Overview
This article aims to illuminate the symptoms of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD), fostering a deeper understanding to support children affected by these conditions.
Recognizing the overlapping symptoms can be challenging, and navigating the complexities of diagnosis often adds to the emotional burden parents face.
By highlighting the necessity for tailored treatment strategies, we can empower families to take informed steps forward.
It is essential to remember that informed advocacy from parents can significantly enhance the management of these disorders, creating a positive impact on their children's lives.
Together, we can work towards a supportive environment that nurtures understanding and compassion.
Introduction
Navigating the intricacies of childhood mental health can feel overwhelming for parents, particularly when confronted with conditions like Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD). Each disorder presents its own unique challenges, yet their intersection can complicate both diagnosis and treatment.
OCD often manifests through persistent, intrusive thoughts and compulsive behaviors, while ADHD is characterized by inattention, hyperactivity, and impulsivity. This overlap can lead to confusion and misdiagnosis, making it essential for parents to grasp the nuances of each condition.
In this article, we will explore the key concepts surrounding OCD and ADHD, examine their prevalence and co-occurrence, and provide insights into effective treatment strategies. Our goal is to empower parents to advocate for their children’s mental health needs, fostering a supportive environment for their growth and well-being.
Defining OCD and ADHD: Key Concepts and Characteristics
Obsessive-Compulsive Disorder (OCD) is characterized by persistent, intrusive thoughts known as obsessions, paired with repetitive behaviors or mental acts called compulsions that individuals feel compelled to perform. Common obsessions may include fears of contamination, concerns about harming others, or a need for orderliness. In contrast, Attention-Deficit/Hyperactivity Disorder (ADHD) is defined by a pattern of inattention, hyperactivity, and impulsivity.
Youngsters facing attention difficulties often encounter challenges in maintaining concentration, completing assignments, and organizing their time effectively.
Understanding these definitions is crucial for parents, as it enables them to recognize potential indicators in their children and seek appropriate interventions. Research indicates that approximately 40% of youth diagnosed with ADHD also experience anxiety, complicating treatment methods, particularly when addressing OCD and ADHD symptoms. Moreover, the co-occurrence of OCD and ADHD symptoms calls for a deeper examination of their neurobiological connections, as ongoing studies strive to clarify how these symptoms interact.
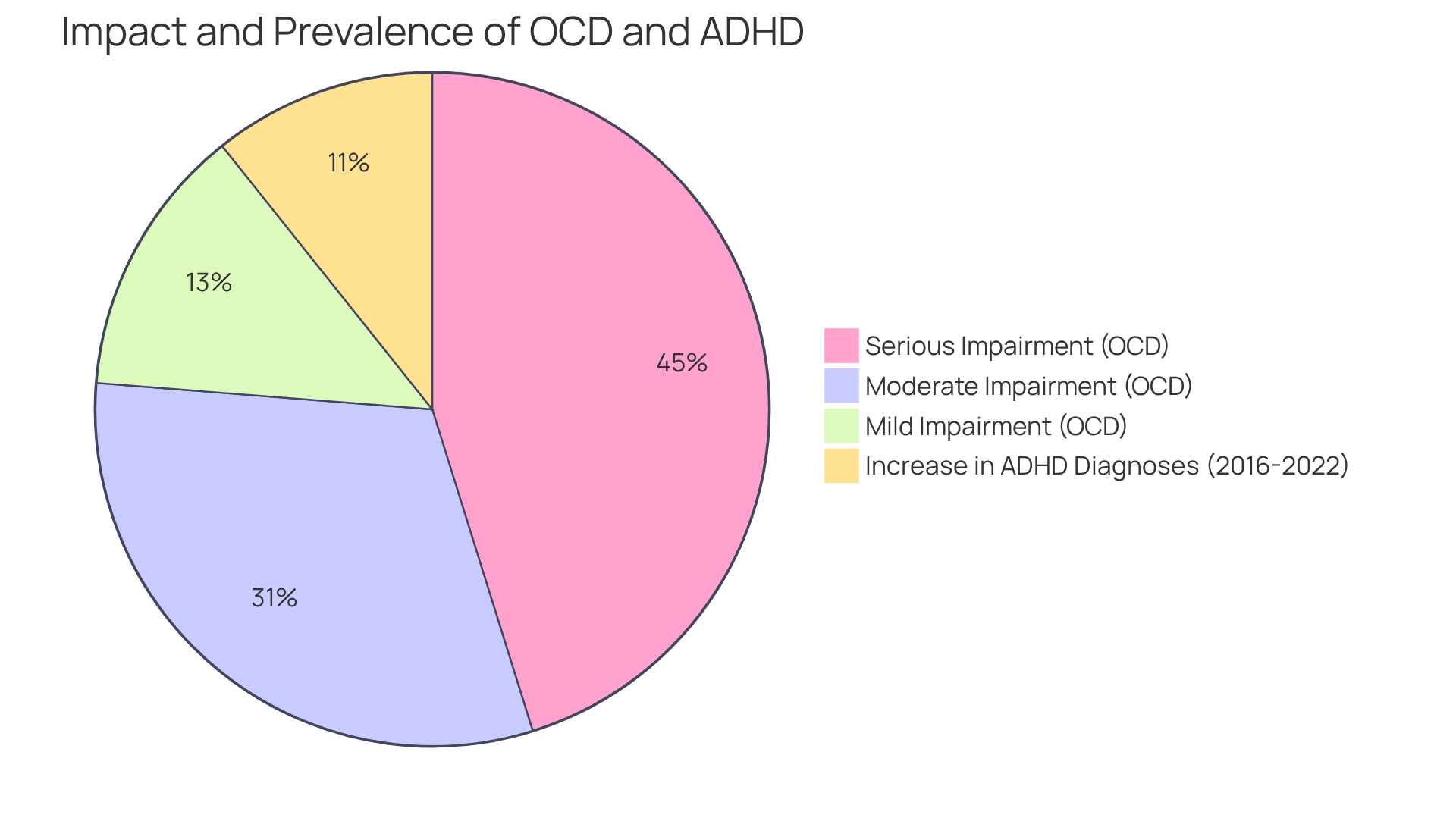
Real-world examples can effectively illustrate these conditions. For instance, a young person exhibiting both OCD and ADHD symptoms might find themselves washing their hands repeatedly due to an overwhelming fear of germs, while a student with these symptoms may struggle to remain still during class, frequently interrupting others. The prevalence of these disorders is significant; recent statistics reveal that the number of youngsters receiving behavioral intervention for ADHD rose from 2.5 million in 2016 to 2.8 million in 2022, highlighting a growing acknowledgment of the importance of behavioral therapy alongside medication.
This increase suggests that parents are becoming more aware of the need for effective intervention strategies.
Additionally, among adults with OCD in the past year, about 50.6% experienced serious impairment, 34.8% had moderate impairment, and 14.6% faced mild impairment, as determined by the Sheehan Disability Scale. This underscores the considerable impact OCD can have on daily functioning, further emphasizing the importance of understanding these conditions.
By familiarizing themselves with the characteristics of OCD and ADHD symptoms, parents can more effectively advocate for their children, ensuring they receive the necessary support and resources to thrive. This understanding not only aids in identifying symptoms but also empowers parents to engage with professionals effectively, fostering a collaborative approach to treatment. Furthermore, the CDC reported that in 2022, an additional 1 million U.S. youths aged 3-17 years had ever received a diagnosis of ADHD compared to 2016, underscoring the increasing prevalence of the condition and the need for informed advocacy.
Prevalence and Co-occurrence: Understanding the Intersection of OCD and ADHD
Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most prevalent psychiatric conditions affecting our youth today, impacting around 5.2% of the global pediatric population. In contrast, Obsessive-Compulsive Disorder (OCD) touches approximately 1-3% of young individuals. Importantly, research reveals that between 12% and 25% of children diagnosed with OCD also exhibit symptoms of ADHD, highlighting a significant overlap between these conditions.
This co-occurrence can complicate both diagnosis and care, making it essential for parents to recognize and understand how attention disorders interact with OCD and ADHD symptoms when seeking help for their children. Additionally, factors such as depression, autism spectrum disorder, and Tourette syndrome can further influence children with ADHD, adding layers of complexity to their care environment. A case study titled "Common Symptoms of Attention Deficit Hyperactivity Disorder" identifies specific symptoms like hyperactivity, impulsivity, and selective attention deficits that can hinder functioning in structured settings.
As Dr. Boduryan-Turner insightfully points out, "Abnormalities in neurotransmitter systems—chemicals such as serotonin, dopamine, and glutamate that send messages between brain cells—are also involved in the disorder." With the landscape of behavioral treatment evolving, the number of children receiving such interventions has risen from 2.5 million in 2016 to 2.8 million in 2022. This increase underscores the growing importance of being aware of co-occurring conditions for effective management and improved outcomes.
While the exact origins of OCD and ADHD symptoms remain unclear, it is believed to involve a combination of genetic, environmental, and neurobiological factors. Irregularities in neurotransmitter systems contribute to the complexity of understanding the co-occurrence of these symptoms. By fostering awareness and understanding, we can better support our children in their journeys.
Identifying Overlapping Symptoms: Navigating the Complexities of OCD and ADHD
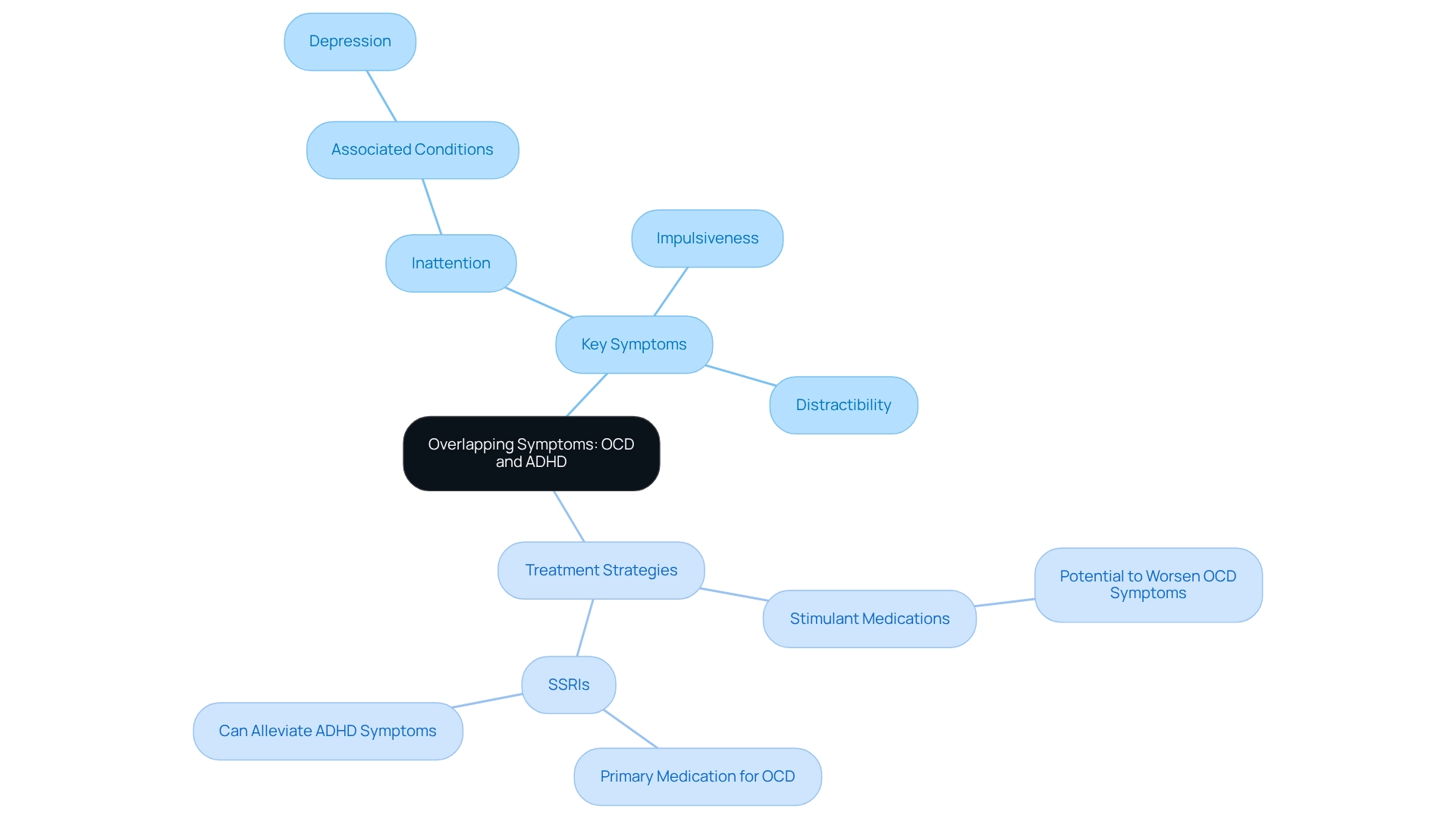
Navigating the complexities of OCD and ADHD can be challenging for parents, especially since both conditions share overlapping characteristics like inattention and distractibility. Imagine a child with OCD, seemingly distracted by intrusive thoughts, while another child struggles to focus due to impulsiveness. This similarity can lead to confusion, making it vital for parents to recognize these nuances.
It's important to note that around 40% of individuals with OCD also experience depression, underscoring the need for a holistic approach to care. Case studies, such as those in 'Treatment Considerations for Comorbid OCD and Attention Deficit Hyperactivity Disorder,' reveal that children diagnosed with both conditions often require tailored treatment strategies.
For instance, stimulant medications for ADHD may worsen OCD symptoms, while SSRIs, the primary medication for OCD, can sometimes alleviate ADHD symptoms. By identifying these overlapping symptoms, parents can better navigate the complexities of both conditions and seek appropriate interventions. As Edna Grunblatt wisely noted, understanding these nuances is crucial for effective management.
If you find yourself in this situation, remember that you are not alone. Sharing your experiences can provide support not only for yourself but for others facing similar challenges. Together, we can foster a community of understanding and compassion.
Diagnostic Challenges: Misunderstandings and Overlooked Symptoms
Diagnosing OCD and ADHD symptoms can be quite challenging, especially when their characteristics overlap, leading to potential misinterpretations. For example, clinicians might confuse compulsive behaviors associated with OCD for impulsivity typical of ADHD, or vice versa. This diagnostic ambiguity is heightened by the fact that the presence of one disorder can obscure the symptoms of the other, resulting in incomplete assessments.
Research shows that about 75% of individuals diagnosed with attention deficit hyperactivity disorder exhibit the impulsive/hyperactive (combined) type, complicating the diagnostic process even further when OCD and ADHD symptoms coexist.
A significant case study titled 'Neuropsychological Profiles of Subgroups' highlights the existence of disorder-specific subgroups within OCD and ADHD. It reveals that varying symptom dimensions can lead to different neuropsychological profiles, suggesting that comorbidity with other disorders can significantly influence the severity of neuropsychological deficits. For instance, children with both ADHD and OCD may experience distinct patterns of impairment shaped by their specific symptoms and any other coexisting conditions.
Interestingly, research indicates that the presence of OCD and ADHD symptoms in comorbid ADHD may lead to reduced neuropsychological impairment compared to pure OCD, particularly when hoarding symptoms are associated with childhood-onset OCD.
The rates of misdiagnosis for OCD and ADHD symptoms are concerning, as many clinicians may lack the nuanced understanding necessary to differentiate between the two. Experts stress the importance of comprehensive evaluations conducted by professionals experienced in both conditions. Parents, it is crucial to remain vigilant and proactive in seeking thorough assessments to ensure accurate diagnoses, as misunderstandings in diagnosing these disorders can lead to inappropriate treatment strategies.
Clinicians have noted that, unlike individuals with ADHD, those with OCD rarely display impulsive actions or risk-taking behaviors. As Amitai Abramovitch, PhD and Research Fellow at the OCD and Related Disorders Program at Massachusetts General Hospital, emphasizes, "Unlike those with attention deficit hyperactivity disorder from adolescence, people with OCD are very rarely impulsive and do not exhibit risk-taking behavior." This underscores the necessity for careful consideration during diagnosis.
In summary, the diagnostic challenges associated with OCD and ADHD symptoms call for a collaborative approach between parents and healthcare providers to ensure that all symptoms are accurately identified and addressed. Understanding the biological underpinnings, such as the linkage of OCD to chromosome 1 and contributions from chromosome 10, can further inform the diagnostic process and treatment options. Together, we can navigate this journey, ensuring that our children receive the care and support they need.
Impact on Daily Life: How OCD and ADHD Affect Children and Families
Children grappling with Obsessive-Compulsive Disorder (OCD) often face significant disruptions in their daily lives due to compulsive behaviors, such as excessive handwashing or repetitive checking rituals. These behaviors can lead to delays in task completion, resulting in increased frustration for both the young individual and their family. For instance, a young person may spend an inordinate amount of time ensuring that doors are locked or that their hands are clean, which can interfere with school schedules and family activities.
Similarly, children with Attention-Deficit/Hyperactivity Disorder (ADHD) often struggle with time management and organization. This can manifest as difficulty adhering to routines, completing homework, or following through on chores, further complicating family dynamics. The interplay between OCD and ADHD symptoms can intensify these challenges, creating a particularly trying environment for families.
Statistics reveal that it can take up to 17 years for individuals diagnosed with OCD to receive adequate therapy, underscoring the urgent need for effective intervention strategies. This delay highlights the importance of interprofessional healthcare teams, which are essential for managing OCD. These teams typically include:
- Primary care physicians
- Psychiatrists
- Clinical psychologists
- Occupational therapists
- Pharmacists
- Social workers
All collaborating to provide comprehensive support.
Moreover, Dr. Nicholas Farrell, Clinical Director at NOCD, emphasizes, "There is certainly a benefit to recognizing OCD subtypes," which can inform tailored treatment approaches. The collective impact of these circumstances not only affects the children but also reverberates through family life, necessitating a robust support system. Family therapists note that the challenges posed by OCD can strain relationships, disrupt family routines, and elevate stress levels among family members.
Real-world examples illustrate these challenges: a young person with OCD and ADHD symptoms may require extra time to prepare for school due to their compulsions, while a sibling with similar symptoms may struggle to maintain focus during family meals, leading to frustration and conflict. Cognitive and learning-based models of OCD suggest that maladaptive beliefs fuel obsessional anxiety, prompting compulsive behaviors aimed at alleviating such anxiety. Understanding these dynamics is crucial for parents and advocates seeking to support children effectively and foster a nurturing home environment.
Treatment Approaches: Strategies for Managing OCD and ADHD
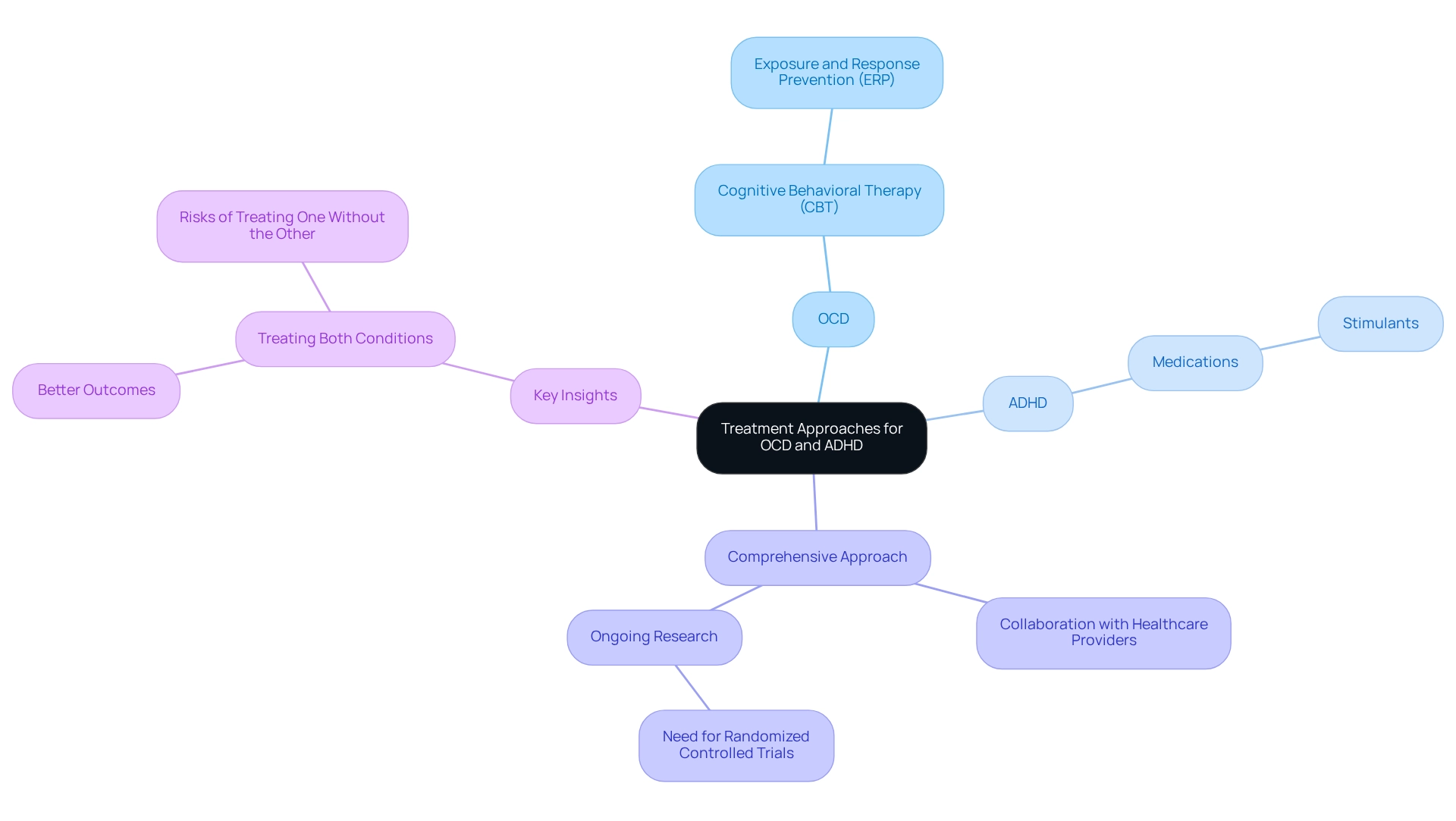
Effective intervention for obsessive-compulsive disorder (OCD) often centers around Cognitive Behavioral Therapy (CBT), particularly focusing on Exposure and Response Prevention (ERP). This nurturing therapeutic method encourages children to gradually face their fears, helping them build resilience and coping skills. For attention-deficit/hyperactivity disorder (ADHD), a combination of behavioral strategies and medications, such as stimulants, has proven beneficial.
When OCD and ADHD symptoms coexist, it is essential to adopt a comprehensive approach that addresses both conditions simultaneously. This is crucial for effective management and support.
Consider a significant case study that illustrates this approach: a 33-year-old patient diagnosed with OCD was later found to have adult ADHD. Initially treated with paroxetine and quetiapine, the patient did not experience adequate symptom relief. However, after incorporating extended-release methylphenidate (ER MPH) into the treatment plan, remarkable improvements were noted in both OCD and ADHD symptoms.
This case highlights the potential effectiveness of psychostimulants in managing comorbid conditions, while also underscoring the importance of consistent medication management to prevent symptom resurgence.
Parents are encouraged to collaborate closely with healthcare providers to develop a tailored care plan that meets their child's specific needs. Expert insights suggest that addressing both OCD and ADHD symptoms together can lead to improved outcomes. As ND wisely stated, "Treating one without the other leads to poorer outcomes in both, while treating both simultaneously is associated with better outcomes."
Furthermore, ongoing research is vital, with calls for more randomized controlled trials to standardize treatment options for the co-occurrence of OCD and ADHD. As the field evolves, particularly with the demand for additional studies, the integration of effective strategies like CBT and medication remains a cornerstone of treatment for young individuals facing the dual challenges of OCD and attention disorders. Together, we can foster a supportive environment for our children as they navigate these complexities.
Building Support Systems: Resources for Parents and Advocates
Parents navigating the complexities of OCD can find a wealth of resources designed to support their journey. Support groups play a crucial role, providing a platform for sharing experiences and strategies. Organizations like the International OCD Foundation and CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) are invaluable in offering information and fostering community connections.
These organizations not only provide educational materials but also facilitate local support groups, allowing parents to connect with others who face similar challenges. In a recent episode of the Parent Matters Podcast, Susan Stutzman emphasized the importance of community assistance, stating, 'Creating a support network is vital for parents as they manage the difficulties of raising kids with OCD and ADHD symptoms.' This perspective aligns with the advocacy for a community approach to support, rather than relying solely on psychiatric diagnoses that may lack scientific validity.
In addition to these organizations, local mental health experts can offer personalized support, helping families address the unique needs of their children. A case study on ADHD treatment highlights that a multifaceted approach is often the most effective; it revealed that 69.3% of children with ADHD received medication, while 47% participated in behavioral treatment. This underscores the importance of combining various strategies to effectively manage OCD and ADHD symptoms.
Moreover, expert opinions stress the necessity of community support systems for parents. Notably, around 20% of college students are managing ADHD while pursuing higher education, illustrating the ongoing need for resources that extend beyond childhood. By utilizing these support networks and educational resources, parents can advocate more effectively for their children and cultivate an environment conducive to growth and development.
ASD Media is dedicated to fostering collaboration and growth in the ABA therapy industry, ensuring that parents have access to the support they need.
Coping Strategies: Practical Tips for Families Navigating OCD and ADHD
Families navigating the dual challenges of OCD and ADHD symptoms can embrace a range of effective coping strategies to enrich their daily lives. One of the most essential methods is establishing structured routines, which provide young individuals with a sense of security and predictability, ultimately alleviating anxiety levels. Research indicates that children often encounter heightened difficulties in social functioning and emotional control due to OCD and ADHD symptoms, making the implementation of routines even more vital.
A study highlighted that individuals with OCD and ADHD symptoms experience additional challenges in social interactions, academic settings, and self-reported feelings of depression. This underscores the importance of organized routines in addressing these hurdles.
Incorporating mindfulness techniques, such as deep breathing exercises and meditation, can significantly alleviate stress for both children and their families. These practices not only assist in managing immediate anxiety but also foster long-term emotional resilience. Moreover, nurturing open communication within the family is crucial.
Encouraging children to express their feelings and challenges creates a supportive environment where they feel safe to share. As James F. Leckman, M.D., from the Yale University School of Medicine, noted, "These results align with prior reports in which youngsters with OCD were impaired and comparable to matched psychiatric comparison subjects on overall assessments of functioning."
Real-world examples demonstrate the effectiveness of these strategies. For instance, families that have initiated regular family meetings report improved understanding and cohesion, which are essential in managing the complexities of OCD and related conditions. Counselors frequently emphasize the significance of these discussions, suggesting they can lead to enhanced coping mechanisms and a stronger family bond.
This aligns with ASD Media's mission to foster collaboration and growth within the ABA therapy industry, as sharing experiences can empower families.
Ultimately, by prioritizing structured routines and open dialogue, families can cultivate a nurturing atmosphere that empowers children to manage their OCD and ADHD symptoms more effectively. This holistic approach not only addresses the immediate challenges posed by OCD and ADHD but also nurtures long-term growth and resilience.

Conclusion
Understanding the complexities of Obsessive-Compulsive Disorder (OCD) and Attention-Deficit/Hyperactivity Disorder (ADHD) is crucial for parents striving to support their children's mental health. This article has explored definitions of these disorders, examined their prevalence and co-occurrence, and highlighted the overlapping symptoms that can complicate diagnosis and treatment. Recognizing the nuances of each condition empowers parents to advocate effectively for their children, ensuring they receive the necessary support and appropriate interventions.
The intersection of OCD and ADHD presents unique challenges, marked by the significant overlap in symptoms and the potential for misdiagnosis. Parents must remain vigilant in identifying these issues, as accurate diagnosis is critical for effective treatment. The impact of these disorders on daily life can be profound, affecting not only the children but also their families. Implementing structured routines, fostering open communication, and utilizing community resources can enhance coping strategies and create a supportive environment for growth.
Ultimately, parents are encouraged to collaborate with healthcare professionals to develop comprehensive treatment plans that address both conditions simultaneously. This holistic approach is vital, as treating one disorder without considering the other can lead to poorer outcomes. By leveraging the insights and strategies discussed, parents can navigate the complexities of OCD and ADHD with confidence, fostering resilience and well-being for their children in the face of these challenges.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
OCD is characterized by persistent, intrusive thoughts known as obsessions, which are paired with repetitive behaviors or mental acts called compulsions that individuals feel compelled to perform.
What are common obsessions associated with OCD?
Common obsessions may include fears of contamination, concerns about harming others, or a need for orderliness.
How is Attention-Deficit/Hyperactivity Disorder (ADHD) defined?
ADHD is defined by a pattern of inattention, hyperactivity, and impulsivity, often leading to challenges in maintaining concentration, completing assignments, and organizing time effectively.
What percentage of youth diagnosed with ADHD also experience anxiety?
Approximately 40% of youth diagnosed with ADHD also experience anxiety, which complicates treatment methods for OCD and ADHD symptoms.
Why is it important for parents to understand OCD and ADHD?
Understanding these conditions helps parents recognize potential indicators in their children and seek appropriate interventions, enabling them to advocate effectively for their children's needs.
What is the significance of the increase in behavioral interventions for ADHD from 2016 to 2022?
The number of youngsters receiving behavioral intervention for ADHD rose from 2.5 million in 2016 to 2.8 million in 2022, indicating a growing awareness of the importance of behavioral therapy alongside medication.
What impact does OCD have on adults?
Among adults with OCD, 50.6% experienced serious impairment, 34.8% faced moderate impairment, and 14.6% had mild impairment, highlighting the significant impact OCD can have on daily functioning.
How prevalent is ADHD among youth?
ADHD affects around 5.2% of the global pediatric population, while OCD touches approximately 1-3% of young individuals.
What is the overlap between OCD and ADHD in children?
Research reveals that between 12% and 25% of children diagnosed with OCD also exhibit symptoms of ADHD, indicating a significant overlap that complicates diagnosis and care.
What factors can influence children with ADHD?
Factors such as depression, autism spectrum disorder, and Tourette syndrome can add complexity to the care of children with ADHD.
What role do neurotransmitter systems play in ADHD and OCD?
Abnormalities in neurotransmitter systems, such as serotonin, dopamine, and glutamate, are involved in both disorders, contributing to the complexity of their symptoms and co-occurrence.




