Overview
To effectively add ADHD and OCD management techniques to your daily routine, individuals should incorporate structured organizational strategies, mindfulness practices, and build support networks. The article emphasizes that combining behavioral therapies with daily management tools, such as visual schedules and mindfulness exercises, significantly enhances coping abilities and overall quality of life for those experiencing both conditions.
Introduction
The intricate relationship between Attention-Deficit/Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder (OCD) presents a unique challenge for many individuals and their families. While ADHD is characterized by symptoms such as inattention and impulsivity, OCD manifests through distressing intrusive thoughts and compulsive behaviors. Recent studies reveal a significant co-occurrence of these two conditions, with rates varying widely, highlighting the complexity of their interplay.
As awareness grows regarding the importance of recognizing ADHD symptoms in the management of OCD, it becomes evident that tailored treatment approaches are essential. This article delves into the nuances of ADHD and OCD, exploring their symptoms, effective therapeutic strategies, daily management techniques, and the vital role of support networks and mindfulness practices in enhancing the quality of life for those affected.
Understanding ADHD and OCD: A Complex Relationship
Attention-Deficit/Hyperactivity Disorder and OCD (Obsessive-Compulsive Disorder) are both distinct yet frequently co-occurring conditions that add ADHD OCD challenges for individuals and their families. Attention Deficit Hyperactivity Disorder is marked by signs such as inattention, hyperactivity, and impulsivity, whereas Obsessive-Compulsive Disorder presents through unwanted intrusive thoughts (obsessions) and repetitive actions (compulsions). Recent studies indicate that the co-occurrence rates of attention deficit hyperactivity disorder and OCD can vary significantly, ranging from 0% to 60% across different research, which underscores the complexity of their relationship.
For example, a significant discovery by Ruscio and associates showed that 19% of individuals diagnosed with OCD had previously displayed signs of attention deficit hyperactivity disorder. Furthermore, around 75% of people identified with attention deficit hyperactivity disorder are categorized as having the impulsive/hyperactive (combined) type, which can complicate the handling of OCD manifestations. Children diagnosed with attention deficit hyperactivity disorder may experience heightened impulsivity, potentially exacerbating compulsive behaviors associated with OCD, making it crucial to understand how to add ADHD OCD and how these conditions interact.
Lamis Ibrahim highlights the necessity for greater awareness concerning childhood attention disorders in psychiatric clinical practice, proposing that tackling these issues is crucial for effective oversight. Furthermore, research indicates that 44% of OCD patients report having experienced attention deficit hyperactivity disorder symptoms during childhood, further supporting the importance of recognizing this relationship. This connection emphasizes the necessity to add ADHD OCD considerations into customized treatment strategies for obsessive-compulsive disorder care.
Moreover, the variability in male-to-female ratios across studies can confound findings on ADHD-OCD co-occurrence, highlighting the need for careful consideration of exclusion criteria in research. A case study titled "Impact of Exclusion Criteria on ADHD-OCD Studies" revealed that varying exclusion criteria can significantly affect the reported prevalence rates of attention deficit hyperactivity disorder and obsessive-compulsive disorder, particularly when excluding conditions like tic disorders. This reinforces the necessity for researchers to transparently report their criteria to enhance the generalizability of their findings.
Comprehending the interaction between attention deficit hyperactivity disorder and obsessive-compulsive disorder is crucial for creating a customized strategy for treatment and daily care, ultimately enhancing the quality of life for individuals impacted by both disorders.
Recognizing Symptoms: Identifying ADHD and OCD in Daily Life
Attention-Deficit/Hyperactivity Disorder is marked by a variety of signs, including trouble focusing on tasks, excessive fidgeting, and hasty decision-making. In contrast, Obsessive-Compulsive Disorder (OCD) often presents through behaviors such as repetitive hand-washing, compulsive checking, or intrusive thoughts that lead to significant anxiety. Understanding how to add ADHD OCD signs may coexist in daily life is critical for effective management.
For instance, a child exhibiting signs of add adhd ocd might frequently interrupt conversations, a hallmark of attention deficit hyperactivity disorder, while simultaneously feeling an overwhelming urge to check that the door is locked multiple times, indicative of OCD. Notably, studies indicate that a history of ADD ADHD OCD symptoms in childhood can result in heightened impulsiveness and more severe OCD manifestations. In fact, OCD is the world’s fourth most common psychiatric disorder, with a lifetime prevalence of 2–3%.
As Mossner observed, 'This gene, based on a meta-analysis by Gizer et al., demonstrated a significant correlation with attention deficit hyperactivity disorder, while it did not associate with OCD after meta-analysis.' This highlights the complex relationship that can be observed when we add ADHD OCD to the discussion of attention deficit hyperactivity disorder and OCD. Furthermore, findings from recent case studies on synaptic genes in attention deficit hyperactivity disorder suggest that synaptic dysfunction may contribute to the pathophysiology of this condition, warranting further investigation.
Maintaining a symptom diary can be an invaluable tool, allowing parents and caregivers to document behaviors and identify triggers. This practice not only promotes greater awareness but also helps in creating customized management strategies to tackle the unique challenges encountered by individuals who add adhd ocd.
Therapeutic Approaches: Effective Treatments for ADHD and OCD
Effectively treating ADD, ADHD, and OCD requires a comprehensive strategy that includes:
- Behavioral therapy
- Medication—such as stimulants
- Parent training programs
For individuals with OCD, Cognitive Behavioral Therapy (CBT) and exposure and response prevention are widely regarded as primary interventions. Research indicates that combining behavioral interventions tailored for attention deficit hyperactivity disorder with CBT techniques specifically aimed at OCD can add ADHD OCD and yield enhanced outcomes.
For instance, the Parent IRS, which consists of 7 items assessing various domains of adolescent functioning, can provide a quantitative measure of the treatment's impact. A recent randomized controlled trial compared metacognitive therapy to supportive therapy for adults with attention deficit hyperactivity disorder, focusing on inattentive behaviors. The metacognitive therapy group showed significantly greater reductions in inattentive symptoms, indicating its effectiveness over supportive therapy.
Laura E. Knouse noted, "Some of the investigator time for preparation of this paper was supported by NIH Grant 5R01MH69812 to Steven A. Safren and by the Kaplen Fellowship on Depression from Harvard Medical School to Laura E. Knouse," emphasizing the importance of research in this area.
It is essential to collaborate with healthcare professionals to develop a personalized treatment plan that can add ADHD OCD and addresses both conditions holistically. Regular follow-ups, including assessments of emotional distress and quality of life, are critical to adapting the treatment as needs evolve, ensuring sustained effectiveness and improvement in overall well-being.
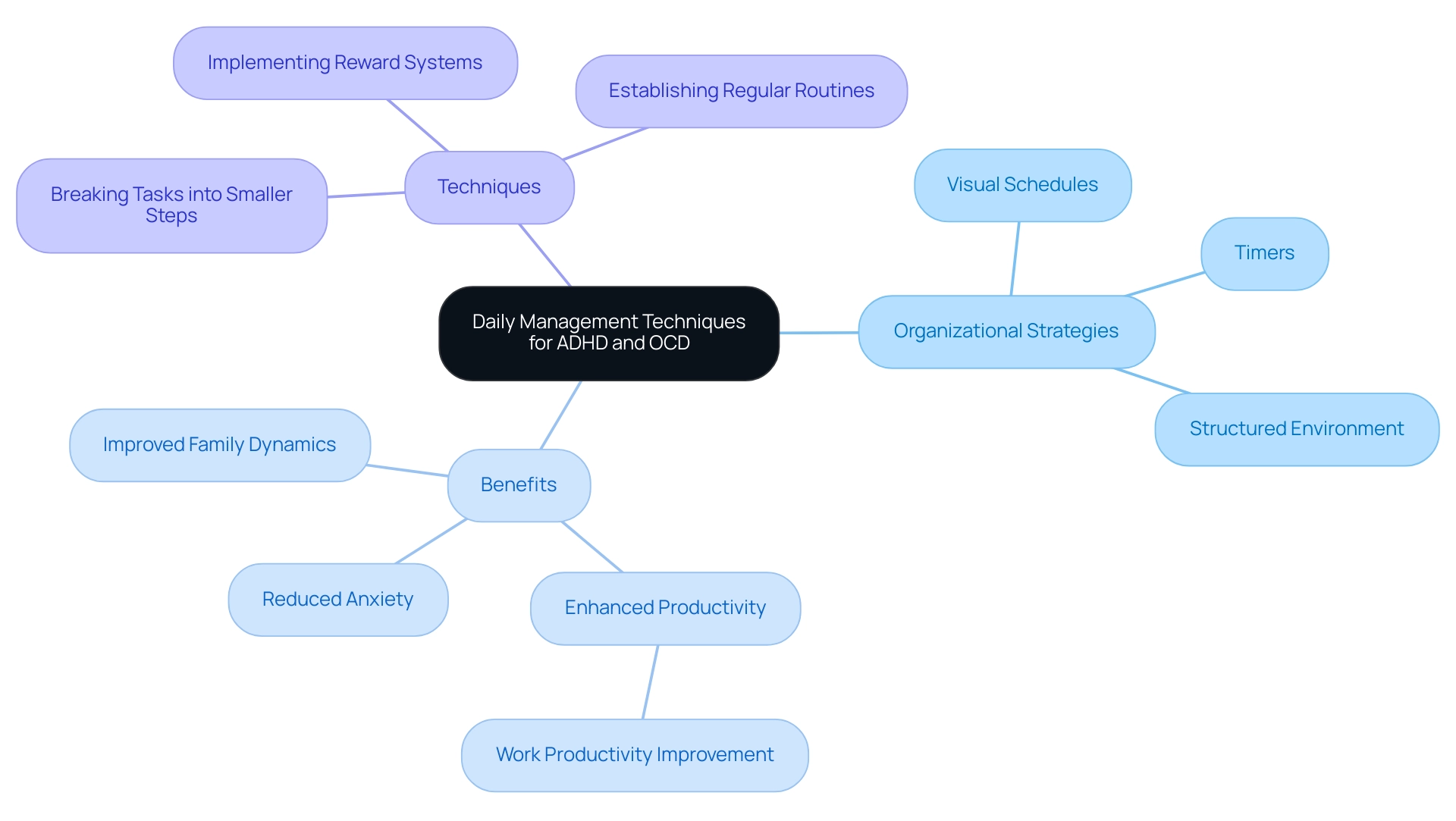
Daily Management Techniques: Integrating ADHD and OCD Strategies
Incorporating effective organizational strategies into daily practices can help to add ADHD and OCD coping advantages for individuals. Utilizing visual schedules, for instance, not only helps children maintain organization and focus but also reduces anxiety and meltdowns, as noted by Tricia:
The predictability and structure provided by visual schedules help to reduce anxiety and meltdowns while promoting independence and self-regulation.
Furthermore, research indicates that work productivity during testing for individuals with attention deficit hyperactivity disorder and obsessive-compulsive disorder was significantly enhanced (F(1, 32) = 14.785, p = .001), underscoring the effectiveness of organized supervision techniques in improving overall results.
Timers can further enhance time organization and facilitate task completion, making them a practical tool in daily operations. Creating a structured environment with clear expectations can alleviate anxiety for those with OCD, promoting a sense of stability. Insights from the case study titled 'Family Functioning and Mental Health' reveal that while attention deficit hyperactivity disorder may strain family relationships, the effect of obsessive-compulsive disorder on family dynamics is less direct, emphasizing the importance of personalized treatment strategies.
Additionally, strategies such as breaking tasks into smaller, manageable steps and implementing reward systems for completed tasks can encourage positive behavior. Establishing regular routines for meals, homework, and relaxation not only supports daily stability but also minimizes stress, demonstrating how a well-structured approach can effectively add ADHD OCD to address the unique challenges. As one therapist highlights,
Daily strategies that incorporate visual schedules and routine can significantly enhance the quality of life for children with attention deficit hyperactivity disorder and obsessive-compulsive disorder, fostering independence and reducing family stress.
Building a Support Network: Connecting with Others for Better Management
Engaging with others who comprehend the intricacies of add adhd ocd can significantly improve the management experience for families. Joining local support groups, online forums, or community organizations dedicated to these conditions offers invaluable opportunities for sharing insights and strategies. Research indicates that children with attention deficit hyperactivity disorder, particularly males who constitute 62% of the samples, often face additional co-occurring conditions and benefit from the collective experiences of others, especially when navigating severe symptoms.
As observed in recent findings, children with both attention deficit hyperactivity disorder and another co-occurring condition, such as anxiety or depression, more frequently experienced severe attention deficit hyperactivity disorder than those without additional conditions. Engaging with fellow parents can illuminate effective resources and provide emotional support that is critical during challenging times. Collaborating with professionals, including therapists and educators, further enriches the management plan for your child.
As one support group leader noted, 'The strength of our community lies in shared experiences; they empower families to tackle their unique challenges together.' Additionally, it is important to recognize that children with Medicaid are less likely to receive care for attention deficit hyperactivity disorder from specialists compared to those with private insurance, highlighting the role of support networks in accessing appropriate care. The effect of community support on handling attention deficit hyperactivity disorder and OCD, particularly when we add ADHD OCD strategies, cannot be understated, as it fosters resilience and encourages proactive approaches to treatment.
To find support networks, consider reaching out to local mental health organizations or searching for online platforms that cater to discussions related to attention disorders and obsessive-compulsive behaviors. By building a robust support system, parents can more effectively navigate their child's journey and promote their overall well-being.

Mindfulness and Self-Care: Enhancing Daily Management of ADHD and OCD
Mindfulness practices—such as meditation, deep breathing exercises, and yoga—play a crucial role in supporting individuals who add ADHD OCD. These techniques promote relaxation and improve focus, which can be especially helpful in managing issues. Setting aside even a few minutes each day for mindfulness activities can lead to significant improvements in emotional well-being.
In fact, a review identified 112 relevant articles, with 10 selected for inclusion, highlighting the growing body of evidence supporting these practices. Furthermore, self-care should not be overlooked; regular physical activity, balanced nutrition, and adequate sleep are essential components of a holistic approach to managing these conditions. Creating a calming home environment, complete with quiet spaces for relaxation, can further promote mental health.
Recent studies suggest that such self-care strategies, when incorporated into daily routines, not only enhance management of issues but also contribute to overall mental wellness. As highlighted by Olivia Guy-Evans, "mindfulness can be a transformative tool," emphasizing the significance of embracing these practices to manage the challenges of add ADHD OCD effectively. Additionally, case studies have shown that clients who engage in mindfulness-based interventions report better treatment outcomes, experiencing greater symptom reduction and perceiving their treatment as more effective compared to those who do not.
This evidence supports the notion that mindfulness practices can significantly enhance the quality of life for individuals who add ADHD and OCD.
Conclusion
The intricate interplay between ADHD and OCD underscores the necessity for a comprehensive understanding of both disorders. Recognizing the distinct symptoms of ADHD, such as inattention and impulsivity, alongside the compulsive behaviors and intrusive thoughts characteristic of OCD, is fundamental for effective management. The co-occurrence of these conditions highlights the need for tailored treatment approaches that address the unique challenges faced by individuals and their families.
Effective therapeutic strategies, including:
- Behavioral therapy
- Medication
- Mindfulness practices
play a crucial role in managing symptoms. Integrating daily management techniques, such as visual schedules and structured routines, can significantly enhance the quality of life for those dealing with both ADHD and OCD. Furthermore, building a robust support network fosters resilience and provides essential emotional backing, empowering families to navigate the complexities of these disorders together.
Ultimately, the journey towards better management of ADHD and OCD requires ongoing awareness, personalized strategies, and the incorporation of supportive community resources. By recognizing the connections between these two conditions and implementing effective management techniques, individuals can improve their overall well-being and lead fulfilling lives. Emphasizing the importance of tailored treatment and community support can pave the way for a brighter future for those affected by ADHD and OCD.
Frequently Asked Questions
What are the main characteristics of Attention-Deficit/Hyperactivity Disorder (ADHD) and Obsessive-Compulsive Disorder (OCD)?
ADHD is characterized by signs such as inattention, hyperactivity, and impulsivity. In contrast, OCD presents through unwanted intrusive thoughts (obsessions) and repetitive actions (compulsions).
How common is the co-occurrence of ADHD and OCD?
The co-occurrence rates of ADHD and OCD can vary significantly, ranging from 0% to 60% across different studies.
What percentage of individuals with OCD have shown signs of ADHD?
Research indicates that 19% of individuals diagnosed with OCD had previously displayed signs of ADHD.
How does ADHD affect the manifestation of OCD symptoms?
Children with ADHD may experience heightened impulsivity, which can exacerbate compulsive behaviors associated with OCD.
What is the significance of recognizing the relationship between ADHD and OCD in treatment?
Understanding the interaction between ADHD and OCD is crucial for developing customized treatment strategies, which can enhance the quality of life for those affected by both disorders.
What percentage of OCD patients report having experienced ADHD symptoms during childhood?
Approximately 44% of OCD patients report having experienced ADHD symptoms during their childhood.
How can exclusion criteria in research impact findings on ADHD and OCD co-occurrence?
Variability in male-to-female ratios and differing exclusion criteria can confound findings, affecting the reported prevalence rates of ADHD and OCD.
What role does maintaining a symptom diary play in managing ADHD and OCD?
A symptom diary can help parents and caregivers document behaviors and identify triggers, promoting greater awareness and aiding in the development of customized management strategies.
What is the importance of further research into the genetic factors associated with ADHD and OCD?
Understanding the complex relationship between genetic factors and these disorders may provide insights into their pathophysiology and inform treatment approaches.




