Introduction
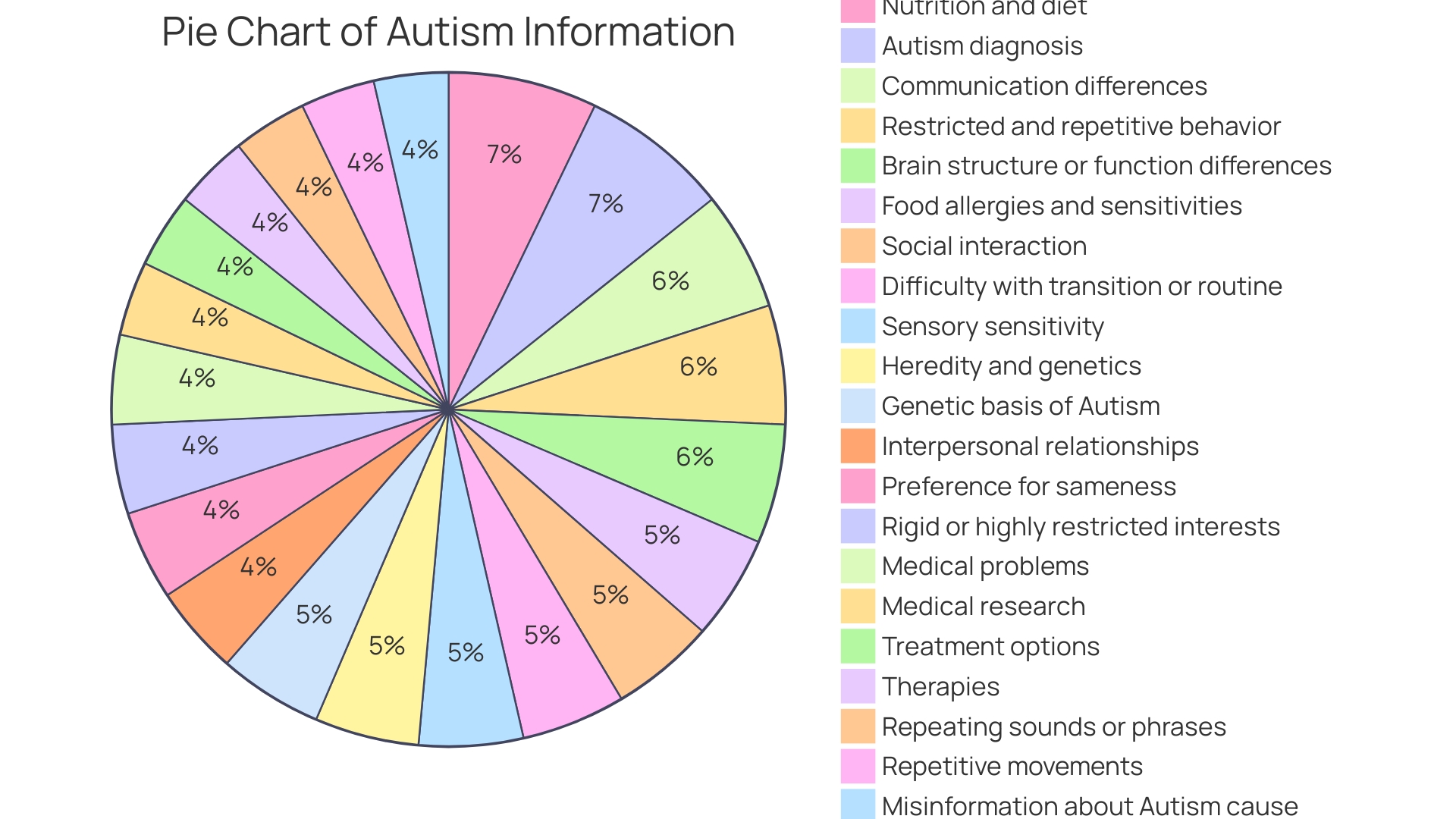
Autism presents unique challenges in dietary needs, with certain foods potentially exacerbating symptoms while others may offer relief. Understanding and addressing these dietary preferences is crucial for the well-being of children with autism. Sensory sensitivities and executive functioning can significantly influence food choices, leading to restricted diets and rigid thinking patterns.
Additionally, children with autism are more prone to gastrointestinal issues and may experience nutritional deficiencies. Managing food obsession and promoting healthy eating habits requires a holistic approach that considers medical factors, parent-child dynamics, and sensory sensitivities. Collaboration with healthcare professionals and support teams is essential in crafting individualized dietary approaches and tailored meal plans.
By embracing these strategies and understanding the interplay between autism and diet, we can foster a more supportive and equitable environment for children with autism to thrive.
Factors Influencing Food Preferences in Autism
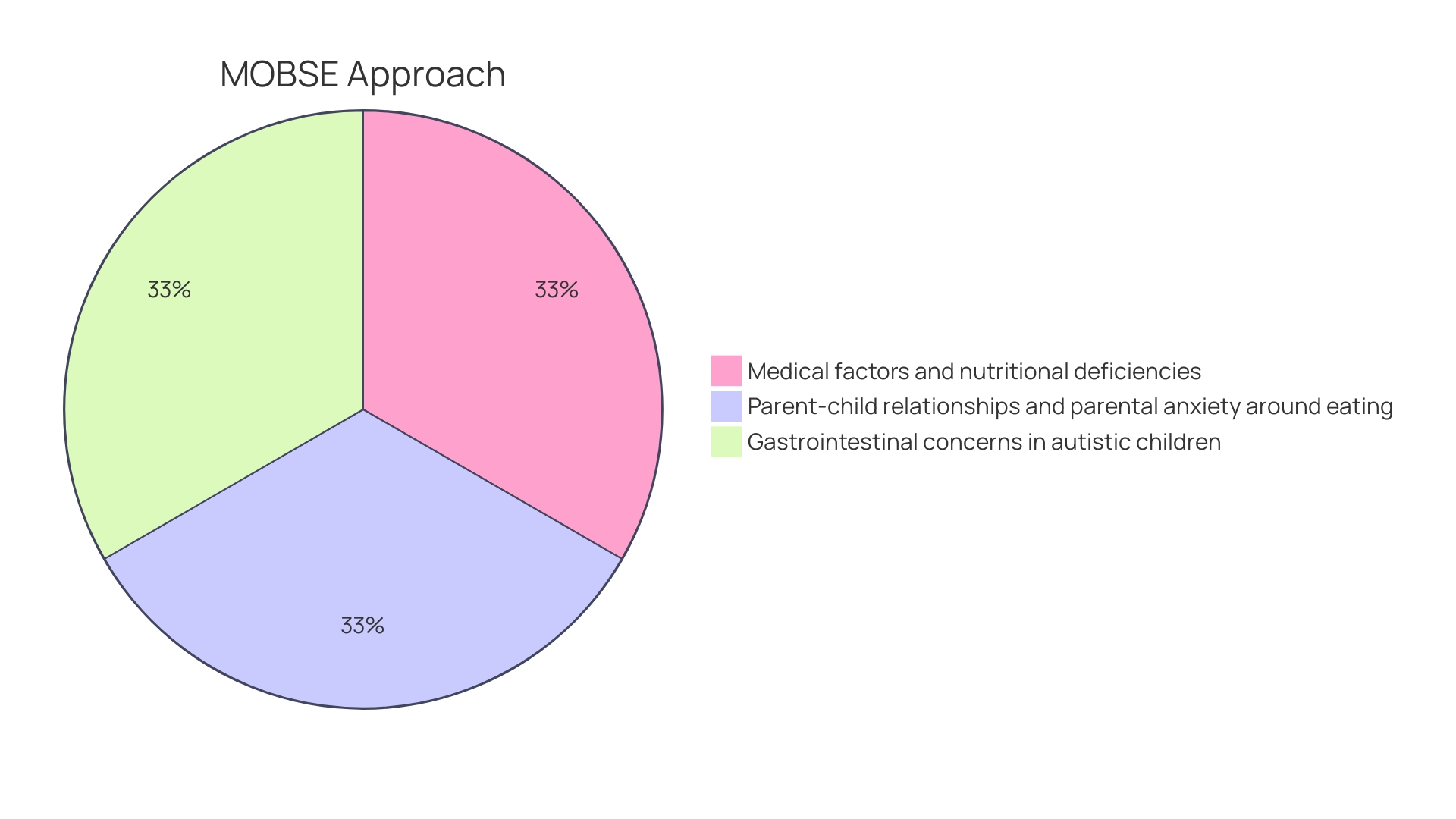
Autistic children often have unique dietary preferences, which can be shaped by a variety of influences. Sensory sensitivities may make certain textures or flavors overwhelming, resulting in a narrowed range of accepted foods. It's essential to acknowledge the complexity of these preferences to provide appropriate nutritional support. For example, the MOBSE approach, developed by Dr. Smile's research team at Holland Bloorview, underscores the importance of considering medical factors and nutritional deficiencies in autistic children, who are four times more likely to have gastrointestinal issues compared to their neurotypical peers. This framework emphasizes the role of the parent-child dynamic and parental concerns regarding eating, which can significantly impact feeding practices and the child's well-being. Furthermore, understanding that autistic children may experience various digestive problems, such as constipation, acid reflux, or food allergies, is vital for tailoring their diet to their specific needs. By addressing these factors with sensitivity and care, we can better support children with autism in achieving a balanced and enjoyable diet.
Sensory Sensitivities and Food Preferences
Understanding the dietary preferences and challenges faced by children with autism is a critical aspect of their care. Sensory sensitivities can significantly influence what foods these children find acceptable. For some, the texture, aroma, or flavor of certain foods may be too intense, leading to a narrow selection of preferred foods. By acknowledging these sensory preferences, caregivers can engage in strategies to diversify the child's diet effectively.
Holland Bloorview's MOBSE framework, developed by Dr. Smile's research team, emphasizes the intricate relationship between parent-child dynamics and eating behaviors. It underscores the importance of addressing medical and nutritional needs first, particularly since autistic children are more prone to gastrointestinal issues, such as constipation, acid reflux, and food allergies.
Recent research illuminates the connection between genetic mutations associated with Autism Spectrum Disorder (ASD) and sensory hypersensitivities. These findings highlight the need for tailored approaches to manage sensory challenges, which can include auditory hypersensitivity. Such sensory processing difficulties underscore the importance of considering individual sensory experiences when introducing new foods.
Studies also reveal that responsive food parenting can play a pivotal role in developing healthy eating habits. Parents who encourage curiosity about food and respect their child's preferences can foster a more positive mealtime atmosphere. This approach is especially beneficial for children facing the dual challenges of sensory sensitivities and restricted diets.
Innovative programs, like The Arc's culinary arts initiative, demonstrate how hands-on experiences with food can be empowering. By involving children in food preparation and catering, such initiatives offer valuable life skills and normalize the food experience, aligning with the understanding that food is far more than mere sustenance; it is a source of nourishment, cultural identity, and a means to feel valued.
Executive Functioning and Rigid Thinking in Food Choices
For individuals with autism, the process of managing diet and food choices can be particularly challenging due to the nature of their neurodiversity. Autism Spectrum Disorder (ASD) affects communication, social interactions, and can result in unique sensory sensitivities and preferences. These characteristics may lead to rigid thinking patterns and a resistance to trying new foods or changing eating habits. Recognizing these difficulties is crucial for parents and professionals to tailor their approach to support healthy eating habits effectively.
One important framework to consider is the MOBSE approach, developed by Dr. Smile's research team, which emphasizes the significance of parent-child dynamics and parental concerns in relation to feeding. This approach involves assessing medical and nutritional factors to ensure children with autism are medically stable, given that they are four times more likely to experience gastrointestinal issues than their neurotypical peers.
Moreover, understanding the impact of executive functions, which include planning, organization, and decision-making skills, is vital. These mental processes are essential for managing one's diet and can be particularly challenging for individuals with neurodiverse conditions. For example, children with ADHD, which can co-occur with autism, often struggle with impulse control and setting goals around food, impacting their ability to maintain a balanced diet.
Recent research has also shed light on eating behavior patterns in children, with findings suggesting that about one in five young children exhibit 'avid eating,' characterized by a heightened enjoyment of food and reduced sensitivity to fullness. Knowing these patterns can help predict which children may be more at risk of weight issues, thus allowing for more personalized and effective dietary strategies.
Incorporating these insights, parents and professionals can work together to create a supportive environment that accommodates the unique needs of children with autism. This can lead to a more varied and nutritious diet, ultimately contributing to better overall health and well-being for these individuals.
Nutritional Concerns and Deficiencies
For children with autism, maintaining a balanced diet is crucial, yet it can be challenging due to common food sensitivities and restricted eating patterns. These dietary limitations can lead to nutritional deficiencies, impacting their growth and overall health. It's essential to collaborate with healthcare professionals to ensure these children receive the necessary nutrients. Recent studies have raised concerns about the nutritional quality of plant-based diets, especially for children, as they may lack certain nutrients found in animal products. Moreover, the trend towards ultra-processed plant-based alternatives, while often perceived as equivalent to their animal-based counterparts, may not provide the same nutritional benefits and could contain additives that affect the gut microbiome. Ensuring a child's diet supports their neurological development is imperative, as autism and ADHD have been linked to increased sensitivity to certain food additives and contaminants like heavy metals and pesticides. Knowledgeable parents who are aware of these potential dietary pitfalls can make informed choices to minimize exposure to these substances, thereby supporting their child's well-being. With the rise of mental and physical health issues among children and the prevalence of fast food in their diets, it's clear that food quality is a critical factor. As advocates for children's health, it's our responsibility to address these nutritional gaps and support parents in fostering healthier eating habits for their children with autism.
Impact of Food Obsession on Daily Life and Well-being
Children on the autism spectrum can sometimes develop a very narrow focus on certain foods or rigid mealtime routines, which presents a challenge not only to their nutrition but also to family dynamics. This phenomenon can be understood through Dr. Smile's MOBSE approach, which considers parental relationships and anxiety around feeding, alongside medical factors like gastrointestinal issues, which are reported to be four times more prevalent in autistic children than in their neurotypical peers.
Nutritional stability takes precedence in the MOBSE framework, with considerations for conditions such as constipation, acid reflux, and food allergies. It's crucial that these children are not simplistically labeled as 'fussy eaters,' as this can exacerbate the issue and overlook underlying medical concerns. Instead, it's important to recognize that the food preferences may be deeply ingrained in how the brain processes sensory information, as part of their neurodiverse condition. This understanding paves the way for tailored strategies that can help them expand their dietary variety while respecting their individual needs.
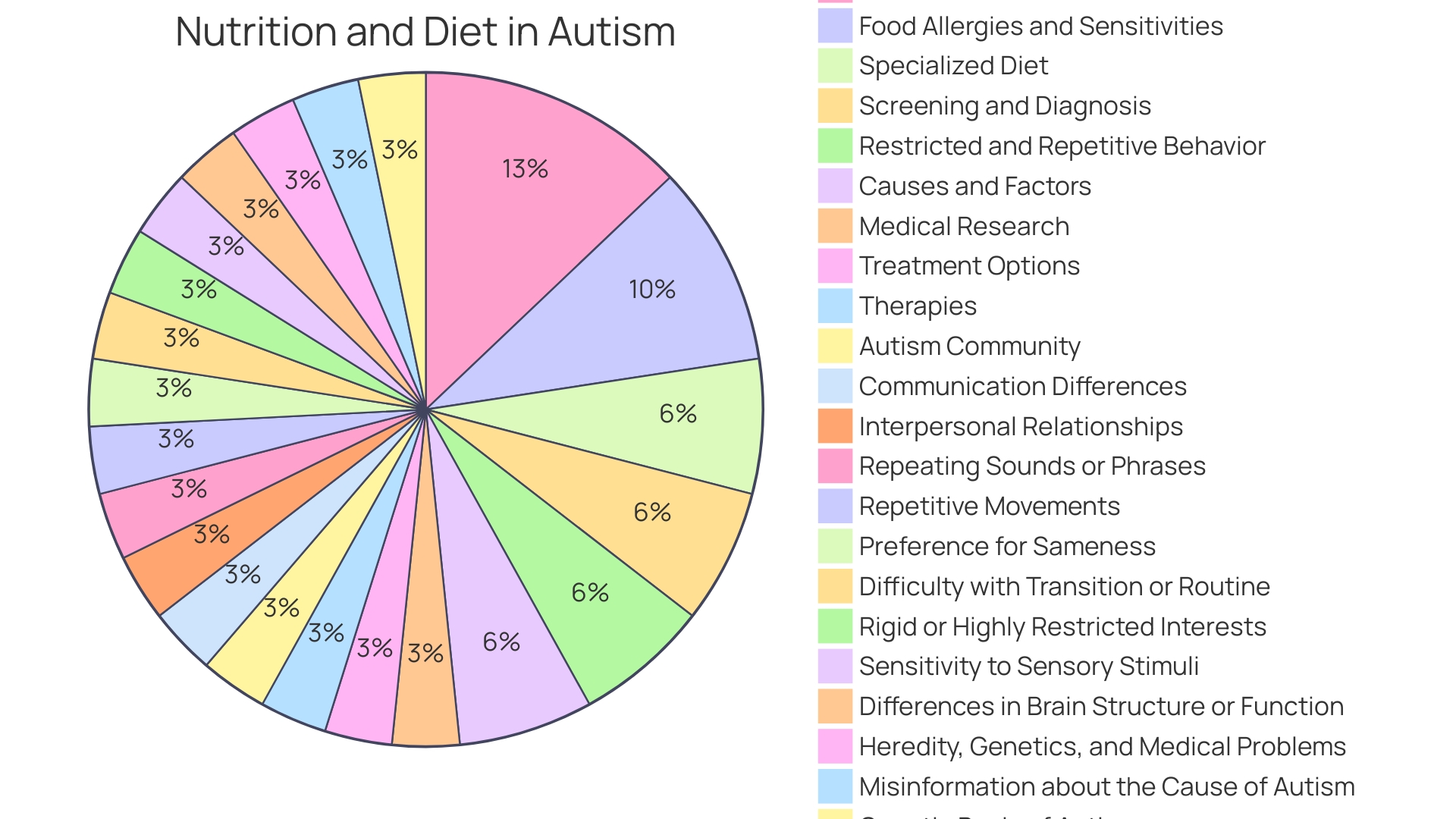
The Autism Community in Action (TACA) emphasizes the significant role of nutrition and diet in health and particularly notes the commonality of food allergies and sensitivities in autism. By exploring specialized diets and improved eating habits, parents and professionals can foster a more positive approach to food. In the spirit of neurodiversity, it's also beneficial to accommodate these children in school environments by permitting 'safe' foods that align with their comfort and needs, thus supporting their educational and social experiences.
Moreover, the Department of Health and Social Care's Autism Act statutory guidance, along with NICE recommendations, advocate for adapted therapeutic interventions, like Cognitive Behavioral Therapy (CBT), tailored to the needs of autistic individuals with eating disorders. These adaptations, along with the option for reasonable adjustments, exemplify the proactive measures that can be taken to support autistic children on their journey towards a healthier relationship with food.
Role of Nutrition and Lifestyle Interventions
Tailoring a child’s diet to address individual needs can be a powerful tool in supporting their development, especially in children with autism. By identifying and managing gastrointestinal issues, which are reported up to four times more in autistic children compared to their neurotypical peers, a significant improvement in quality of life can be achieved. The MOBSE framework, developed by Dr. Smile’s research team at Holland Bloorview, emphasizes the importance of understanding the interplay between medical factors, nutritional deficiencies, and parent-child dynamics in feeding.
Adequate nutrition is not only about meeting dietary requirements; it's about fostering a nurturing environment that acknowledges the cultural significance of food and its role in making children feel valued and at home. Studies have shown that a healthy diet during pregnancy may reduce the risk of childhood autism, highlighting the necessity of nutritional vigilance from the earliest stages of development.
The commitment to a fair and supportive race for children with disabilities, as championed by Dr. David (Dan) R. Offord, extends to ensuring that children with autism receive appropriate support in all domains of their lives - at school, at home, and during leisure activities. This holistic approach can reduce stress for both the child and their caregivers, facilitating better mental health and overall well-being. Engaging with medical interventions and behavioral communication, as advised by experts, can also significantly enhance outcomes for autistic children.
Importance of Balancing Blood Sugar and Identifying Food Allergies
Stabilizing blood sugar levels and identifying potential food allergies are key steps in managing the health of children with autism. Studies show that children on the autism spectrum are four times as likely to experience gastrointestinal problems, such as constipation, acid reflux, and irritable bowel syndrome, compared to their neurotypical peers. These digestive issues can significantly affect a child's behavior, mood, and overall quality of life.
The groundbreaking MOBSE approach, developed by Dr. Smile's research team at Holland Bloorview, emphasizes the importance of medical stability and nutritional adequacy in these children. It highlights how intricately linked a child's eating experience is with parent-child dynamics and the anxiety that can surround mealtimes.
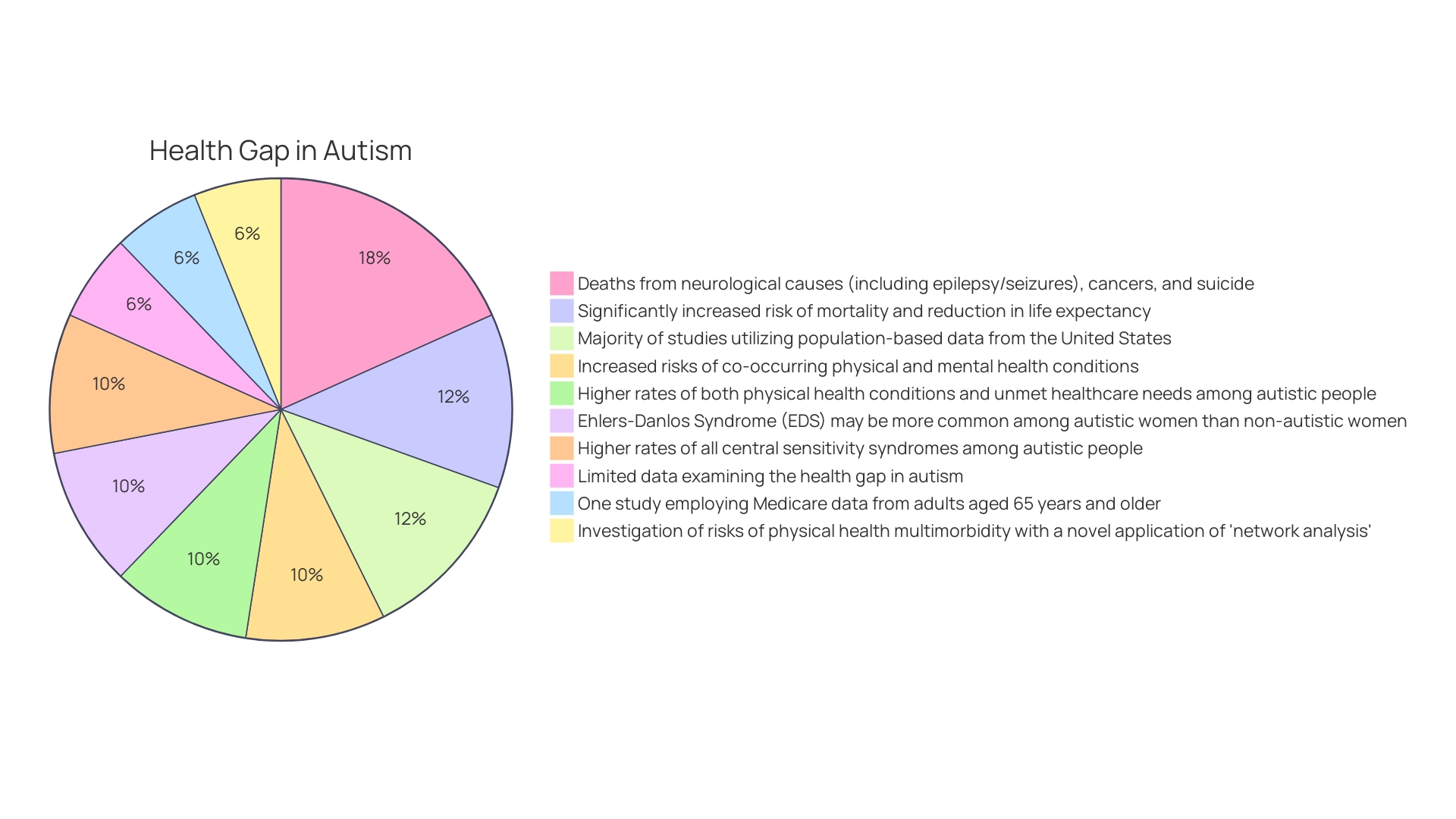
Moreover, recent statistics indicate that autistic individuals face a higher risk of co-occurring physical health conditions, which may contribute to a reduction in life expectancy. Autistic adolescents and young adults, in particular, show higher rates of unmet healthcare needs and physical health conditions.
Addressing both blood sugar balance and potential food allergies is not just about symptom management; it's about enhancing the overall well-being of the child and reducing the risk of additional health complications. As we continue to understand the complex interplay between diet and autism, it becomes increasingly clear that a comprehensive approach to medical and nutritional care is vital for these children's health and development.
Addressing Gastrointestinal Issues and Restoring Gut Balance
The intricate ecosystem within our intestines, known as the gut microbiota, encompasses trillions of microorganisms, including bacteria, viruses, and fungi. This ecosystem is not static; it begins to flourish from birth and undergoes significant development during the early years, playing a vital role in digestion, metabolism, immune system maturation, and even brain development. In children with autism, this gut microbiota may diverge from typical patterns, manifesting in gastrointestinal challenges that are all too common in these young individuals.
For children on the autism spectrum, gastrointestinal discomfort can range from mild stomach cramps to more severe forms of diarrhea, often linked to an imbalance in gut microbes. This imbalance may present a skewed ratio of harmful-to-beneficial bacteria and reduced microbial diversity. Addressing these gastrointestinal issues is not just about alleviating physical symptoms; it also has the potential to enhance the overall quality of life for these children. The GEMMA project, which tracks the microbial content in the stools of infants who have older siblings with autism, underscores the importance of a balanced bacterial composition in maintaining intestinal integrity. This research hints at the profound connection between gut health and the development of autism.
Probiotics have been recognized for their ability to improve a broad spectrum of health conditions by interacting with and balancing our microbial communities. By competing with pathogenic microbes for binding sites and stimulating immune response, probiotics may offer a beacon of hope for managing not only common gastrointestinal ailments but also more complex conditions indirectly related to gut health. Such interventions, tailored to the needs of children with autism, could be pivotal in not just managing symptoms but in supporting their overall well-being and development.
The importance of a balanced diet and adequate nutrition cannot be overstated, especially when considering the frequent occurrence of food allergies and sensitivities in children with autism. Organizations like The Autism Community in Action (TACA) emphasize the impact of nutrition on both physical health and cognitive function. By exploring and navigating specialized diets, parents and caregivers can make informed decisions that may significantly improve eating habits and, subsequently, the health of their children with autism.
As we continue to unravel the complexities of autism and its association with gut health, it's evident that the intertwining of these biological systems holds keys to unlocking better health outcomes. With the prevalence of autism now estimated at 1 in 44 children, the imperative to understand and address the full spectrum of health challenges becomes even more pressing. By focusing on gut balance and nutrition, we not only address the gastrointestinal concerns but potentially pave the way for more resilient and thriving children.
Strategies for Managing Food Obsession and Promoting Healthy Eating
Establishing a balanced diet and addressing food-related challenges in children with autism is critical, given the higher likelihood of gastrointestinal issues in these children compared to their neurotypical peers. A holistic strategy is essential, which includes structured mealtime routines to provide predictability and security, gradual introduction of new foods to accommodate sensory sensitivities, and active involvement of children in meal planning and preparation to foster autonomy and interest in food. Such approaches can mitigate parental anxiety surrounding mealtimes and support children in forming a positive and healthy relationship with eating, as emphasized by the MOBSE approach from Holland Bloorview's research team. This framework underscores the importance of medical stability and nutritional adequacy in autistic children, who are four times more prone to report gastrointestinal concerns, highlighting the need for careful monitoring of potential medical issues such as constipation, acid reflux, and food allergies. By embracing these strategies, parents and professionals can promote the mental health and equitable social participation of children with autism, ensuring that they are not unfairly disadvantaged in the 'race' of growing up.
Collaboration with Healthcare Professionals and Support Teams
Forging a path to wellness for children with autism involves a holistic approach, and dietary considerations play a crucial role. Recognizing that each child's needs are unique, a collaborative effort between parents and healthcare professionals is pivotal. Together, they can craft individualized nutritional strategies that not only cater to specific health requirements but also accommodate the child's sensory preferences and any food sensitivities or allergies. This partnership allows for ongoing evaluation and fine-tuning of dietary plans, thus fostering an environment where children can thrive both physically and emotionally.
The Autism Accreditation program underscores the importance of such collaborative efforts, setting a high standard for support systems that cater to the autistic community. It is a testament to the necessity of continuous improvement and tailored care in these settings. According to The Autism Community in Action (TACA), nutrition can significantly impact not just physical health but also cognitive function, highlighting the need for well-considered dietary approaches.
In the words of Dr. Smile, whose research birthed the MOBSE framework, it's imperative to ensure that children are 'nutritionally and medically stable,' acknowledging that autistic children are more likely to experience gastrointestinal issues. Furthermore, as Dr. David (Dan) R. Offord pointed out, the goal is to ensure that all children, including those with disabilities, have equitable opportunities for growth and development. This includes not just addressing their needs but also leveraging their strengths, in an environment free from undue stress, where caregivers are empowered with the necessary resources.
Ultimately, the journey towards optimal health for autistic children involves a community of support, where food is more than sustenance—it's a foundation for growth, a source of comfort, and a right every child deserves.
Individualized Dietary Approaches and Tailored Meal Plans
Autism presents unique challenges in dietary needs, with certain foods potentially exacerbating symptoms while others may offer relief. It's essential to recognize that each autistic child is distinct, with their own preferences, intolerances, and nutritional requirements. For instance, gastrointestinal issues are notably more prevalent in autistic children, affecting their comfort and behavior. A tailored diet, therefore, becomes not just beneficial but necessary for their health and well-being.
By adopting a personalized approach, like the MOBSE framework developed by Dr. Smile's team, which takes into account medical factors and nutritional deficiencies, caregivers can better manage these dietary intricacies. This method aligns with recent findings from The Center for Discovery, which emphasize the importance of individualized strategies to predict and mitigate behaviors.
Moreover, general public health guidance often overlooks the variability in children's eating behaviors, leaving parents to deal with a one-size-fits-all approach that rarely fits their child. Recognizing this, research funded by the Economic and Social Research Council seeks to define eating behavior profiles, allowing for more customized feeding strategies. This research is crucial for parents striving to support their child's unique dietary needs.
As we understand more about the interplay between autism and diet, the emphasis on individualized nutrition plans grows. It's a way not only to manage the medical and behavioral aspects of autism but also to ensure that the child's developmental race is as fair and supported as possible, echoing the sentiments of Dr. David (Dan) R. Offord on the importance of equity in children's health and participation.
Conclusion
In conclusion, addressing the unique dietary needs of children with autism is crucial for their well-being. Sensory sensitivities significantly influence their food preferences, and strategies to diversify their diet effectively must be implemented. Collaboration with healthcare professionals and tailoring individualized dietary approaches are key in promoting healthy eating habits.
Children with autism often face executive functioning challenges, making it difficult to manage their diet and food choices. Recognizing these challenges is important for parents and professionals to provide appropriate support. Considering the interplay between parent-child dynamics and medical factors, such as gastrointestinal issues, is essential in maintaining a balanced diet for children with autism.
Nutritional deficiencies are common among children with autism due to their restricted eating patterns. Collaborating with healthcare professionals and being aware of potential dietary pitfalls, such as plant-based diets lacking certain nutrients, can help address these deficiencies. Making informed choices and addressing nutritional gaps are crucial for fostering healthier eating habits in children with autism.
Food obsession can present challenges to nutrition and family dynamics. Understanding that food preferences may be deeply ingrained in sensory processing is important. By addressing these preferences with sensitivity, children can expand their dietary variety while respecting their individual needs.
Accommodating children in school environments and providing adapted therapeutic interventions are crucial in developing a healthier relationship with food.
Stabilizing blood sugar levels and identifying food allergies are key steps in managing the health of children with autism. A comprehensive approach to medical and nutritional care is essential in enhancing overall well-being and reducing the risk of additional health complications.
In conclusion, by understanding and addressing the unique challenges in dietary needs faced by children with autism, we can create a more supportive environment for them to thrive. Collaboration with healthcare professionals, consideration of sensory sensitivities and executive functioning challenges, and tailoring individualized dietary approaches are vital in promoting healthy eating habits and ensuring the well-being of children with autism.




