Introduction
The intersection of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) presents a nuanced challenge in the realm of mental health. Misdiagnoses and misinterpretations of symptoms can have significant impacts on individuals, particularly autistic women who are more prone to being misdiagnosed with BPD. To address this issue, accurate identification and understanding of ASD as a lifelong condition are crucial in fostering supportive environments.
Additionally, research highlights the need for healthcare systems to address the comprehensive care requirements of autistic individuals. This article explores the complexities of misdiagnosis, the importance of accurate assessment and diagnosis, treatment strategies, and emerging research in the field. By staying informed and understanding the clinical intricacies of these dual diagnoses, healthcare professionals can deliver the highest quality of care to those they serve.
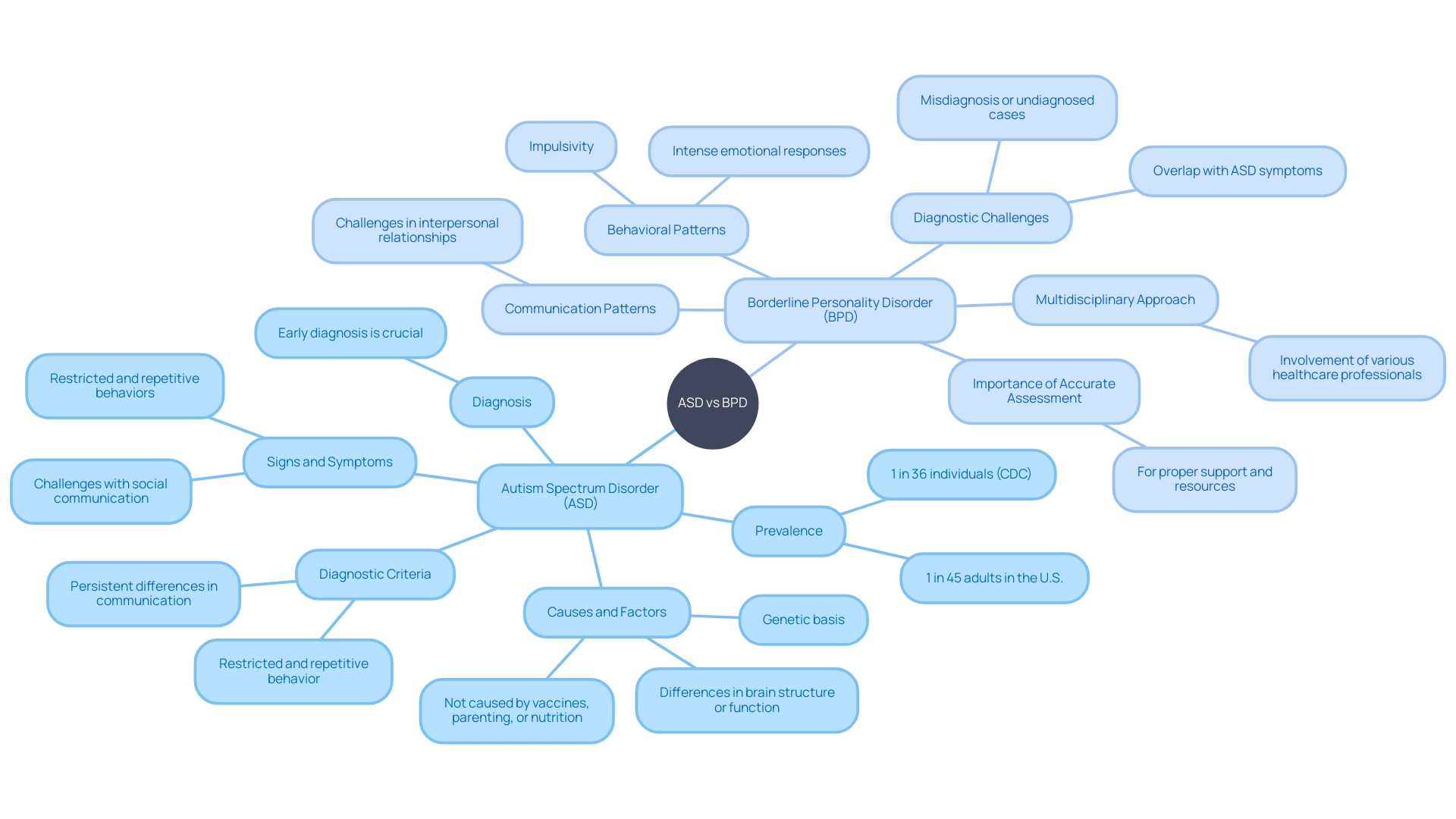
Understanding BPD and Autism
The intersection of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) presents a nuanced challenge in the realm of mental health. Bree Conklin's experience highlights the complexity of this issue, having lived with a misdiagnosis of BPD until the age of 34, only to later be correctly diagnosed with autism. Such cases are not isolated events, as the overlapping symptoms between the two conditions can lead to misinterpretations and incorrect treatment approaches.
Dr. Megan Neff, who herself was diagnosed with autism in adulthood, emphasizes that although co-occurrence of ASD and BPD is possible, it is a rarity. The misinterpretation of an autistic individual's responses as BPD symptoms is a more frequent occurrence, particularly among autistic women who are more prone to being misdiagnosed with BPD, significantly impacting their mental health and well-being.
According to the study published in Borderline Personality Disorder and Emotion Dysregulation, BPD is characterized by profound emotional instability, impulsive behaviors, and tumultuous relationships. The condition manifests through severe mood swings, fear of abandonment, and a distorted self-image. Dissociation and emotion dysregulation are also key features, intensifying the complexity of differentiating it from ASD.
This confusion in diagnosis underscores the critical need for careful evaluation using standardized assessment tools to ensure accurate identification and appropriate therapeutic interventions.
The implications of such misdiagnoses are far-reaching, affecting not only the mental health of individuals but also their social interactions and overall quality of life. Misunderstandings about autism can lead to inadequate support structures for those affected, as noted by experts in the field. Accurate recognition and understanding of ASD as a condition that persists across a person's lifespan are essential in fostering supportive environments for individuals on the spectrum.
This knowledge empowers those around them, including friends, educators, and colleagues, to provide the necessary support.
Moreover, research indicates that autistic individuals face a higher risk of co-occurring mental and physical health issues, along with an increased mortality rate. Studies utilizing population-based data reveal a significant health gap for autistic individuals, emphasizing the urgent need for healthcare systems to address their comprehensive care requirements more effectively. The personal narratives of women like Bree Conklin and professionals like Dr. Megan Neff serve as a poignant reminder of the critical importance of precise diagnosis and informed treatment strategies in enhancing the lives of those with autism and co-occurring conditions.
Case Study: Misdiagnosis of Autism as Borderline PD
The journey toward a correct diagnosis for autism spectrum disorder (ASD) can be fraught with missteps, as evidenced by the experiences of individuals such as Bree Conklin. Initially misidentified as having borderline personality disorder (BPD), Conklin finally received an ASD diagnosis at the age of 34. This is not an isolated incident; the overlap in symptoms between ASD and BPD can lead to misdiagnoses, especially in women, with profound implications for treatment plans.
Dr. Megan Neff, who herself was diagnosed with autism later in life, underscores that while comorbidity exists, it's relatively uncommon. Instead, it is more likely that behaviors associated with autism are mistakenly classified as BPD characteristics. The distinction between the two is critical, as it informs the approach to support and intervention.
The Centers for Disease Control and Prevention (CDC) describe autism as a condition with a spectrum of symptoms that can affect communication, behavior, and socialization. Recognizing autism's hallmark signs, such as difficulties with social interaction or rigid adherence to routines, is essential for early and accurate diagnosis. However, there is no medical test for ASD, which makes observational assessment of behavior and development pivotal.
The implications of delayed or mistaken diagnosis can be severe. For instance, autistic women often grapple with higher rates of depression, and an inaccurate diagnosis can exacerbate these challenges. Moreover, understanding that both autism and ADHD are neurodevelopmental differences, not illnesses to be cured, is fundamental.
This perspective is supported by the National Autistic Society, which emphasizes the social challenges and unique sensory responses associated with autism.
With early diagnosis, individuals can access resources and opportunities to thrive. Research is ongoing to unravel the genetic factors contributing to ASD. Brain scans have revealed structural differences in individuals with autism, hinting at a genetic underpinning, despite common misconceptions about causes such as vaccines.
Machine learning technologies are emerging as promising tools for enhancing ASD detection, offering hope for improved quality of life through prompt intervention and support.
Mechanisms in Misdiagnosis
Clinicians face a complex challenge when assessing individuals who may present with symptoms common to both Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD). These overlapping symptoms can lead to misdiagnoses, affecting the treatment and support provided. For Angeleena O'Connor, who had the police called to her house more than 40 times, including a violent incident, understanding the difference between these conditions could have altered her path significantly.
Similarly, Bree Conklin was misdiagnosed with BPD for years before her correct diagnosis of autism at age 34, reflecting a broader trend where autistic women are often misinterpreted as having BPD. Dr. Megan Neff, a psychologist diagnosed with autism later in life, highlights that while it's possible to have both conditions, it's quite rare. This distinction is crucial as intervention strategies for ASD differ greatly from those for BPD.
The concept of neurodiversity recognizes this difference, championing individual brain variations. As research progresses, machine learning technologies are being employed to enhance diagnostic accuracy for ASD, potentially improving life quality for individuals and their families by allowing for timely interventions. The use of classification models and clustering methods to analyze ASD datasets represents a promising advancement in the field, with researchers rigorously testing these models to achieve the best results and sharing their findings for future study.
Comprehensive Assessment and Diagnosis
Understanding the nuances between Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) is critical for accurate diagnosis and treatment. The process incorporates a variety of assessment tools and diagnostic criteria, which are pivotal in distinguishing between the two. For ASD, the American Psychiatric Association's Diagnostic and Statistical Manual (DSM-5) outlines specific communication and behavioral patterns for diagnosis, including persistent differences in social interaction and restricted, repetitive behaviors.
It's important to acknowledge the spectrum nature of ASD, which manifests differently in each individual, affecting them to various degrees. The recent statistics highlight the prevalence of autism, with 1 in 36 individuals being on the spectrum. Early diagnosis is key as it connects individuals with vital resources that can significantly improve quality of life.
On the other hand, mental health disorders like BPD have their own set of diagnostic challenges and criteria, which may include symptoms such as mood changes and poor judgment. The phenomenon of Bulimia Nervosa is mentioned to emphasize the complexity of diagnosing mental health conditions, which often entails identifying a pattern of behavior like binging and purging.
A multidisciplinary approach is essential for a thorough evaluation, as it brings together the expertise of various healthcare professionals. This collaborative effort ensures that the assessment is comprehensive, considering the individual's unique symptoms and behaviors. The insights from a Board-Certified Behavior Analyst, with over a decade of clinical knowledge, support the significance of coordinated care and the use of technology to streamline the diagnostic process.
While the medical model for autism testing has its flaws, resulting in many adults receiving inconclusive results, self-diagnosis is a respected option within the autistic and neurodivergent community. Some individuals may choose to undergo formal diagnosis to access certain supports or for personal reasons, as was the case with a Canadian who sought diagnosis to ensure equitable opportunities for their children.
Accurate assessment and diagnosis are the cornerstones of equipping individuals with the understanding and support they need. Whether through formal testing or self-identification, recognizing and addressing the needs of individuals with ASD or BPD is crucial for their well-being and integration into society.
Treatment and Outcomes
Navigating the complexities of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) can be challenging, especially when they co-occur. A personalized approach is crucial, as evidenced by interventions like hyperbaric oxygen therapy, which, in one case, significantly improved a young boy's ADHD and Asperger's symptoms. Individualized treatments, which consider unique histories and symptoms, can lead to remarkable progress.
For example, a BPD diagnosis in a military veteran revealed underlying trauma and stress, highlighting the need for treatments that address not just symptoms but also root causes. Embracing evidence-based therapies, such as Dialectical Behavior Therapy (DBT), which validates deep emotions rather than dismissing them, can foster better outcomes. The Kevin and Avonte Program further exemplifies targeted support, focusing on preventing wandering, a serious issue in the ASD community.
With approximately 1 in 54 children in the US affected by ASD, understanding and addressing the spectrum of symptoms through individualized care and continuous evaluation is imperative for improving lives.
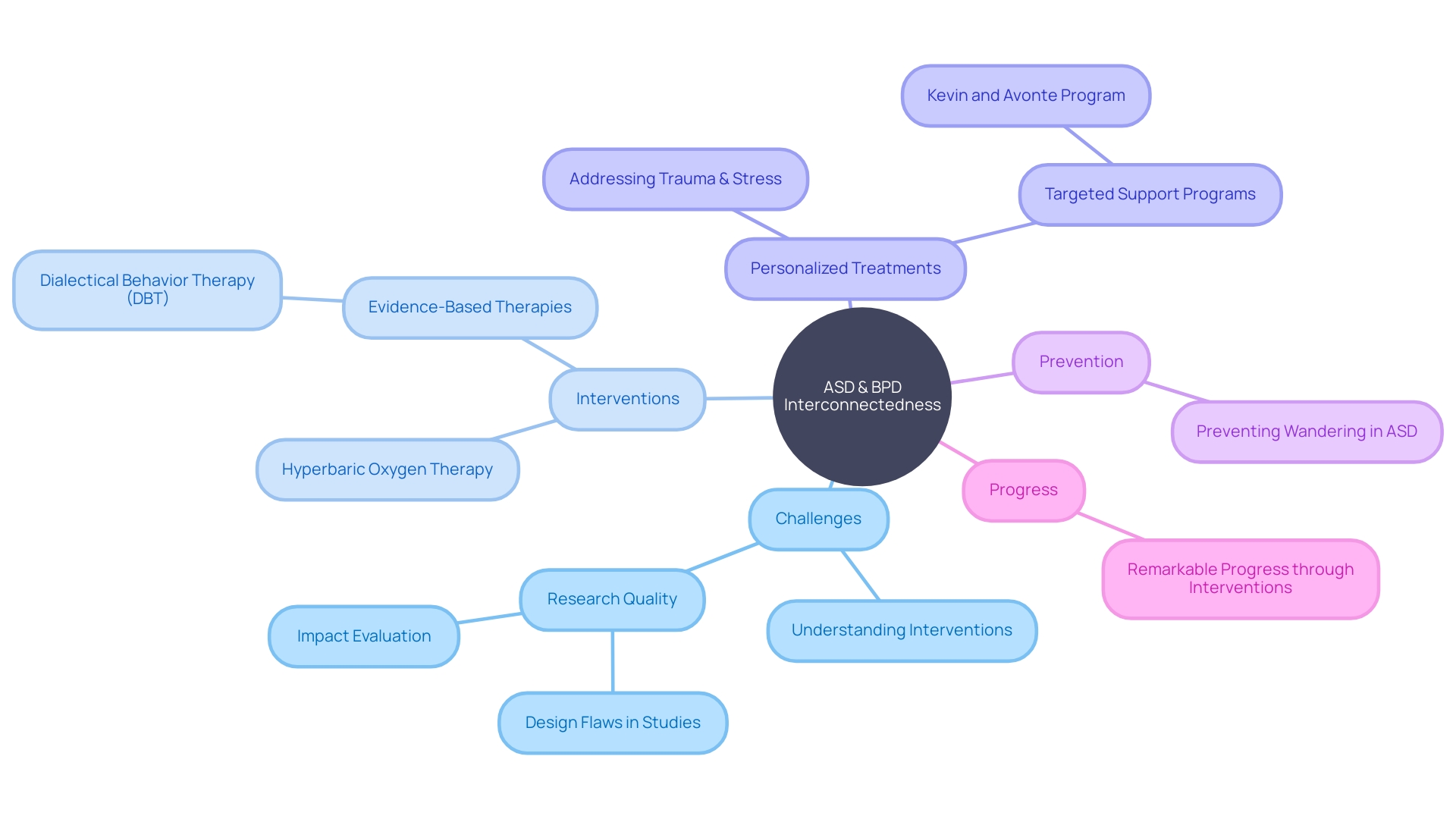
Clinical Challenges and Emerging Research
Healthcare professionals specializing in mental health face a unique set of clinical challenges when providing care to individuals diagnosed with both Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD). These challenges are compounded by the intricacies of ASD, which is characterized by a spectrum of behaviors that affect individuals differently and to varying degrees. Statistics indicate that ASD is more common than previously thought, with current estimates suggesting that as many as 1 in 36 individuals are affected, underscoring the importance of early diagnosis and intervention.
The intersection of ASD and BPD requires a nuanced approach to care, as evidenced by research from various fields. A synthesis of 58 publications reveals the complexity of co-occurring ASD and BPD, highlighting the need for comprehensive research to better understand the prevalence, impact, and effective treatment strategies for this dual diagnosis. The research underscores the significant time investment required by medical care providers, who spend over half of their time on administrative tasks, such as documenting medical visit notes.
This administrative burden detracts from patient care and contributes to professional burnout.
Emerging findings in the field point to the genetic underpinnings of ASD, with brain scans illustrating structural differences in individuals with ASD compared to neurotypical development. This genetic focus is critical, as it dispels misconceptions about the causes of ASD and directs attention towards hereditary and medical factors. Moreover, recent ethical considerations, particularly in the realm of neurodiversity research involving human brain organoids transplanted into animals, have sparked discussions about the implications of such studies for understanding cognitive disorders like ASD.
With the goal of improving the life outcomes for individuals with ASD, initiatives are being developed to address the employment challenges faced by this population. Autistica estimates that only 3 in 10 working age autistic individuals are employed, despite a strong desire to work among this group. Studies indicate that autistic people face the largest pay gap of all disability groups, earning a third less than non-disabled individuals.
This highlights the need for continued efforts to raise awareness, reduce stigma, and support the inclusion of autistic individuals in the workforce.
In light of these challenges, it is essential for healthcare professionals to stay informed about the evolving landscape of ASD research and practice. By understanding the clinical intricacies of dual diagnoses such as ASD and BPD, and by keeping abreast of the latest research developments, professionals can deliver the highest quality of care to those they serve.
Conclusion
In conclusion, accurate assessment and diagnosis are crucial for addressing the complexities of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD). Misdiagnoses can have significant impacts, especially on autistic women who are often misdiagnosed with BPD. Healthcare professionals must have a comprehensive understanding of both conditions to provide appropriate support and intervention.
The healthcare system needs to address the comprehensive care requirements of autistic individuals, who face a higher risk of co-occurring mental and physical health issues. Personalized treatment strategies, such as Dialectical Behavior Therapy (DBT) and targeted support programs, can lead to better outcomes.
Staying informed about emerging research is essential. Understanding the genetic underpinnings of ASD, the impact of brain scans, and the potential of machine learning technologies can enhance diagnostic accuracy. Efforts to raise awareness, reduce stigma, and support the inclusion of autistic individuals in the workforce are crucial for their well-being and integration.
By staying informed and understanding the clinical intricacies of these dual diagnoses, healthcare professionals can deliver high-quality care to individuals with ASD and BPD. Accurate assessment, diagnosis, and personalized treatment strategies are vital for fostering supportive environments and ensuring the well-being and integration of individuals on the spectrum.




