Introduction
Neurodevelopmental Disorders, such as Autism Spectrum Disorder (ASD) and Pervasive Developmental Disorder (PDD), pose unique challenges for parents and caregivers. Navigating the diagnostic process, understanding treatment options, and advocating for their children's well-being can be overwhelming. However, in the face of these complexities, there is a growing community of Parent Advocates who are empowered to support their children with confidence and resilience.
In this article, we will explore the importance of early detection and intervention, the multidisciplinary approach to treatment, the role of Parent Advocacy in the diagnostic process, and the significance of a robust support system for parents and caregivers. Through guidance and resources, we aim to equip Parent Advocates with the tools they need to navigate the journey of PDD diagnosis and treatment, ensuring the best possible outcomes for their children.
Definition and Diagnostic Criteria of PDD
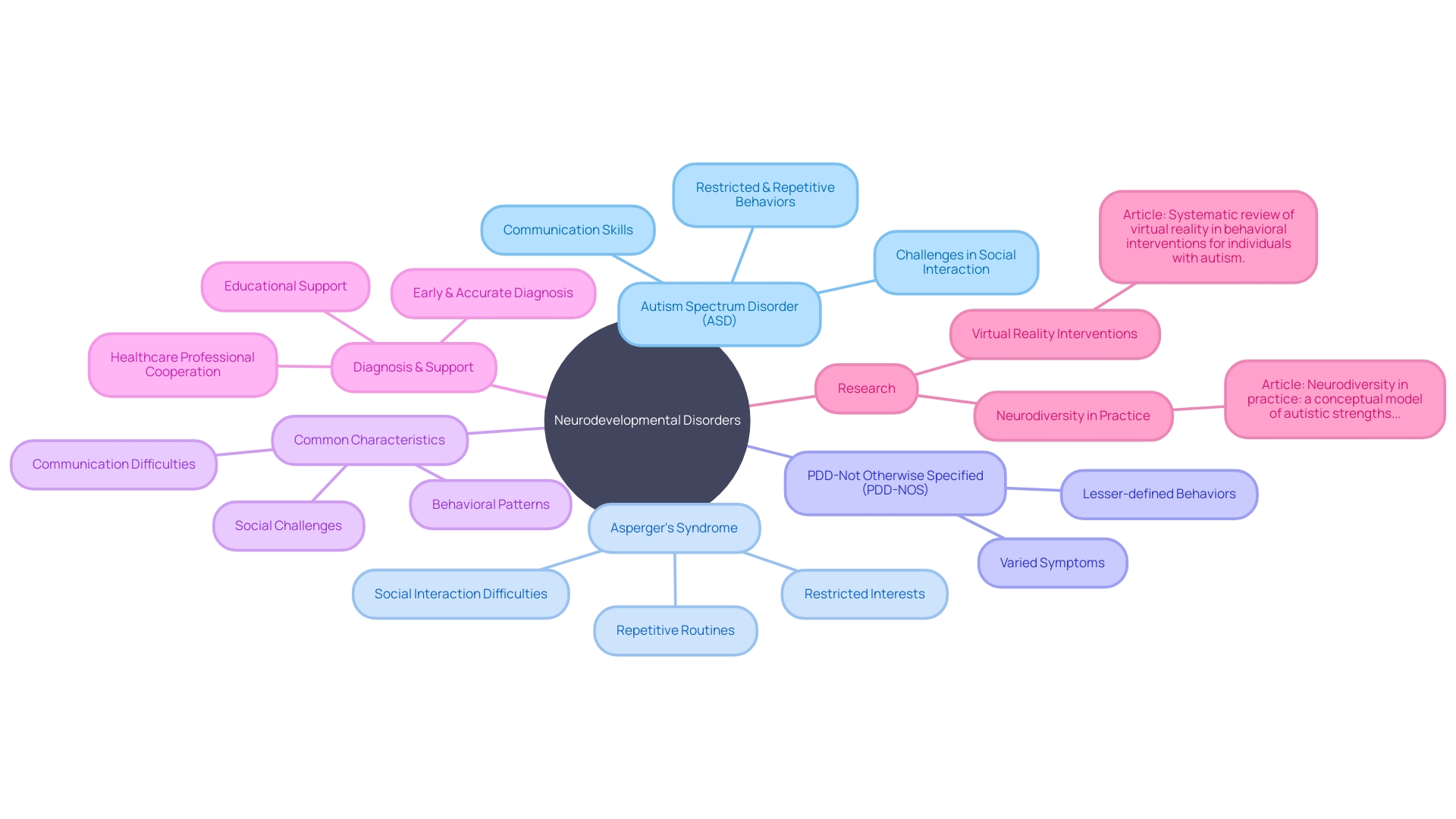
Neurodevelopmental Disorders, as classified by the DSM-5 and ICD-11, encompass a range of conditions with onset in the developmental period. These conditions are not due to sickness or injury but are present since birth, resulting in challenges in personal, social, academic, or occupational functioning. Under this umbrella, Autism Spectrum Disorder (ASD), Asperger's Syndrome, and PDD-Not Otherwise Specified (PDD-NOS) are identified as conditions associated with challenges in social interaction, communication skills, and often include restricted and repetitive behaviors.
The DSM-5 outlines specific criteria for diagnosing these disorders, while the ICD-11 provides a standardized framework for the recording, analysis, interpretation, and comparison of health data worldwide. Both systems aim to facilitate accurate diagnosis, which is crucial for intervention. In fact, organizations like The Autism Community in Action emphasize the importance of early and accurate diagnosis for ASD, linking it to improved outcomes through earlier access to interventions such as behavioral therapy.
Moreover, cooperation between healthcare professionals and a common comprehension of these diagnostic terms among providers can improve assistance for individuals with these conditions. This unified approach is essential for providing the necessary support in educational settings, where individuals with neurodevelopmental disorders often require additional assistance.
The Diagnostic Process for PDD
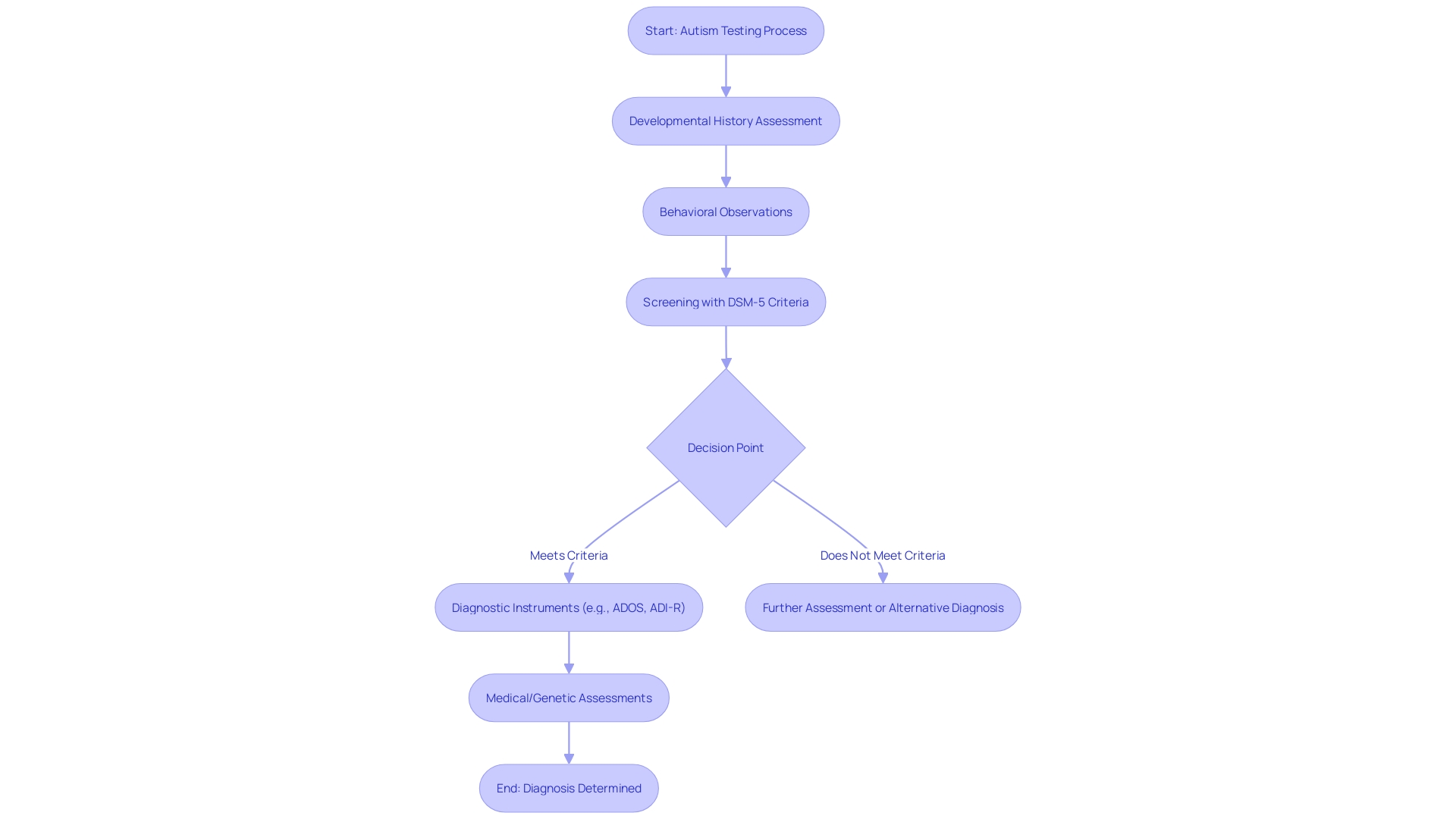
The journey to a Pervasive Developmental Disorder (PDD) diagnosis is intricate, involving a multidisciplinary team of experts who assess the individual comprehensively. This team typically includes psychologists, psychiatrists, speech-language pathologists, and occupational therapists, each playing a critical role in the evaluation. The process is multifaceted, beginning with an in-depth analysis of the person's developmental history and extending to careful observation of behavior and social interactions. Standardized assessment tools are employed to gain insights into the individual's condition. The ultimate aim is to ascertain if the individual meets the criteria for a PDD diagnosis, such as Autism Spectrum Disorder (ASD) or Asperger's Syndrome, and to pinpoint the specific type of PDD that is present. This careful and thorough diagnostic approach is essential, not only for determining the presence of PDD but also for guiding the direction of subsequent interventions and support.
Components of the Diagnostic Process
Autism testing is a multifaceted process, involving more than just answering a series of questions. It requires a thorough assessment of the developmental history that examines early milestones and any concerns raised by those closest to the individual. Observations of the child's behavior and social interactions are made in familiar environments like home and school. Instruments such as the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R) offer structured ways to evaluate symptoms. Moreover, medical and genetic assessments may be included to exclude other conditions.
For instance, at Children's National Hospital, which has one of the largest clinical genetics departments in the U.S., over 10,000 visits a year are from families seeking diagnoses for rare genetic disorders. This story parallels the autism diagnostic journey, underscoring the need for precision and thoroughness in identifying such complex conditions. Meanwhile, standard screenings like the M-CHAT-R/F are used during well-child visits, but research indicates they may not always capture autism accurately across all demographics. A study found that while the M-CHAT-R/F is specific, it lacks sensitivity and has a low positive predictive value, necessitating better screening tools to ensure equitable access to diagnosis and intervention.
The science of screening is intricate, especially for conditions like autism where signs can be subtle and vary greatly. It’s a process that involves comparing behaviors and development against standard benchmarks. Despite the challenges, such screenings are crucial because early detection and intervention are linked to significantly better outcomes. This principle is reinforced by the convergence of medical classification systems like the DSM-5 and ICD-11, both of which strive to provide clear diagnostics for neurodevelopmental conditions, facilitating shared understanding and interprofessional collaboration. These efforts are essential for empowering families and professionals to navigate the complexities of autism and advocate for the best possible support and interventions.
Multidisciplinary Approach to Treatment
The importance of a collaborative, multidisciplinary approach in treatment plans for individuals with pervasive developmental disorders (PDD) cannot be overstated. Such an approach draws on the expertise of behavioral therapists, speech-language pathologists, occupational therapists, and special education teachers, creating a comprehensive strategy tailored to the unique challenges and goals of each person affected by PDD. This team's synergy is pivotal in applying evidence-based interventions like Applied Behavior Analysis (ABA), speech therapy, social skills training, and sensory integration therapy, which are vital in managing PDD's core symptoms and fostering overall development and well-being.
Multidisciplinary care is especially crucial given the complex nature of neurological conditions, as highlighted by recent findings in Parkinson's disease research. Importantly, Parkinson's Disease At Risk Syndrome (PARS) outlines a progressive, often insidious disease course, emphasizing the significance of prompt and precise interventions. Similarly, in PDD, early and adaptive treatments are essential for addressing the multifaceted symptoms that may span various developmental stages and functional domains.
Advanced therapeutic models, such as adaptive deep brain stimulation (aDBS), underscore the potential benefits of real-time, responsive treatments. ADBS utilizes AI-derived methods to adjust therapy based on fluctuating symptoms, offering personalized symptom management. This idea of flexibility in therapy could be revolutionary for PDF care, ensuring interventions are as dynamic as the conditions they aim to treat.
Furthermore, a holistic approach to care is supported by the recognition that non-pharmacological strategies, including exercise, psychological interventions, acupuncture, and massage, can play a significant role in managing associated conditions like pain in Parkinson's disease. This reinforces the value of a multidisciplinary team in addressing the full spectrum of needs in individuals with PDD, potentially incorporating emerging therapeutic modalities that extend beyond conventional treatments.
Ultimately, the integration of various specialists in a multidisciplinary team is not just a preferred method; it's a cornerstone of effective treatment for PDD, ensuring that each individual receives the most comprehensive and adaptive care possible, reflective of the latest advancements and understanding in neurological and developmental condition management.
Importance of Early Detection and Intervention
Identifying the initial indications of pervasive developmental challenges (PDD) is crucial for initiating timely interventions that can change the course of a youngster's growth. Similar to neurodegenerative disorders such as Parkinson's disease, where a sequence of distinguishable stages takes place prior to clinical diagnosis, identification of PDD at an initial stage can result in notable improvements in communication, social skills, and adaptive behaviors. It is essential to understand that by the time neurodegenerative diseases are clinically apparent, considerable neuronal loss may have already taken place. Similarly, with PDF, catching those subtle yet pivotal changes in behavior and development can make a world of difference.
Screenings that detect PDD in the initial stages, particularly in children showing delays in speech and language, challenges in social interactions, and repetitive behaviors, enable parents and clinicians to pursue intervention strategies at the beginning. These strategies are much like those discussed in the Parkinson's Disease At Risk Syndrome (PARS) schema for pre-diagnostic stages of Parkinson's, aiming to identify and address issues before they fully manifest.
Recent discoveries in neurology highlight the importance of timely detection. For instance, a comprehensive meta-analysis revealed a higher prevalence of autoimmune disorders among individuals with Parkinson's disease, suggesting a pattern of immune dysregulation. This understanding of Parkinson's disease parallels the significance of identifying markers for PDD at an initial stage and promotes proactive health measures.
Furthermore, progress in AI and data analytics offer clinicians with potent tools for diagnosis and personalized treatment plans, as pointed out by Deloitte. These tools leverage vast amounts of medical data to support clinical decisions, emphasizing the promise of detection in improving population health outcomes. Considering such technological advancement, the role of the parent advocate becomes increasingly crucial in advocating for early screenings and assessments, utilizing these innovative resources to enhance their offspring's growth and welfare.
Parental Advocacy in PDD Diagnosis and Treatment
Parent advocates play a crucial role in guiding their offspring through the complexities of pervasive developmental disorders (PDD). Their distinct position, shaped by personal experiences with protective services for children, enables them to advocate effectively for the needs and rights of their offspring. These advocates engage with professionals to compile information, raise critical questions, and actively partake in the diagnostic process. They don't hesitate to seek additional opinions and leverage support networks, ensuring that they are conversant with contemporary research and advancements concerning PDD diagnosis and treatment.
Drawing from their lived experiences, parent advocates also contribute to the broader scope of safeguarding. Their involvement isn't merely confined to individual cases but also extends to influencing policy and organizational decisions. Through participation in advisory boards and initiating family-centered practices, they elevate the voice of experience in the formation of welfare policies. The powerful narratives of parent activists highlight their drive to instigate systemic change, confront power imbalances, and cultivate community empowerment.
The significance of a well-informed and engaged parent advocate cannot be overstated. As they navigate their offspring's journey through diagnosis and treatment, they not only empower themselves but also set the stage for improved well-being and outcomes for their children. It is this active involvement and advocacy that reinforces parents' roles as pivotal figures in the quest for a better understanding and management of PDD.
Supporting Parents and Caregivers
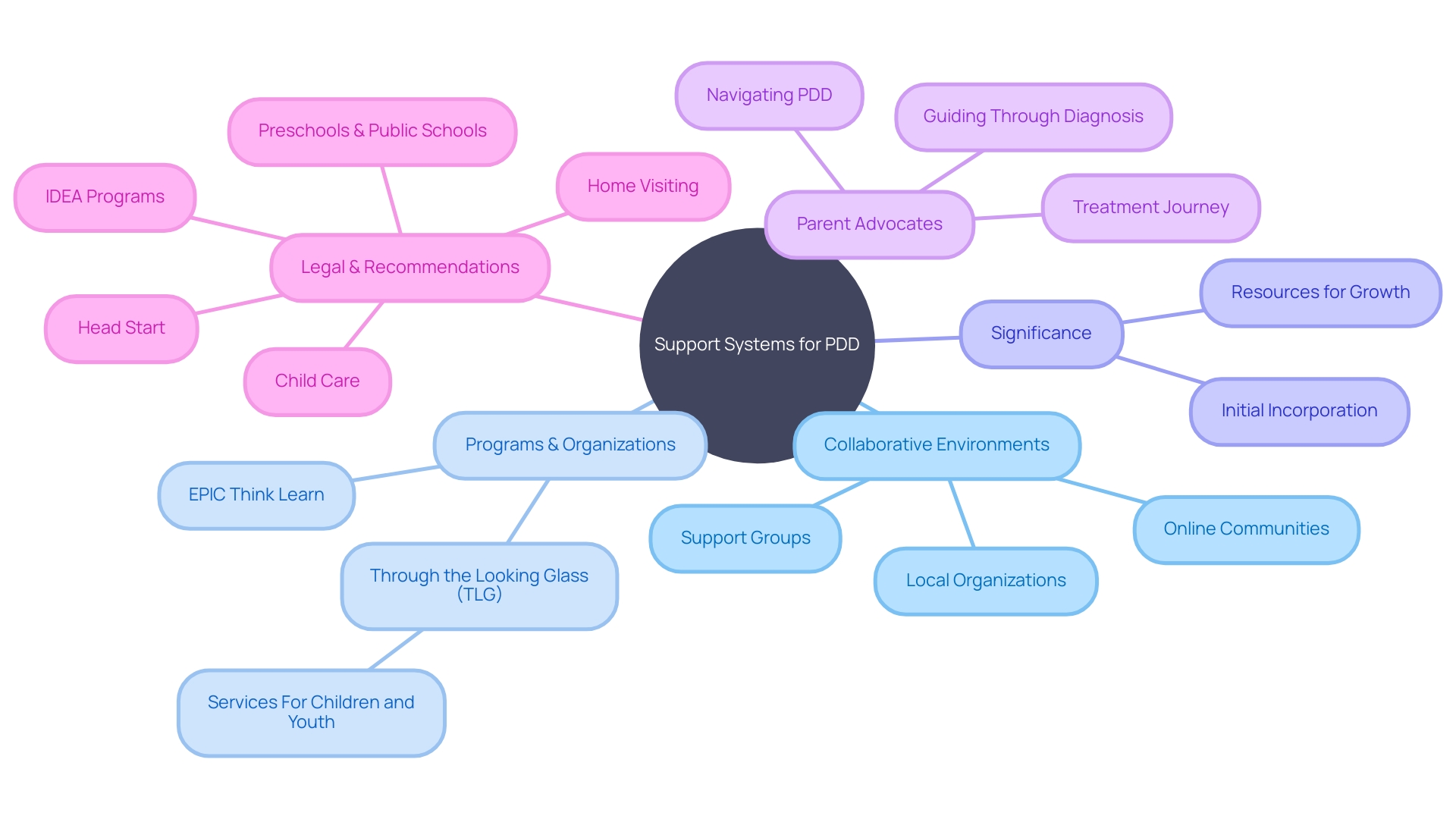
Navigating the complexities of pervasive developmental disorders (PDD) requires a robust support system for parents and caregivers. These committed individuals often face difficulties that can range from comprehending the intricate requirements of their offspring to accessing specialized services. Collaborative environments like support groups, online communities, and local organizations offer a sanctuary where parents can share insights, gain emotional support, and pool resources. Such networks are critical in promoting the equitable participation of individuals with disabilities in all life domains, as emphasized by psychiatrist Dr. David R. Offord, who advocated for a 'fair race' for all individuals.
Through the Looking Glass (TLG) exemplifies an organization that empowers families dealing with disabilities through its research, training, and services, emphasizing non-pathological approaches and the integration of personal disability experience. Furthermore, programs such as EPIC Think Learn address the personalized requirements of young individuals, whether identified or not, promoting comprehension and welfare through neuro affirmative activities. In the face of significant adversities, such as over 265,000 young individuals losing a caregiver to COVID-19, these support systems become even more vital.
The significance of initial incorporation cannot be emphasized enough, with ongoing endeavors to enhance public consciousness and strengthen legal backing for the incorporation of individuals with disabilities from the earliest stages. Ensuring that caregivers have the necessary resources to foster their children's growth and family well-being is a fundamental step toward a more inclusive society, as emphasized by the latest science and recommendations for early childhood programs. By fortifying these support structures, parent advocates can more effectively guide their children through the journey of PDD diagnosis and treatment.
Conclusion
In conclusion, navigating the complexities of Pervasive Developmental Disorders (PDD) requires a confident and supportive approach from Parent Advocates. Early detection and intervention play a crucial role in improving outcomes for children with PDD. By recognizing the early signs and seeking timely screenings, parents and clinicians can initiate interventions that enhance communication, social skills, and adaptive behaviors.
The diagnostic process for PDD involves a multidisciplinary team that carefully assesses the individual's developmental history and behavior, ensuring accurate diagnosis and guiding subsequent interventions. A collaborative, multidisciplinary approach to treatment is essential, drawing on the expertise of various specialists to tailor comprehensive strategies that address the unique challenges of each individual with PDD. Parent Advocates, with their lived experiences, play a vital role in the diagnostic process and contribute to the broader scope of child protection, advocating for their children's needs and rights.
A robust support system is crucial for parents and caregivers, providing them with resources, emotional support, and opportunities to share insights. By fortifying these support structures, Parent Advocates can effectively guide their children through the journey of PDD diagnosis and treatment, ensuring the best possible outcomes and fostering a more inclusive society.




