considered?
Psychosurgery refers to surgical interventions on the brain aimed at addressing severe psychological disorders. It is typically reserved for cases where other therapies have failed and is considered a last resort.
What is transcranial magnetic stimulation (TMS)?
TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, primarily targeting depression. It has gained traction due to its favorable safety profile and effectiveness for individuals who do not respond to traditional treatments.
What role does peer support play in biomedical therapy?
Combining peer support interventions with pharmacotherapy can improve adherence to care and overall effectiveness, as participants who received peer support during therapy reported better outcomes.
What is the significance of integrating psychotherapy and pharmacotherapy?
The integration of psychotherapy and pharmacotherapy is often preferred because combining these methods can yield improved outcomes for individuals facing psychological challenges.
Why is understanding biomedical therapy important?
Understanding biomedical therapy is crucial for addressing the unique needs of diverse populations and enhancing the effectiveness of treatments for psychological disorders, particularly given the prevalence of mental health issues.




