Introduction
Pervasive Developmental Disorders (PDD), such as Autism Spectrum Disorder (ASD), have a profound impact on social interaction, communication, and behavior. With a prevalence of 1 in 54 children diagnosed with ASD in the U.S., accurate diagnosis and comprehensive assessments are crucial.
This article explores the definition, historical trends, early detection and intervention, comprehensive management approaches, and the vital role of parent advocates in enhancing outcomes for children with PDD. Discover valuable guidance and resources to navigate these challenges and ensure the well-being of your child.
Definition and Prevalence of PDD Disorder
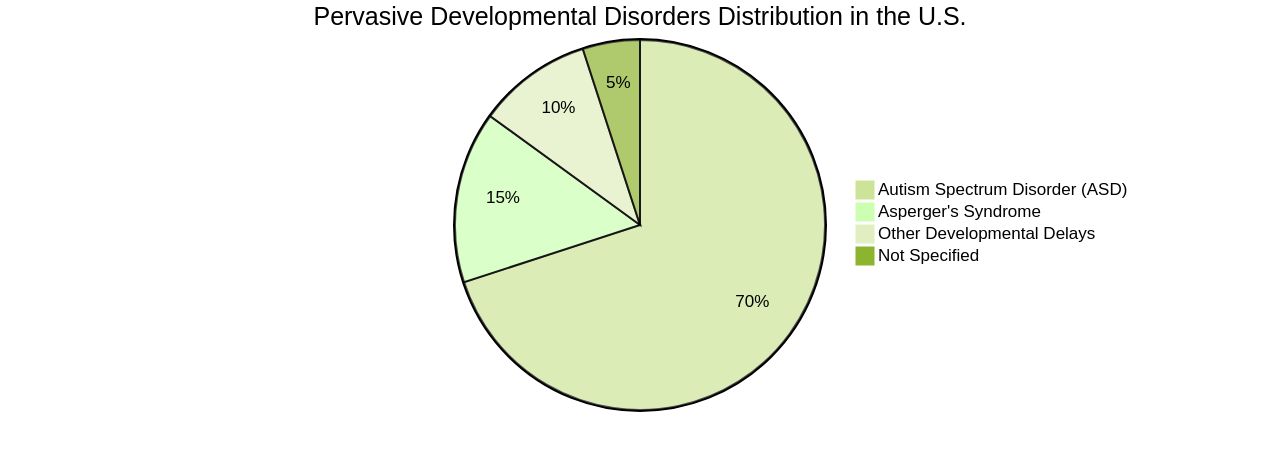
Pervasive Developmental Disorders (PDD), including Asperger's syndrome, affect social interaction, communication, and behavior through restricted interests and repetitive activities. These disorders present challenges from early childhood, persisting into adulthood.
Notably, around 1 in 54 children is diagnosed with autism spectrum disorder (ASD) in the U.S., highlighting the widespread impact of these conditions. Accurate diagnosis is crucial for managing PDD, and it relies on comprehensive assessments that combine parent or caregiver reports with professional observations.
The Diagnostic and Statistical Manual, Fifth Edition (DSM-5), outlines standardized criteria for diagnosing ASD, while tools like the Autism Diagnostic Interview-Revised (ADI-R) assess behaviors in social interaction, communication, and repetitive behaviors. However, it's important to remember that no single tool is definitive for diagnosis. Specialists such as neurodevelopmental pediatricians and child neurologists play a vital role in the assessment process, often in conjunction with early intervention programs. Despite the complexities involved in diagnosing PDD, it is essential for tailoring appropriate interventions and support, underscoring the need for continued research and improved diagnostic methods.
Historical and Current Trends in PDD Disorder
As we delve into the intricacies of Pervasive Developmental Disorders (PDD), it's imperative to recognize the evolution of our understanding and the diagnostic landscape. With the advent of the DSM-5, a significant consolidation occurred, replacing various PDD subtypes with the broader classification of Autism Spectrum Disorder (ASD).
This pivotal move has not only streamlined the diagnostic process but has also fostered a more inclusive perspective on the spectrum of neurodevelopmental disorders. Recent studies, like those conducted by Dr. Thomas Reilly of Oxford University, underscore the prevalence of conditions such as Premenstrual Dysphoric Disorder (PMDD), highlighting the potential under-diagnosis of these conditions.
With approximately 1.6% of women and girls globally meeting the stringent criteria for PMDD, the actual figures could be higher, suggesting a need for greater awareness and refined diagnostic approaches. In parallel, groundbreaking research into the human microbiome offers promising insights into autism.
For instance, a study from the Simons Foundation's Autism Research Initiative (SFARI) has illuminated the complex interrelations between gut microbes and ASD. This aligns with TACA's efforts, which emphasize the importance of early intervention in ASD, and the innovative work by researchers at Indiana University and Purdue University, who are pioneering diagnostic techniques to expedite ASD identification. The global clinical practice network's latest advancements in revising the criteria for mental, behavioral, or neurodevelopmental disorders aim to reflect real-world clinical practice more accurately. By avoiding arbitrary symptom thresholds and offering a nuanced symptom description, the revisions in the ICD-11 aim to enhance diagnostic precision and cultural relevance across diverse populations. This ongoing research and the evolution of diagnostic criteria are critical in shaping the future of care and support for individuals with neurodevelopmental and psychiatric conditions, providing a clearer path for parent advocates in their journey to assist families navigating these challenges.
Early Detection and Intervention for PDD Disorder
Understanding the early indicators of Pervasive Developmental Disorders (PDD), including Parkinson's Disease (PD), is pivotal for parents and caregivers. The subtleties of these early signs, such as diminished olfactory senses and constipation, could be the first whisperings of PD and are often overlooked. However, research has shown a correlation between diabetes mellitus and the incidence of PD, with a significant likelihood ratio.
This underpins the importance of maintaining good glycemic control, not only for its general health benefits but also as a potential factor in influencing PD progression. Furthermore, innovative treatments like exenatide have shown neuroprotective promises, enhancing cognitive functions and life quality for PD patients. The World Health Organization emphasizes the urgency in creating harmonized strategies for PD risk reduction, advocating for individual and community-level interventions.
The advent of AI and large datasets, such as the AlzEye, has revolutionized our ability to detect PD markers years before traditional symptoms manifest, offering a window for earlier intervention. As parent advocates, recognizing these early signs and advocating for timely evaluations and therapies, including speech and occupational therapy, can drastically alter the trajectory of PDD outcomes. Informed, proactive engagement with healthcare providers ensures that interventions are tailored to the unique challenges faced by individuals with PDD, ultimately supporting their long-term well-being.
Comprehensive Approach to Managing PDD Disorder
To effectively manage Pervasive Developmental Disorders (PDD), a tailored strategy that encompasses behavioral, social, and therapeutic interventions is crucial. This integrative approach includes behavioral therapies, social skills development, and speech and language therapy, all of which are essential for the individual's progress.
Occupational therapy and adjustments within the educational system are also integral to this comprehensive plan. The collaborative effort between healthcare providers, educators, and therapists, along with the involvement of community resources, forms the cornerstone of an individualized treatment plan.
This holistic method can significantly enhance the quality of life for those with PDD, as evidenced by the case of improved finger movement and swelling in a pediatric patient. Despite the absence of standardized treatment protocols, significant advancements have been made in understanding the biological underpinnings of neurodevelopmental disorders like PDD.
For example, the complex interplay of factors such as protein build-up in the brain has been identified, leading to innovative testing methods. These developments underscore the necessity for personalized care that not only addresses the immediate symptoms but also aligns with the biological complexity of the condition. Incorporating evidence-based pharmacological treatments, such as SSRIs or SNRIs, when non-pharmacological methods fall short, is another critical aspect of managing associated mood and anxiety disorders. This approach should always be personalized and enacted in partnership with mental health professionals, considering the individual's unique needs influenced by various factors, including co-occurring conditions, age, developmental level, and personal circumstances. The aim is not only to support the individual but also to empower caregivers with a comprehensive understanding of the behaviors and needs of those with PDD, guiding them towards effective interventions.
The Role of Parent Advocates in Enhancing Outcomes
Parent advocates play a pivotal role in the lives of children with developmental disorders, acting as a bridge between their children and the world around them. With a keen awareness of their child's unique needs, these dedicated individuals attend educational planning sessions and therapy appointments, contributing valuable input that shapes their child's development. Statistics reveal that such involvement has tangible benefits: 18.8% of children have a parent with an internalizing disorder diagnosis, which impacts their educational journey.
Parent advocates often draw strength and knowledge from connecting with peers, which has been shown to increase parental engagement and reduce out-of-home care placements. Studies suggest that when parents are engaged, children are more likely to stay with their families, benefit from family-centered placements, and experience successful reunifications, all while reducing the chance of re-entering the welfare system. These outcomes are not only supported by qualitative research methods, including interviews and focus groups, but also by quantitative data like the 4.4 million parents with disabilities who demonstrate daily that disability does not preclude effective parenting.
The Inklings initiative exemplifies this, highlighting the importance of early intervention and parental involvement in shaping positive outcomes for children with disorders like autism. This partnership aligns with the NDIS Review's recommendations for early supports and has already shown promising results for participating families. Through advocacy and support, parent advocates are essential agents of change, ensuring their children receive the best possible care and opportunities for success.
Conclusion
In conclusion, accurate diagnosis and comprehensive assessments are crucial for managing Pervasive Developmental Disorders (PDD) like Autism Spectrum Disorder (ASD). Ongoing research and improved diagnostic methods are needed to better understand and support individuals with PDD.
Early detection plays a vital role in timely evaluations and therapies that can significantly impact outcomes. A comprehensive approach to managing PDD includes behavioral therapies, social skills development, speech and language therapy, occupational therapy, and adjustments in the educational system.
Collaborative efforts between healthcare providers, educators, therapists, and community resources are crucial for individualized treatment plans. Parent advocates have a pivotal role in enhancing outcomes for children with PDD.
Their involvement in educational planning sessions and therapy appointments shapes their child's development. Parent engagement leads to increased parental involvement, reduced out-of-home care placements, successful reunifications, and decreased re-entry into the welfare system.
By staying informed about accurate diagnosis methods, early detection strategies, comprehensive management approaches, and leveraging your advocacy skills as a parent advocate, you can make a positive impact on your child's journey. Remember that you are not alone—valuable guidance resources are available to support you every step of the way. Empower yourself through knowledge and support networks to ensure the well-being of your child with PDD. Together with healthcare providers and educators, create an individualized plan that addresses your child's unique needs and provides them with the best possible care and opportunities for success. Your role as a parent advocate is essential in navigating the challenges of PDD and ensuring a brighter future for your child.




