Introduction
Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) are complex conditions that can significantly impact individuals' lives. Understanding the nuances of these disorders is crucial for accurate diagnosis and effective support. This article explores the overlapping characteristics, diagnostic challenges, and implications for treatment and support in individuals with ASD and BPD.
By delving into real-life examples and considering the unique needs of each individual, we can work towards a more inclusive and empowering approach that honors the diversity within these communities. Join us as we navigate the complexities of ASD and BPD and explore strategies to ensure the well-being of individuals and their families.
Understanding Autism Spectrum Disorder (ASD)
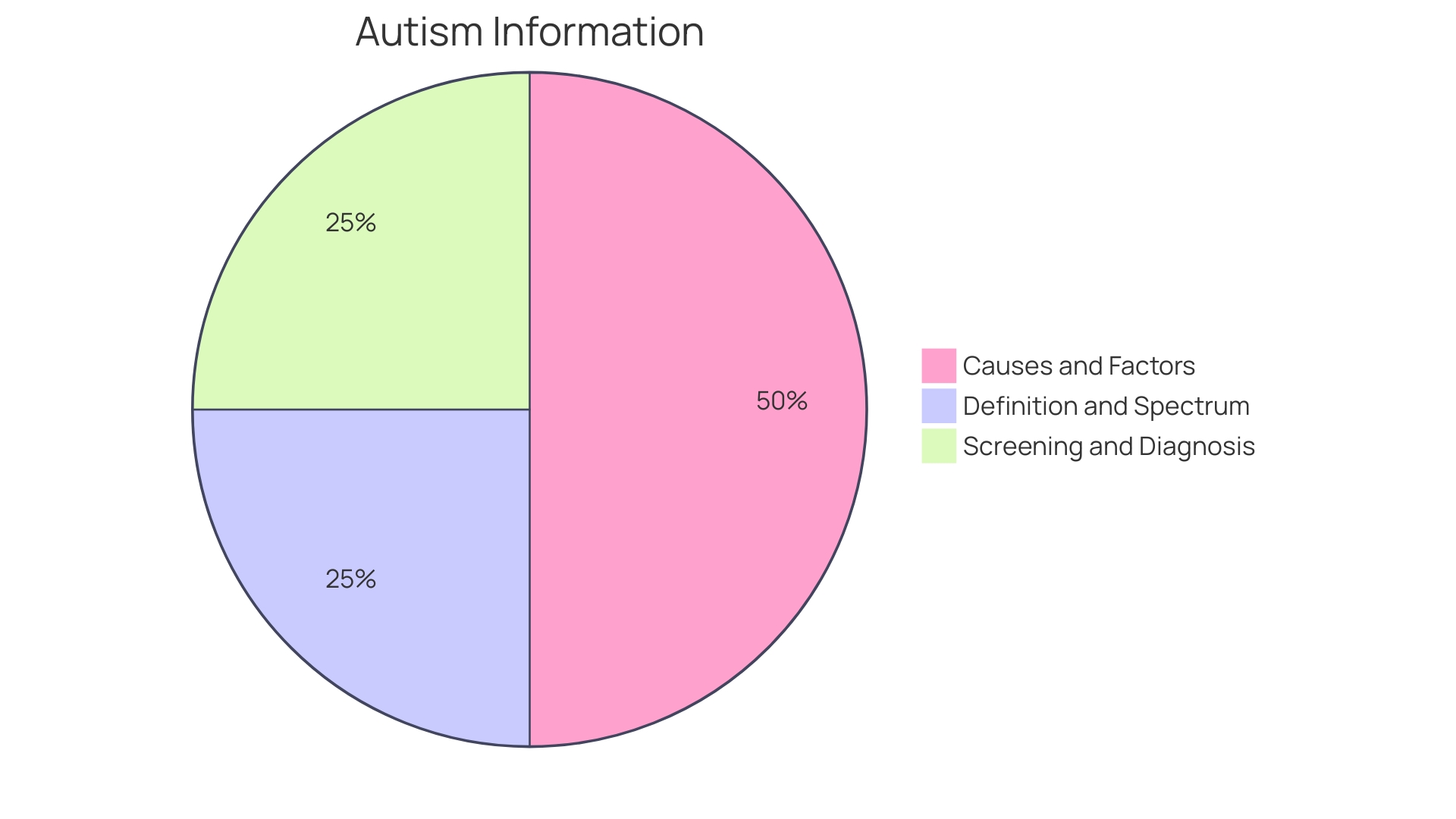
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition recognized for its wide-ranging effects on social interaction, communication abilities, and behavior. Individuals with ASD may exhibit a variety of symptoms and abilities, as the condition manifests uniquely from person to person. The American Psychiatric Association outlines the diagnostic criteria for ASD in the DSM-5, which includes persistent challenges in social communication across multiple contexts and the presence of restricted, repetitive patterns of behavior or interests. For instance, individuals might repeat certain phrases, show an intense focus on specific topics, or display a heightened sensitivity to sensory input.
Recent studies, including a notable case involving dizygotic twins with level 3 severity ASD requiring substantial support, underscore the genetic components of ASD and the importance of early diagnosis. These twins, like all individuals with ASD, displayed unique characteristics despite their shared environment, highlighting the spectrum nature of the disorder. With an estimated prevalence as high as 1 in 36 individuals according to the CDC, understanding ASD's genetic underpinnings is critical. Brain scans have revealed structural differences in individuals with ASD, and ongoing research continues to explore genetic theories, dispelling misconceptions such as the discredited notion that vaccines cause autism.
Moreover, the conversation around ASD is evolving, with experts advocating for precise, non-eponymous terminology that respects the diversity and individuality of those affected. As knowledge about ASD grows, so does awareness of its multifaceted impact on individuals' lives, leading to a greater understanding and support for those on the spectrum and their families.
Understanding Borderline Personality Disorder (BPD)
Borderline Personality Disorder (BPD) presents as a complex mental health challenge with symptoms that can significantly disrupt an individual's emotional regulation, self-image, and ability to maintain relationships. Often misunderstood, BPD is marked by a pattern of intense mood swings, impulsivity, and a profound struggle with self-identity. The emotional turbulence of BPD can lead to severe and unstable interpersonal relationships.
Those living with BPD, like Imogen, confront the daily realities of managing symptoms such as 'splitting'—seeing things as all good or all bad—and dissociation, a disconnection between thoughts, identity, consciousness, and memory. The journey towards understanding and managing BPD is deeply personal, and narratives like Imogen's underscore the importance of destigmatizing the condition and advancing supportive treatments.
Dr. Daniel J. Fox has dedicated his career to changing perceptions of BPD, advocating for approaches that focus on core issues rather than just symptoms. His methods aim to simplify treatment, reduce behaviors that hinder therapy, and foster stronger therapeutic relationships, ultimately improving client retention and outcomes.
Stigma surrounding BPD remains one of the greatest barriers to seeking help. Misconceptions and stereotypes contribute to individuals feeling shame, which only compounds their struggles. The severity of the disorder is underscored by the fact that approximately 80% of those with BPD will attempt suicide in their lifetime, with up to 10% succumbing to suicide.
However, there is hope. Research has illuminated a more optimistic trajectory for BPD than previously believed. Studies, including one in the American Journal of Psychiatry, have shown that with appropriate treatment, individuals can experience significant quality of life improvements. For instance, after two years of treatment, about half of the study's participants no longer met the criteria for BPD, and a decade later, the rate of recovery improved to 85%, although some continued to face psychosocial challenges.
Understanding BPD is crucial, not just for those who live with it but also for mental health professionals, family members, and the wider community. By addressing the stigma and supporting effective treatment pathways, there is a potential for individuals with BPD to lead fulfilling lives, contributing richly to society while managing their mental health concerns.
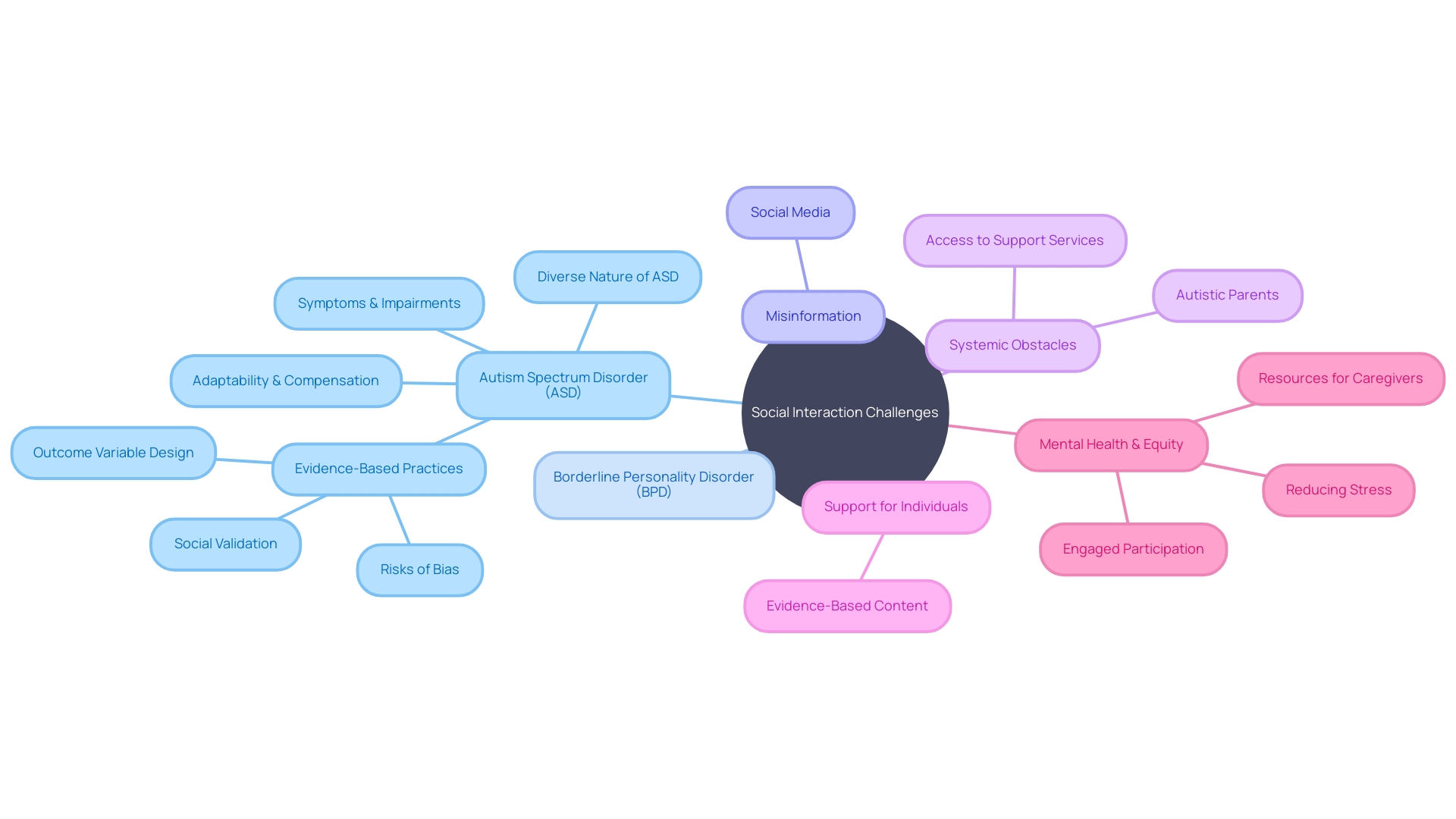
Overlapping Characteristics: Social Interaction Challenges
Understanding the intricacies of social interaction challenges is essential in the context of autism spectrum disorder (ASD) and borderline personality disorder (BPD). Both ASD and BPD are marked by hurdles in creating and sustaining interpersonal relationships, yet the roots and expressions of these obstacles are distinct. Studies examining autistic adolescents have highlighted that mood disorders within this demographic can exhibit through various behaviors, from moral distress to communication impairments. Dr. Katie Maras, with over five years of research into supporting autistic adults, points out that autistic individuals may struggle with perspective-taking and recounting events due to language and social communication issues.
The complexity of social interactions for individuals with ASD is further underscored by the diverse nature of the condition itself. ASD is a spectrum, presenting a range of symptoms and impairments that require tailored approaches for each individual. In light of this, educational and human services settings have adopted methodologies like functional behavioral assessment to determine the environmental triggers of challenging behavior, allowing for more personalized interventions.
The reach of autism information on social media, particularly platforms like TikTok, has raised concerns about the spread of misinformation. Giacomo Vivanti from Drexel University emphasizes the double-edged sword of social media's broad reach: while it can educate the public, it can also propagate inaccuracies. This highlights the importance of accurate, evidence-based content to support those with autism and their families.
In their efforts to support their children, parents, particularly those who are autistic themselves, often encounter systemic obstacles rather than individual failings within support services. Interviews with autistic mothers of children in mainstream education revealed a need to advocate fiercely for appropriate support, echoing the experiences of non-autistic parents.
The profound adaptability and compensation strategies employed by autistic individuals, often unseen by society, reveal the depth of their efforts to navigate a world not designed for them. This 'compensation' involves both conscious and unconscious tactics to align with neurotypical behaviors, highlighting the resilience of the autistic community.
The evidence-based practices to support people with autism are under constant scrutiny for biases and the true effectiveness of interventions. These practices include social validation to gauge community perspectives on the interventions and monitoring for any adverse effects, ensuring that the outcomes bring meaningful, lasting changes to individuals with ASD.
In understanding the social interaction challenges in ASD and BPD, it is crucial to acknowledge these differences and similarities, which can pave the way for more effective support and interventions tailored to the unique needs of each individual.
Overlapping Characteristics: Sensory Sensitivities
Sensory processing challenges are a central feature of autism spectrum disorder (ASD), profoundly affecting many individuals' daily experiences. Those with ASD may grapple with hypersensitivity, leading to overwhelming responses to stimuli that others might find innocuous. Conversely, hyposensitivity can result in a muted reaction, leaving some sensory inputs almost unnoticed. These sensitivities extend across a range of senses, including visual, auditory, tactile, and even proprioceptive cues, encompassing one's sense of balance and body awareness.
In a similar vein, sensory sensitivities can also be present in individuals with Borderline Personality Disorder (BPD), although the manifestation and impact can differ significantly. This variance underscores the importance of recognizing the unique sensory profiles of each individual. The intersection of sensory sensitivities in both ASD and BPD raises questions about the underlying neural mechanisms and how they influence each condition's expression.
Exploring these sensory dimensions further, research has highlighted the occurrence of synesthesia in individuals with ASD, where sensory stimulation in one modality may involuntarily trigger an additional sensory experience in another. This phenomenon adds another layer of complexity to the sensory world of some individuals with autism.
Moreover, innovative approaches like Design Thinking (DT) have been employed to better understand and address the needs of autistic children in healthcare settings. By fostering a deep empathy and adopting a collaborative, solution-focused methodology, DT aims to improve participation and experiences during healthcare visits for those with sensory sensitivities.
Recognizing the diversity and intensity of sensory experiences in ASD, it's evident that each person's sensory profile is as unique as their fingerprint. These insights not only enhance our comprehension of ASD and its overlap with conditions like BPD but also pave the way for more personalized and effective support strategies, ensuring that sensory needs are met with understanding and care.
Misdiagnosis and Challenges
Understanding the nuanced differences between autism and Borderline Personality Disorder (BPD) is critical for delivering correct diagnoses and effective interventions. Both conditions share similar symptoms, such as difficulties in social interaction and emotional regulation, which can easily lead to misdiagnosis. For families like those at MacDill Air Force Base, where access to specialized support through the Exceptional Family Member Program proved challenging, the stakes of misidentification are high. A mother recounts her struggle with bureaucratic obstacles when her son's autism was not accommodated at the local school, underscoring the importance of precise identification and support.
The advent of social media and platforms like TikTok has expanded access to information about autism, but with this comes the risk of misinformation. As Giacomo Vivanti of Drexel University highlights, while such platforms offer broad reach, the unfiltered content can propagate inaccuracies. This calls for better vetting of information and the development of reliable diagnostic tools.
Indeed, diagnosing ASD has traditionally leveraged parental insights and professional observations, guided by the DSM-5 criteria. Nonetheless, no single tool should be used in isolation. For instance, the Modified Checklist for Autism in Toddlers-Revised (M-CHAT-R/F) demonstrates varying degrees of effectiveness in different settings, indicating a pressing need for more accurate, objective, and scalable screening methods. A study of over 25,000 children revealed the M-CHAT-R/F's limitations, particularly in primary care contexts.
In light of these challenges, the push for innovation in diagnostic technology is gaining momentum. Machine learning models such as AutMedAI, which boasts an 80% accuracy rate for identifying children under two with autism, show promise in enhancing early detection.
It is essential to consider personal accounts and professional perspectives alongside emerging technologies to refine our approach to autism diagnosis. Only then can we ensure that individuals receive the tailored care and support they need to thrive.
Self-Harm Behaviors: Differences and Similarities
Self-harm is a critical issue among adolescents, with approximately 17% of teens reporting at least one instance in their lifetime. The average age for the first self-harm incident is alarmingly at 13 years old. These behaviors often arise from an inability to manage difficult emotions healthily, serving as a distraction or a cry for help. While self-harm is a complex behavior seen across various conditions, its manifestation in autism spectrum disorder (ASD) and borderline personality disorder (BPD) is particularly notable, with each having distinct motivations and expressions.
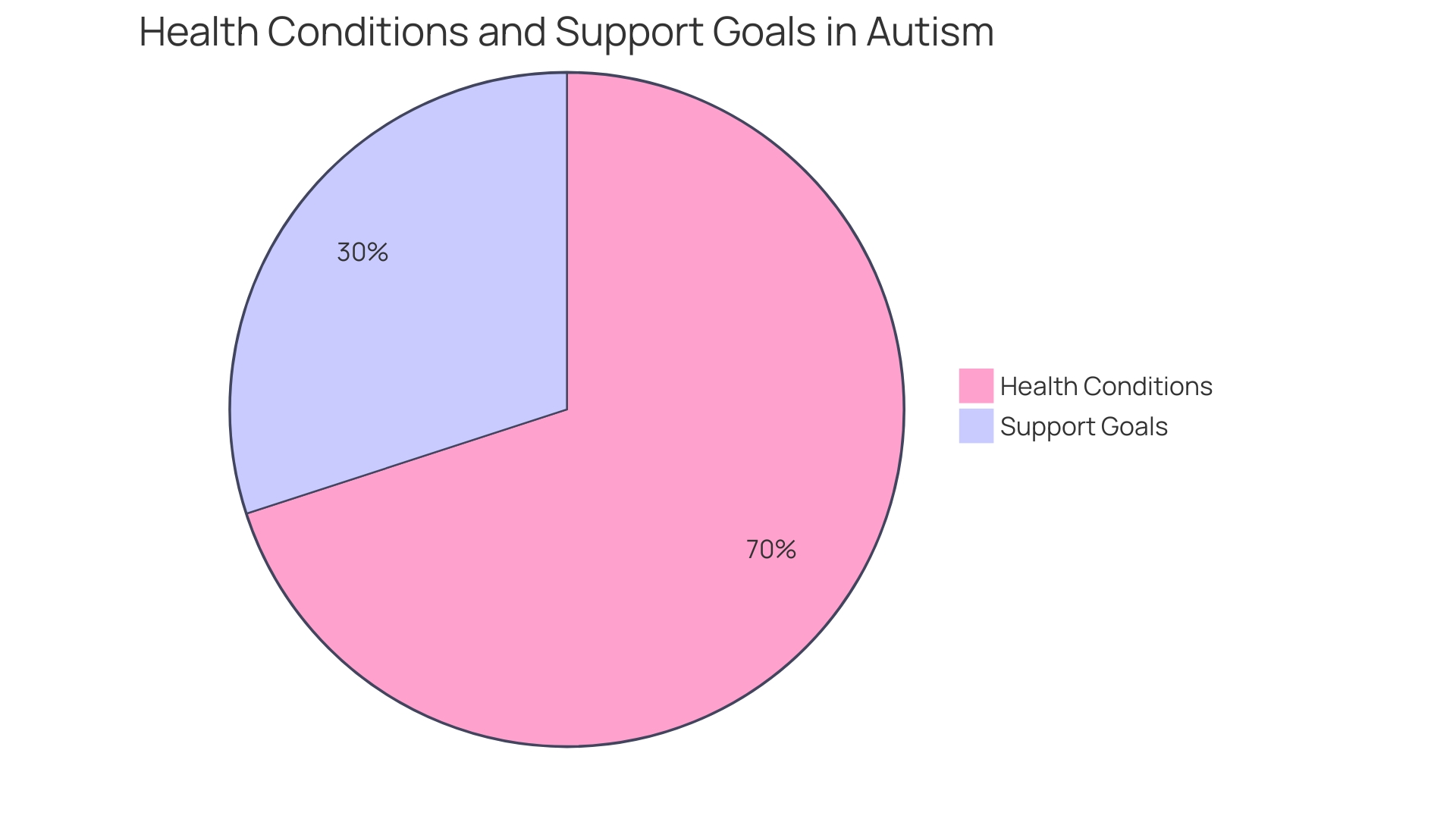
In ASD, self-harm can sometimes be a response to overwhelming sensory inputs or an effort to regulate intense emotions. Autistic individuals may not always communicate distress in conventional ways, and self-harm could be a non-verbal expression of their emotional turmoil. Recognizing this, the Department of Health and Social Care under the Autism Act statutory guidance suggests tailored support for autistic individuals facing mental health challenges. For example, Cognitive Behavioral Therapy (CBT) adaptations are recommended for autistic people with eating disorders, emphasizing the importance of personalized therapeutic approaches.
Conversely, individuals with BPD might use self-harm as a way to cope with acute emotional pain. The intense emotional experiences characteristic of BPD can make self-harm a method for managing or expressing distress. It's vital to understand these underlying differences to provide appropriate support and interventions.
Research, like that conducted at The Center for Discovery, leverages AI and machine learning on extensive data sets, including those of autistic individuals, to better predict and mitigate significant behaviors. This innovative approach aims to preempt the occurrences of self-harm by understanding the precursors to such actions.
The presence of self-harm behaviors in both ASD and BPD highlights the necessity of nuanced understanding and individualized care strategies. As self-harm can be a precursor to more severe mental health issues and even increase the risk of suicide attempts, it is imperative to address these behaviors with sensitivity and evidence-based interventions.
Emotional Dysregulation: Causes and Manifestations
Understanding and managing emotions can be particularly challenging for individuals with autism and those with Borderline Personality Disorder (BPD). Both groups often face difficulties with emotional regulation, which is the capacity to manage the intensity and duration of emotions. It is a skill that typically develops through childhood and adolescence, but can be disrupted by various biological and environmental factors, leading to emotional dysregulation.
For those with autism, emotional regulation is often hindered by their inherent difficulties in recognizing and communicating their emotions. This can lead to a mismatch between their internal emotional state and their external expression, sometimes resulting in unexpected emotional outbursts. In contrast, individuals with BPD may experience emotions with great intensity and rapid shifts, often in response to interpersonal interactions. Their emotional responses can be unpredictable and overwhelming, which is frequently associated with the disorder's hallmark instability in moods and self-image.
Emotional dysregulation can manifest in a variety of behaviors, from eating disorders to suicidality. Suicidal ideation, in particular, can be a coping strategy to escape extreme emotional turmoil. Further, emotional dysregulation may arise from external factors such as psychological trauma, including abuse or neglect during childhood, contributing to conditions like reactive attachment disorder.
Dr. Judy Ho, a neuropsychologist, highlights the role of the nervous system in regulating our responses to environmental and psychological stressors. The nervous system, which works closely with hormonal systems, triggers physical reactions to emotional stimuli, such as sweating or tensing muscles when we feel threatened. Understanding the nervous system's role can help us devise strategies to manage our emotions better.
Therapist Greg Bodin suggests in-the-moment techniques such as movement, breathwork, tuning into our senses, and emotional freedom technique (EFT) or 'tapping' to help regain emotional control during a crisis. These methods can serve as immediate tools to cope with intense emotions, but building long-term resilience is also crucial for those with emotional dysregulation.
It's important to acknowledge that emotional dysregulation does not define an individual. Many people with mental health concerns, including those with emotional regulation issues, lead productive and fulfilling lives. Recognizing the unique experiences of individuals and their support networks is essential in understanding and addressing the complexities of emotional dysregulation in autism and BPD.
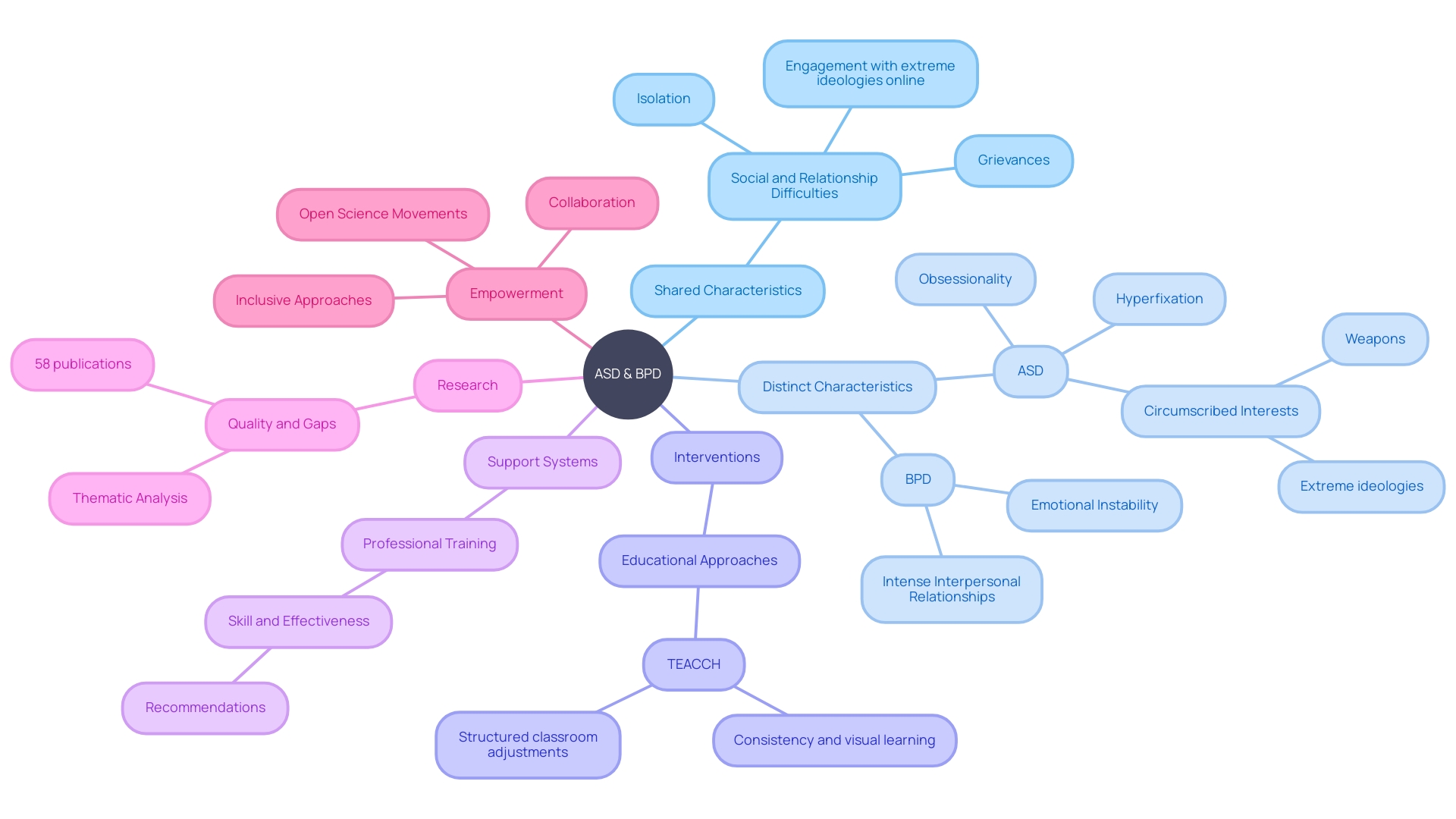
Areas of Difference Between ASD and BPD
Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) are distinct clinical entities that can sometimes be confused due to overlapping symptoms, such as difficulties in social interactions and emotional regulation. Distinguishing between them is crucial for effective treatment and support. A study in the Journal of Personalized Medicine highlighted the complexity of ASD by examining the case of 4-year-old dizygotic twins with 'level 3 severity' autism, requiring substantial support. These twins, conceived through in vitro fertilization, had diverse presentations despite their shared environment, underscoring the individualized nature of ASD.
Recent news stories, like that of Heather Florio who received an autism diagnosis at 41, further illustrate the diversity within the autism spectrum and the profound impact an accurate diagnosis can have on one's life. The evolving understanding of autism has led journals like Pediatric Research to avoid eponymous names that may not reflect the condition's spectrum, advocating for non-eponymous alternatives to foster clarity.
Beth Lambert from Epidemic Answers emphasizes the potential for improving the lives of children with ASD, highlighting resources and communities that empower parents to support their children’s journey. This reflects the growing recognition of the importance of personalized approaches in managing ASD symptoms and the need for ongoing research and education.
Understanding the nuances of ASD is vital, especially given its rising prevalence. The narrative that autism is a spectrum disorder is echoed by experts who stress that while high functioning autism might present with milder symptoms and higher intellectual abilities, it still poses substantial challenges. These include navigating social interactions, coping with sensory sensitivities, and managing repetitive behaviors.
The complexity of ASD, as illustrated by these case studies, news reports, expert insights, and academic discussions, reinforces the importance of recognizing the unique experiences of each individual. It's a call to action for a more personalized approach that honors the diversity within the autism community and the need for tailored interventions that address the distinct needs of each person on the spectrum.
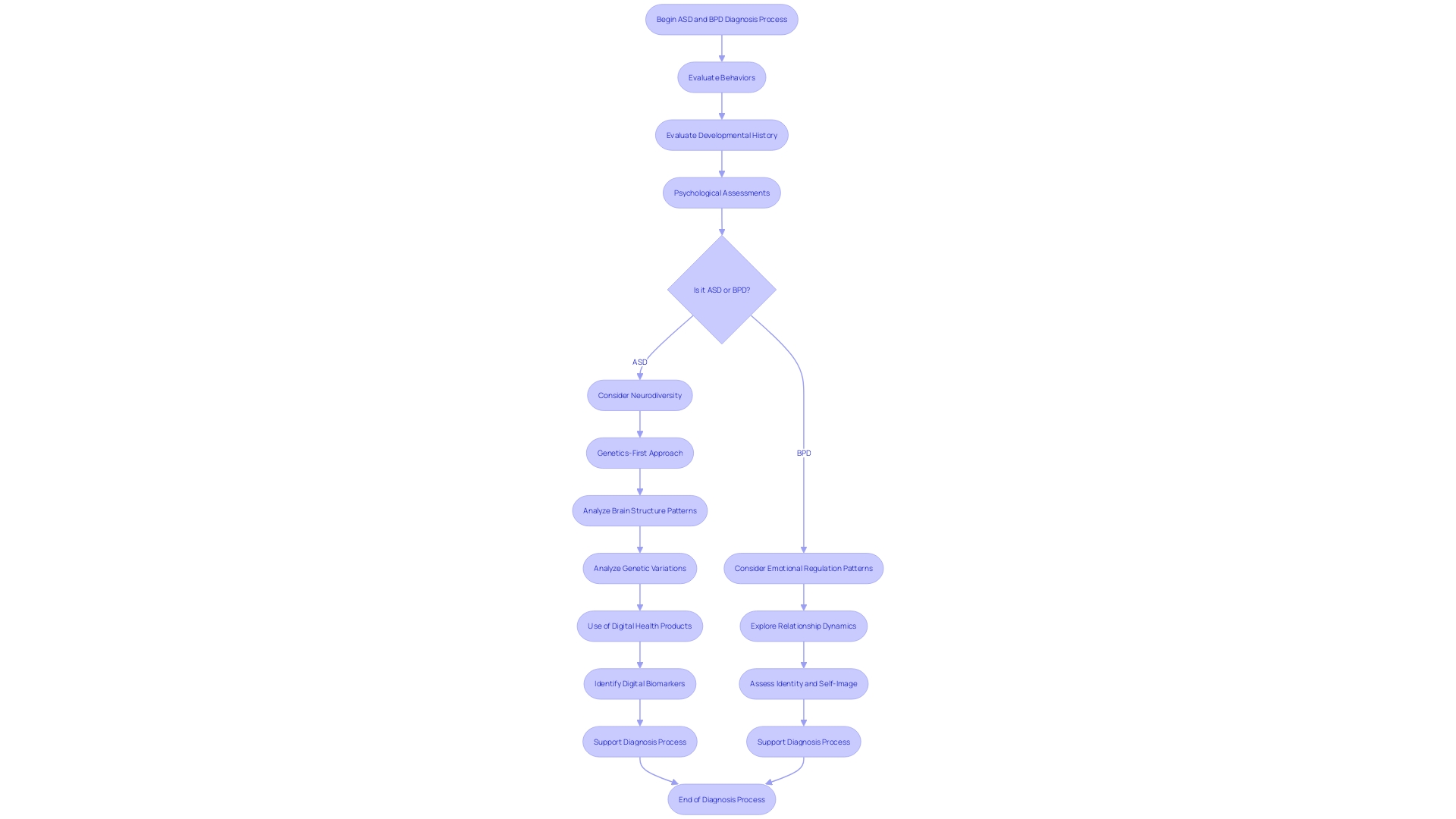
Diagnostic Considerations and Comprehensive Assessment
Determining whether an individual is on the autism spectrum or has Borderline Personality Disorder (BPD) necessitates a thorough evaluation that encompasses a spectrum of diagnostic tools. It's essential to observe behaviors, delve into the individual's developmental history, and conduct psychological assessments. Such a nuanced process is vital for accurately distinguishing between autism and BPD. Neurodiversity, a term that describes the wide range of brain development and information processing differences across the population, plays a significant role in understanding these conditions. Autism, a neurodevelopmental disorder characterized by distinct behaviors and considered a spectrum condition, affects individuals in various ways and degrees. According to the CDC, autism may occur in as many as 1 in 36 individuals. The diagnostic criteria outlined in the DSM-5 include persistent differences in communication and social interaction, as well as restricted and repetitive patterns of behavior. A genetics-first approach to autism, as suggested by recent research published in Science Advances, can revolutionize our understanding of the condition. This approach involves analyzing brain structure patterns and genetic variations known as "copy number variations," which are deletions or duplications in the genetic code linked to autism. With the prevalence of autism spectrum disorder (ASD) estimated at 1 in 45 adults in the U.S., it's critical to recognize that a formal diagnosis is not the sole pathway for self-identifying as autistic. Although no single tool should dictate the diagnosis of ASD, a combination of parent or caregiver descriptions and professional observations is typically used to assess the disorder. Digital health products, including mobile apps, show promise in supporting the diagnosis process by providing additional information from an individual's daily environment. This approach may help identify digital biomarkers, aiding in the early detection and understanding of autism and related conditions.
Case Study: Real-Life Examples of Coexistence
Delving into real-world experiences of those navigating both autism and Borderline Personality Disorder (BPD) illuminates the unique lived realities of these individuals. By understanding the distinct ways in which autism manifests—characterized by social challenges, repetitive behaviors, and intense interests, as noted by the National Autistic Society—we are better equipped to support those with concurrent BPD. Autism, a spectrum disorder influenced by numerous genetic factors, is often misunderstood. It does not imply intellectual disability, as only about half of autistic individuals face such challenges. Moreover, neurodiversity, a term embracing the range of differences in brain function, highlights that autism and other conditions like ADHD are not illnesses to be 'cured' but rather variations in human cognition.
Heather Florio's story, as reported in the news, serves as a powerful case study. Diagnosed at 41, her journey to self-acceptance after years of feeling 'different' underscores the importance of understanding and diagnosing autism. Similarly, individuals with AuDHD—a term merging autism and ADHD—demonstrate that co-occurring conditions can lead to complex but distinctive needs.
With this deeper comprehension, we can validate the coexistence of autism and BPD, tailoring interventions to each individual's needs. For instance, visual storytelling can demystify complex mental health concepts, offering clarity and empathy. As we share these narratives, we not only provide insights but also foster a more inclusive and supportive environment for those with autism and related conditions.
Implications for Treatment and Support
The intertwining of autism spectrum disorder (ASD) and borderline personality disorder (BPD) presents a complex challenge, yet understanding this connection opens doors to more nuanced care and support. Tailoring interventions to meet the unique combination of needs in individuals with both ASD and BPD is crucial for enhancing their quality of life. By distinguishing the shared and distinct characteristics of these conditions, we can customize support systems that not only address the challenges but also harness the strengths of those with dual diagnoses. Reflecting on Dr. David (Dan) R. Offord's vision of a fair race for all children, we recognize the importance of equipping individuals with disabilities with the tools they need for meaningful participation in society. This includes ensuring that caregivers have the necessary resources to foster their child's development and mental health. Open science movements, such as those seen during the pandemic, underscore the value of sharing knowledge and collaborating across borders to advance our understanding and interventions for complex conditions like ASD and BPD. At the UC Davis MIND Institute, such collaborative efforts are already shaping more personalized and equitable support systems for neurodevelopmental conditions. As we embrace this ethos of inclusivity and shared knowledge, we empower individuals with dual diagnoses to thrive in their communities.
Conclusion
In conclusion, understanding the complexities of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) is crucial for accurate diagnosis and effective support. These conditions share overlapping characteristics, such as challenges in social interaction and sensory sensitivities, but also have distinct differences.
Misdiagnosis is a concern due to the overlapping symptoms, emphasizing the need for reliable diagnostic tools and accurate information. Tailored interventions and early detection through innovative technologies can greatly improve outcomes.
Self-harm behaviors and emotional dysregulation are shared aspects, but the motivations and expressions differ. Recognizing these differences and providing individualized care strategies is essential for promoting mental health.
Comprehensive assessment and diagnostic considerations play a vital role in distinguishing between ASD and BPD. A thorough evaluation that incorporates various diagnostic tools is necessary.
Real-life examples highlight the unique challenges faced by individuals with dual diagnoses. Creating inclusive and supportive environments is crucial to their well-being.
Tailoring interventions to meet the specific needs of individuals with both ASD and BPD can greatly enhance their quality of life. Collaborative efforts and knowledge sharing contribute to empowering individuals with dual diagnoses.
In conclusion, a comprehensive understanding of ASD and BPD allows for accurate diagnosis, tailored support, and empowering interventions. Recognizing the unique needs and experiences of individuals with these conditions fosters an inclusive and supportive environment that promotes their well-being.




