Introduction
Autism Spectrum Disorder (ASD) presents a unique set of challenges, impacting social skills, communication abilities, and leading to repetitive behaviors. With a prevalence of 1 in 45 adults in the U.S., it is crucial to understand the far-reaching implications of ASD, especially when it intersects with mental health conditions like depression. The prevalence of depression among those with ASD surpasses that of the general population.
However, diagnosing depression in individuals with ASD can be challenging due to overlapping symptoms and communication difficulties. Tailored support and interventions are necessary to address this disparity and ensure the mental well-being of those on the spectrum. This article explores the complexities of living with ASD and depression, the symptoms of depression in autistic individuals, contributing factors, strategies for supporting individuals with ASD and depression, therapeutic interventions, and the pivotal role of family and caregivers in creating a supportive environment.
By embracing a compassionate and informed approach, we can empower and uplift the autism community, promoting inclusivity and enhancing the quality of life for all.
Understanding Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) presents as a constellation of challenges, primarily impacting social skills, communication abilities, and leading to distinctive, repetitive behaviors. In its essence, ASD embodies a diverse array of manifestations, which can range from mild to profound, making each individual's experience with autism uniquely their own. The recognition of these variations is not only about understanding the struggles but also about appreciating the strengths that autism brings to the individual and their community.
Central to supporting individuals with ASD is acknowledging the profound impact that autism has within the family unit. Parents, who serve as the primary caregivers, are instrumental in fostering a nurturing and supportive environment for their child's development. They face the daunting task of balancing the need to address repetitive behaviors, facilitate social integration, and manage any co-occurring emotional and behavioral issues.
These daily endeavors are done with the hope of equipping their children for fair participation across various life domains, be it in educational settings or social circles.
Stem cell scientists have made headway in developing models to study human cerebellar development and disease, which can shed light on autism. Moreover, research indicates a potentially significant relationship between prenatal exposure to dopamine-related drugs and the likelihood of autism in children. Understanding the intricate interplay between neurotransmitters like dopamine and serotonin with autism offers a promising avenue for therapeutic innovations.
According to the latest reports, 1 in 45 adults in the U.S. have been diagnosed with ASD. This calls for heightened awareness and screening measures to identify and extend necessary support to those who may have slipped through the cracks without a formal diagnosis, continuing to contend with challenges unbeknownst to them. Adults with ASD encounter obstacles that span social interactions and sensory sensitivities, regardless of their functional capabilities and intellectual prowess.
The journey towards diagnosis and obtaining support can be replete with barriers, particularly for adults seeking comprehension of their condition in retrospect. Understanding ASD is not a static endeavor; it is an ongoing process that must involve a holistic look at the individual's developmental history, cognitive function, and feedback from self-report questionnaires.
Understanding ASD's far-reaching implications requires an interdisciplinary approach, integrating insights from caregiving science, behavioral observation, and the lived experiences of autistic individuals and their families. This approach must be grounded in compassion, equity, and a dedication to making society inclusively supportive for all.
Prevalence of Depression in Individuals with ASD
Autism Spectrum Disorder (ASD) extends far beyond its direct effects on an individual's communication and behavior, with the intersection of autism and mental health garnering increased attention. Studies have illuminated a concerning trend: the prevalence of depression amongst those with ASD surpassing that of the general populace. The intricacies of ASD complicate the diagnosis and management of co-existing conditions like depression.
Symptoms can be masked or altered by the underlying traits of autism, such as atypical expressions of distress or social withdrawal.
As adolescents with autism approach adulthood—whether diagnosed in youth or later in life—they and their families may face distinct psychological and societal challenges. The expression of mood disorders, including depression, in individuals with ASD can vary, featuring both verbal and non-verbal signs. One may see manifestations like moral distress, difficulties with social interaction, or behavioral changes.
Healthcare practitioners often play a critical role in managing these conditions but may lack specific training for autistic adults' needs, creating a barrier to effective care.
Contrary to the assumption that current therapeutic approaches are unsuitable for autistic individuals, the core therapeutic needs for conditions such as anxiety and depression align closely with those of the broader population. Yet, many adults with autism report difficulty accessing mental health services, facing rejection from healthcare providers unequipped or unwilling to accommodate their needs. This highlights a gap in healthcare delivery that, with minimal training and an openness to learn, could be closed, allowing for more inclusive and understanding care.
The collective mental health landscape in the United States points to a broader societal issue, with 1 in 6 U.S. youth facing mental health disorders annually, and suicide ranking as a leading cause of death in young individuals. ASD adds a layer of complexity to these statistics. Autistic individuals encounter a higher risk of several physical and mental health conditions, contributing to a disparity in life expectancy and unmet healthcare needs.
This increased vulnerability underscores the urgent need for tailored support and interventions, which respect the unique strengths and communication styles of those with ASD.
Efforts to bridge the mental health services gap for this underserved population must acknowledge the societal, communication, and behavioral nuances of ASD. Understanding and responsiveness from the community and healthcare professionals can help to promote better health outcomes and enhance the quality of life for those on the spectrum.
Symptoms of Depression in Individuals with ASD
Understanding autism spectrum disorder (ASD) involves a nuanced approach, particularly when it comes to recognizing overlapping conditions such as depression. Unlike neurotypical individuals, adults with ASD may display unconventional indicators of depressive states, including heightened irritability, aggression, and in some cases, self-harm behaviors. With ASD in adults regularly presenting distinct challenges in social communication and behavior, depression can add a layer of complexity to their lives, necessitating a compassionate, tailored understanding from both their support networks and healthcare providers.
The prevalence of ASD in adulthood is significant, with statistics highlighting that approximately 1 in 45 adults in the U.S. are on the autism spectrum. Challenges for individuals with ASD persist into adulthood, encompassing psychological and societal hurdles, particularly if the autism diagnosis comes later in life. The co-occurrence of conditions like depression, which can be as common in autistic adults as in the broader population, demands recognition and appropriate intervention.
Unfortunately, many adults on the spectrum report difficulties in accessing specialized care, citing experiences of being turned away by practitioners reluctant to integrate autistic patients into their caseloads.
Despite these roadblocks, research shows that the therapeutic requirements for dealing with conditions such as anxiety or depression in autistic adults are not vastly different from those of other adults. However, a willingness to understand the specific needs of this demographic and a commitment to adjust standard therapeutic practices is critical. As stated by professionals in the field, even a modest increase in training can empower healthcare providers to competently include autistic adults in their range of services.
This not only supports the mental health needs of the autistic community but also builds on their strengths and fosters mutual trust.
Challenges in Diagnosing Depression in ASD
The intersection of autism spectrum disorder (ASD) and mental health conditions, such as depression, presents unique diagnostic challenges due to the intricate nature of overlapping symptoms and diversity in emotional expression among individuals with ASD. A notable concern is the atypical manifestation of responses to emotions or distress, which can lead to the underdiagnosis or misdiagnosis of depression in autistic individuals. It becomes essential to acknowledge that a standard approach may overlook critical aspects of their experience.
This underscores the need for professionals and caregivers to tailor their evaluative practices and to cultivate a deep understanding of these nuances to support accurate diagnosis and appropriate care.
Recent studies support this need for a nuanced approach. For example, it is reported that autistic individuals face a substantial risk of comorbid physical and mental health issues and are subject to a markedly higher mortality rate. This concern is due in part to the prevalence of neurological disorders, cancer, and a risk of suicide that cannot be solely attributed to these factors.
Often, these conditions can mask or be masked by depression, which calls for healthcare providers to be acutely perceptive to ensure that needs are met.
The significance of tailored mental health care for those with ASD is highlighted by research from the UCL, which found that autistic adults are considerably less likely to engage in Talking Therapies for Anxiety, a standard treatment offered by the NHS for depression and anxiety, compared to the general population. This discrepancy may partly stem from an information-processing divergence that leads to a preference for visual materials over impromptu verbal communication and the need for more detailed, predictable instructions about treatment expectations. To address these barriers, experts suggest customizing mental healthcare services, considering the sensory sensitivities of autistic individuals, to foster a more inclusive and accessible environment for their therapeutic journey.
Moreover, statistics reveal the importance of evaluating the concept of social competence, acknowledging that neurotypical definitions may not fully represent the skills and experiences of autistic people themselves. The inclusion of diverse measures to assess social competence can better reflect the complexity of social interactions and its correlation with mental health outcomes such as self-esteem and anxiety. Consequently, recognizing these differences is crucial for healthcare providers to build trust and rapport with autistic individuals.
For many adults with ASD, especially those who may have gone undiagnosed or misdiagnosed, learning about common autism signs can be a vital first step. As awareness of autism continues to grow, it's important that we understand how the hallmarks of autism—social communication challenges and restricted, repetitive behaviors—manifest in adulthood. By acknowledging the psychological and societal hurdles faced, and by reinforcing the strengths that autistic patients bring forth, we can begin to tailor our support and services to better accommodate the unique dimensions of autism.
Professionals are called upon to rise to the occasion by embracing a willingness to learn and adapt, which can significantly enhance their capacity to include autistic patients in their care programs. Self-education about autism and open-mindedness to modify standard practices enable practitioners to better address the complex needs that accompany ASD, particularly when specialized referrals are not readily available. This approach not only fosters trust but also aligns with core medical values that emphasize patient-focused care and the betterment of health outcomes.
Factors Contributing to Depression in ASD
Grasping the complexities of living with autism spectrum disorder (ASD) necessitates an understanding of the various factors that may contribute to mental health challenges, such as depression. Research and studies repeatedly reveal that individuals with ASD are at a heightened risk for depression due to a confluence of social and environmental factors. Among these, social isolation stands out as a critical component.
Findings from a comprehensive review place approximately half of Americans within the spectrum of loneliness, a condition exacerbated for those with ASD due to difficulties in initiating and maintaining social connections.
Communication challenges are also central to the ASD experience, impacting not only personal relationships but also educational and professional success. Peer-reviewed research has linked these challenges directly to depression in autistic adolescents, where unique non-verbal expressions and behavioral responses may signify underlying distress. Moreover, academic hurdles often intersect with ASD in a profound manner, as demonstrated by studies of 'twice-exceptional' students—those with autism who also exhibit exceptional academic talents.
These individuals require tailored support to navigate the pressures of conforming to neurotypical environments, especially in rigorous academic settings.
Further complicating the picture is the issue of 'social camouflage'—the adaptive behavior of mimicking neurotypical social cues to fit in—which can be especially burdensome in cultures that prize conformity over individuality. This is seen in countries like Japan, where the discrepancy between social expectations and the authentic expression of autistic individuals can lead to significant mental health struggles. Such cultural nuances underscore the need for context-specific understanding and support.
The intertwined facets of social and communication difficulties, sensitivity to sensory stimuli, experiences of bullying, and the stresses of academic demands contribute significantly to the risk of depression in individuals with ASD. Addressing these elements through informed, compassionate practices—recognizing the need for social support, offering strategies to aid communication, and developing inclusive academic environments—is paramount in fostering the mental well-being of those on the autism spectrum.
Strategies for Supporting Individuals with ASD and Depression
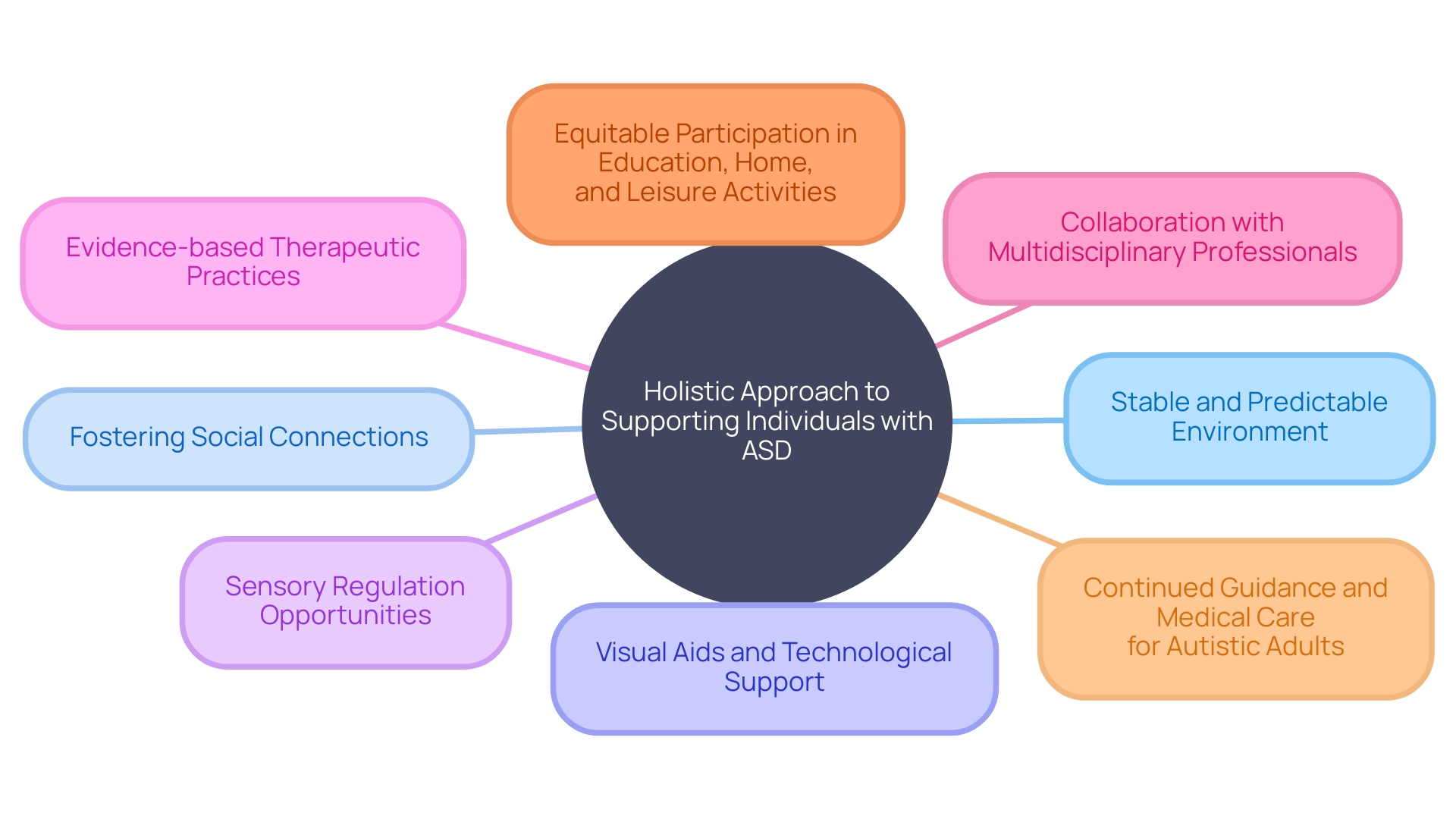
To optimally support individuals with Autism Spectrum Disorder (ASD) who may also be grappling with depression, an intricate and customized strategy must be embraced. Practices such as establishing a stable and predictable environment can significantly bolster their sense of security. Fostering social connections enhances inclusivity, which, in tandem with visual aids and technological support, can substantially mitigate their daily challenges.
Another key element involves affording sensory regulation opportunities coupled with evidence-based therapeutic practices, recognizing that autism and mental health are closely intertwined. As renowned child psychiatrist Dr. David (Dan) R. Offord articulated, a society that ensures equitable participation for all its children, including those with disabilities, in educational, home, and leisure activities, is one that is committed to mental health and fairness. This holistic approach benefits not only the individuals directly affected but also their caregivers by reducing stress and bridging the resource gap.
This method's efficacy is underpinned by active collaboration with multidisciplinary professionals. It aligns with insights from leading organizations, such as the Interagency Autism Coordinating Committee (IACC), which strives to enhance the coordination of autism research and services, reflecting a broader, community-inclusive initiative. Similar sentiments are echoed by specialists like Christopher McDougle of Harvard Medical School and the Lurie Center for Autism, who emphasizes the critical need for continued guidance and medical care for autistic adults after they transition out of the school system.
It is through personalized care plans, which cater to the specificities of each individual, that we can truly support and uplift the autism community, ensuring that every child and adult with ASD can lead a productive life with dignity and respect.
Therapeutic Interventions for Depression in ASD
Depression, a somber shadow affecting millions, touches not only individuals but seeps into family dynamics. Statistics paint a stark reality: about 37 million people, or 7.2% of the EU populace, were embroiled in a battle with chronic depression as of 2019. For those navigating life on the autism spectrum, the confluence of ASD characteristics and depression can pose unique challenges, necessitating tailored therapeutic interventions.
Cognitive-behavioral therapy (CBT), a beacon of hope, is particularly efficacious, dispelling depressive symptoms by restructuring negative thought patterns. Social skills training empowers individuals with ASD to traverse the intricacies of interpersonal interactions, potentially alleviating social contributors to depression. Meanwhile, mindfulness-based strategies offer a tranquil harbor, teaching presence and acceptance to weather emotional turbulence.
Where indicated, medication becomes a vital ally, working in concert with therapy to restore equilibrium.
To foster a "fair race" in mental health - a vision advocated by the late Dr. David (Dan) R. Offord - we must ally ourselves with seasoned professionals who comprehend the subtleties of autism. They are the cornerstones in constructing a supportive edifice for individuals and their families, ensuring that each therapeutic journey is as individualized as the lives it seeks to uplift.
Amidst a bustling landscape of developmental research, emerging studies highlight the intricate roles of dopamine and serotonin, magnifying our understanding of how these neurotransmitters may guide the formation of neural circuits. With ongoing examination, we strive to unearth innovative therapeutic targets, promising a paradigm shift in autism treatment.
Education, in parallel to therapeutics, is pivotal. Approaches such as the TEACCH program harness visual learning and consistency, transforming classrooms into crucibles of progress. We must also heed the calls for inclusivity in existing practices, recognizing that with modest adjustments, practitioners can competently address the therapeutic needs of autistic adults, who often encounter barriers in accessing specialized care.
In summary, comprehensive, evidence-based interventions, buttressed by communal insights and supported by vigilant research, can illuminate the path toward well-being for individuals with ASD and their families. Whether through psychological therapies, medicinal supplements, or educational fortification, it is a collective endeavor to harmonize the rhythm of life's race.
Role of Family and Caregivers in Support
Supporting individuals with Autism Spectrum Disorder (ASD), especially when accompanied by depression, calls for a compassionate and informed approach by families and caregivers. Embracing the values of engagement and equitable treatment championed by the late Dr. David Offord, families are key to offering a fair chance for loved ones with ASD in all areas of their lives. It involves creating environments that are not only nurturing but also lessen stress and acknowledge the unique contributions individuals with ASD bring to society.
In the spirit of making every race a fair one, caregivers are encouraged to immerse themselves in the understanding of both ASD and depression, seeking inclusive professional advice where available and tirelessly advocating for adequate resources to support the holistic development and welfare of individuals with ASD.
Case studies such as those from healthcare leader Christine Sakdalan illuminate the profound impact that committed family support can have on mental health management, highlighting the enduring courage and dedication needed to navigate the healthcare system with a loved one facing mental health challenges. News insights further inform that the journey of supporting those with ASD extends beyond behavior and communication challenges, with the need for awareness and sensitivity being paramount amongst all social interactions. Recognizing that the nurturing of an autistic identity is essential in both personal and communal spheres, it is also essential to appreciate that this identity development is a continuous process, profoundly influencing one's sense of self and interaction with others.
Ultimately, by ensuring engaged and peaceful participation in education, home life, and leisure activities, and by providing a comprehensive support network, families and caregivers champion the mental health and well-being of individuals with ASD, making strides towards a society that honors equality, acknowledges individual needs and celebrates the assets of every member, especially those with disabilities.
Creating a Supportive Environment
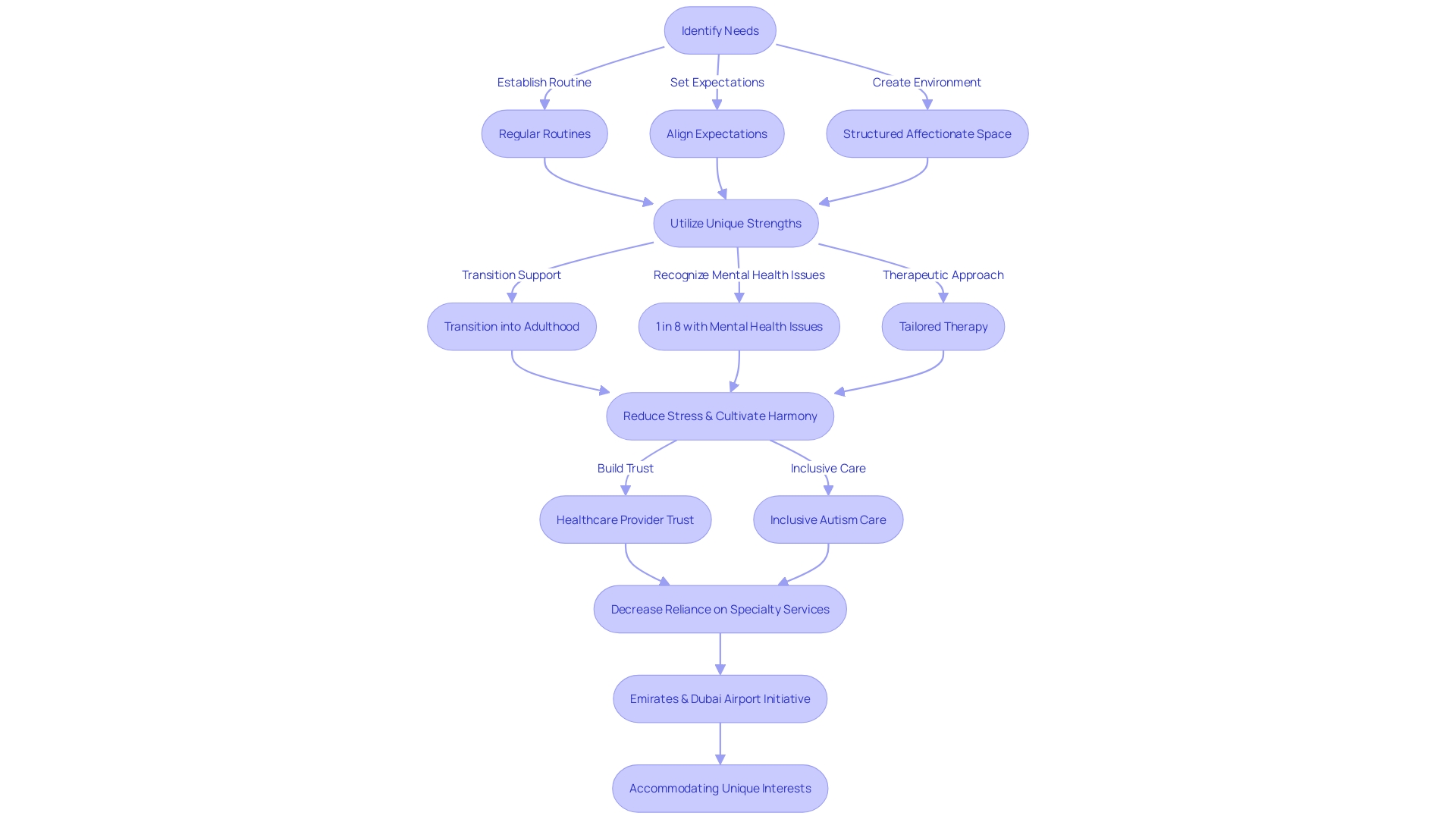
Establishing regular routines, aligning expectations, and cultivating a structured yet affectionate space are pivotal in supporting the well-being of individuals with Autism Spectrum Disorder (ASD) and depression. It's crucial to recognize and mobilize the unique strengths of autistic individuals as they transition into adulthood or receive later diagnoses, acknowledging their desire to contribute meaningfully to their communities. In line with Dr. David (Dan) R. Offord's vision of a fair race for every child, a harmonious environment can significantly influence mental health and help in reducing stressors, which is particularly vital given that a staggering 8 in 10 autistic individuals report experiencing mental health issues.
Moreover, tailored therapeutic approaches, akin to those of neurotypical individuals but delivered with additional understanding and patience, can make a considerable difference in the lives of autistic adults. By doing so, healthcare providers can foster trust and make autism care more inclusive without referring to scarce specialty services. As we see with initiatives like the one by Emirates and the Dubai International Airport, understanding and accommodating an autistic individual's unique interests, like Humza's passion for airplanes, can make experiences like traveling less daunting and more enjoyable.
This underscores the need for supportive environments that validate the identity and autonomy of autistic individuals, facilitating their participation and well-being across all aspects of life.
Conclusion
Supporting individuals with Autism Spectrum Disorder (ASD) and depression requires a compassionate and informed approach. The complexities of ASD, such as social isolation and communication challenges, contribute to an increased risk of depression. Diagnosing depression in individuals with ASD can be challenging due to overlapping symptoms, necessitating tailored understanding from caregivers and healthcare providers.
Various factors, including social isolation, communication difficulties, academic challenges, and cultural expectations, contribute to depression in individuals with ASD. Creating personalized strategies and inclusive environments can enhance mental well-being.
Therapies like cognitive-behavioral therapy (CBT), social skills training, mindfulness-based strategies, and medication can help individuals with ASD and depression. Collaborating with professionals experienced in working with autism is vital for effective treatment.
Family and caregivers play a pivotal role in supporting individuals with ASD and depression. Nurturing a nurturing and inclusive environment, advocating for their loved ones, and creating comprehensive support networks champion mental health and well-being.
Creating a supportive environment involves establishing routines, aligning expectations, and recognizing the strengths and interests of individuals with ASD. By providing tailored therapies and nurturing their sense of identity, we can make a significant difference in their lives.
In conclusion, supporting individuals with ASD and depression requires a compassionate and informed approach. By embracing this approach and collaborating with professionals, families, and caregivers, we can empower and uplift the autism community, promoting inclusivity and enhancing the quality of life for all.




