Introduction
Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) is a complex condition that falls within the autism spectrum. While it may not fully meet the diagnostic criteria for other Autism Spectrum Disorders, it presents unique challenges in social interactions, communication abilities, and behavior patterns. This article explores the historical context, signs and symptoms, diagnosis criteria, subgroups and variability, treatment and intervention strategies, impact on daily functioning, comparison with other pervasive developmental disorders, challenges, and future directions.
By shedding light on the diverse experiences and needs of individuals with PDD-NOS, this article aims to provide guidance and resources to empower Parent Advocates in supporting their children's well-being.
Historical Context and Definition
Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) was once a separate category under autism spectrum disorders (ASDs), reflecting a variant of autism with subtler manifestations. It has evolved with the updated classification in DSM-5 to be encompassed in the broader diagnosis of Autism Spectrum Disorder – Level 1. This change reflects a more nuanced understanding of autism, recognizing that varying levels of social and communication challenges, as well as repetitive behaviors, can manifest even if they don't fit the conventional diagnosis criteria.
Lifelong impacts of such developmental disorders are evident in cases like Jordan's, a 54-year-old with developmental disabilities who has navigated life's upheavals with resilience. Jordan's experiences underscore the spectrum nature of autism, embodying the fact that while challenges exist, individuals with ASD can engage in and enjoy activities like sports and leisure, contributing to their social and emotional well-being.
Signs and Symptoms
Individuals with Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS) display a cluster of behaviors that can significantly affect their social interactions, communication abilities, and behavior patterns. One of the primary challenges they face is in the realm of social interaction, wherein they may struggle with grasping social norms and cues, leading to difficulties in forming and maintaining relationships and a tendency to avoid making eye contact. Communication hurdles often present through a delay in the development of speech and language skills, alongside atypical speech patterns such as echolalia.
Additionally, these individuals might find it hard to understand and convey nonverbal communication effectively.
Another characteristic sign of PDD-NOS is the display of restricted and repetitive behaviors. This can manifest as repetitive physical movements, such as rocking or hand-flapping, or an intense and exclusive focus on specific interests or routines. These behaviors are not just habits but are integral to their sense of order and predictability.
Moreover, experts note the nuanced presentation of these symptoms, emphasizing that no two cases are identical, hence the diagnosis and approach to care must be individualized. Physicians employ psychiatric diagnostic criteria to evaluate and diagnose personality disorders, such as PDD-NOS, which often necessitates a thorough understanding of the person's behavioral patterns and the distress or impairment they engender. While medications can alleviate some symptoms, it is the tailored psychotherapeutic interventions that equip individuals with the tools to navigate their personal and interpersonal challenges more effectively.
With advancing research and richer insights gleaned from healthcare professionals' interactions with patient advocacy groups, there is an ever-growing understanding and recognition of conditions like PDD-NOS, empowering affected individuals and their families to seek the support they need.
Diagnosis and Diagnostic Criteria
Diagnosing any neuropsychiatric disorder meticulously follows established criteria to ensure accuracy and tailor appropriate interventions. When it comes to Pervasive Developmental Disorder - Not Otherwise Specified (PDD-NOS), professionals rely on the criteria stated in the DSM-5. This condition is characterized by significant challenges in social communication and interaction, coupled with the presence of restrictive and repetitive behaviors.
However, the manifestation does not satisfy the complete diagnostic requirements for other Autism Spectrum Disorders (ASD).
PDD-NOS is not a diagnosis to be taken lightly or made in haste. It requires a comprehensive evaluation by a healthcare professional adept in psychiatric disorders, such as a psychiatrist or psychologist. This extensive assessment includes considering the individual’s developmental level and age, which influence the presentation of symptoms and consequent diagnostic criteria.
A parallel can be drawn to recent studies, such as the case of a 57-year-old woman presenting with upper motor neuron signs along with parkinsonian symptoms, leading to a diagnosis of primary lateral sclerosis plus parkinsonism. The diagnostic process exemplified the need for a period of observation and thorough investigation before arriving at a conclusive diagnosis. This rigorous approach ensures that while some diagnostic standards, like the Pringle criteria, necessitate a pure presentation of symptoms for years, clinicians remain vigilant to the possibility of variations in symptomatology, as evidenced in PDD-NOS assessments.
These cases underscore the necessity for precise diagnosis guided by strict criteria, which is not only a cornerstone of individualized patient care but is also crucial for informing research and development strategies. Clinicians must be attuned to the nuances of each diagnosis, often requiring them to remain flexible in their approach and open to evolving information, ultimately enhancing the support to both individuals with the condition and the broader patient advocacy community.
Subgroups and Variability
People with Pervasive Developmental Disorders-Not Otherwise Specified (PDD-NOS) are a diverse group, each with unique abilities and hurdles to overcome. Unlike classic autism, which has a well-defined set of symptoms, individuals with PDD-NOS might display a wide array of social, communication, and behavioral challenges, albeit not fitting all the typical autism criteria. This spectrum includes those who are socially awkward but manage well in academic environments, to those with significant challenges in daily functioning.
Addressing the individual needs of persons with PDD-NOS is paramount, crafting support strategies that emphasize their personal aptitudes while mitigating the areas they find challenging. Psychiatrists using criteria from the DSM-5-TR may find differing personality traits underlining their behavior, with an emphasis on understanding each personality's impact on their self-perception and interactions with others. By prioritizing a tailored approach to treatment and intervention, rather than a one-size-fits-all mentality, patients and specialists alike can navigate these complexities better, improving quality of life.
Treatment and Intervention Strategies
Managing PDD-NOS encompasses various intervention strategies to aid individuals in leading rewarding lives despite the absence of a specific cure. It is widely recognized that early intervention plays a pivotal role in this endeavor. The interventions may comprise speech and language therapy, which targets communication deficits, and occupational therapy, which focuses on improving daily functioning.
Social skills training is particularly beneficial for enhancing interactions with others, a challenge commonly faced by individuals with PDD-NOS.
One of the notable therapies utilized is Applied Behavior Analysis (ABA), which employs positive reinforcement to cultivate new skills and mitigate challenging behaviors. Through individualized education plans (IEPs), tailored strategies are provided to meet each person's needs. Specialized educational settings further support these individuals by offering necessary accommodations.
These combined efforts help in fostering a supportive environment that enables individuals with PDD-NOS to thrive.
Impact on Daily Functioning
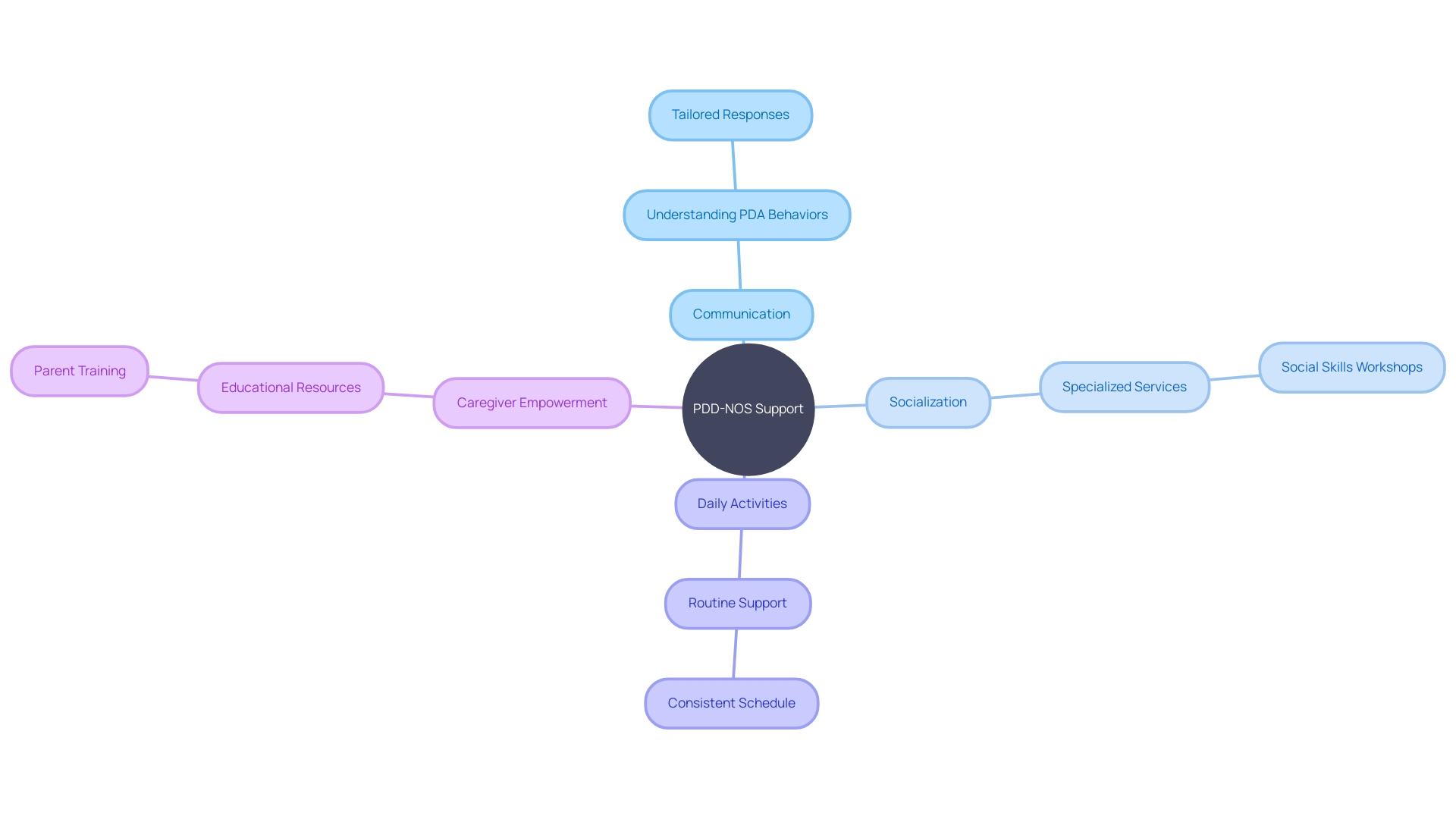
Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) can present complex challenges in communication, socialization, and daily activities for those diagnosed with it. To navigate these challenges, individuals with PDD-NOS often require tailored support and accommodations. This support is not just critical for their well-being but can be transformative in developing necessary life skills.
By drawing on the collective insights from educational interventions for children with ADHD, we understand that negative experiences can accumulate over time. This cumulative effect makes it crucial to provide consistent and everyday support, not just formal interventions like IEPs. For instance, caregivers and teachers who work closely with children with ADHD witness the positive impact routine support can have, improving the child's ability to engage more fully with their education and peer relationships.
Legal frameworks, like the Creative Commons license—which facilitates the sharing and adaptation of resources—emphasize the importance of accessible interventions. This is particularly relevant for PDD-NOS, where understanding and addressing the unique demands of the condition are essential. Notably, anecdotal evidence, such as the experience of Fabio Dwyer, sheds light on the profound personal and professional impact that neurological challenges can have on individuals.
Similarly, initiatives like 'Connecting Communities to Caring-Based Dementia-Specific Services and Supports' highlight the beneficial effects of linking individuals with disabilities and their families to specialized support.
Moreover, research into Pathological Demand Avoidance (PDA), a profile associated with the autism spectrum, reveals that everyday demands can trigger intense anxiety in individuals, leading to extreme avoidance. This avoidance is a coping mechanism to maintain a sense of control and protect one's autonomy. Key traits include resistance to routine tasks, which echoes similar obstacles faced by those with PDD-NOS.
Consequently, understanding these behaviors can inform tailored support strategies that resonate with the individual's need for independence while also encouraging engagement with their environment.
Lastly, acknowledging the caregivers' role, as seen in dementia care, is equally applicable to those supporting individuals with PDD-NOS. Informal caregivers often face financial strain, mental health challenges, and physical exhaustion, but they also report positive experiences like feelings of reciprocity and spiritual well-being. The COVID-19 pandemic has intensified these challenges, emphasizing the need for a robust support network.
Supporting those with PDD-NOS thus involves not only direct interventions but also empowering those in caregiving roles, underscoring the interconnectedness of individual support systems and overall life quality enhancement.
Comparison with Other Pervasive Developmental Disorders
Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) represents a category within the autism spectrum where individuals demonstrate certain autistic traits, but not to the extent that fully satisfies an Autism or Asperger's Syndrome diagnosis. These individuals often present a mosaic of characteristics, which results in unique profiles that necessitate tailored intervention strategies. The condition aligns with the notion of neurodiversity, valuing different brain wiring that do not align strictly with a 'neurotypical' or standard neurocognitive pattern.
This perspective celebrates individual variance and contends that approaches to neurological conditions should not be one-size-fits-all. The inception of PDD-NOS as a diagnosis highlights the importance of nuanced understanding of the autism spectrum and the diversity within it.
Challenges and Future Directions
While we've made strides in recognizing and diagnosing Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), there's still a long journey ahead. Access to vital services, such as early intervention, specialized education, and consistent therapies, remains scarce for many dealing with PDD-NOS, causing detrimental delays in care. With stories like Jordan's, who lived through profound loss and faced hospitalization due to the lack of suitable support, it becomes increasingly clear that more research is necessary to delve into the causes of PDD-NOS and craft effective, individualized interventions.
Recent news highlights initiatives paving the way, such as research funded by organizations that prioritize the views of those affected by neurological conditions. A heartening example is the alignment of research funding with community priorities, focusing on understanding the evolution of conditions like Parkinson's. Additionally, technology's role in overcoming barriers to care is gaining recognition, urging a reassessment of its compatibility across various access points, considering individuals' technological familiarity and the security of these platforms.
Empowering narratives, like the one shared by Kelley Coleman in her upcoming book, offer guidance to families navigating the complex networks of support required for loved ones with disabilities. Amidst this, alarming statistics remind us of the urgent need for action: the COVID-19 pandemic alone has left over 265,000 children without a parent or caregiver, with long-lasting repercussions, particularly on communities of color and low-income families. In this context, it's vital to recognize the power of advocacy, community engagement, and the mutual sharing of experiences to overcome current hurdles and create an inclusive environment where individuals like Jordan can thrive without fear of being left behind.
Conclusion
In conclusion, PDD-NOS is a complex condition within the autism spectrum that presents challenges in social interactions, communication abilities, and behavior patterns. Accurate diagnosis and tailored interventions are crucial in supporting individuals with PDD-NOS.
Early intervention, speech and language therapy, occupational therapy, and social skills training play vital roles in managing PDD-NOS. The individualized approach, including Applied Behavior Analysis (ABA) and individualized education plans (IEPs), helps cultivate new skills and mitigate challenging behaviors.
Recognizing the unique needs of individuals with PDD-NOS is paramount. The diversity within PDD-NOS profiles necessitates tailored support strategies that emphasize personal strengths while addressing areas of difficulty. Embracing the neurodiversity perspective promotes inclusivity and individualized care.
Improving access to support services for individuals with PDD-NOS is a priority. Further research is needed to better understand the causes of PDD-NOS and develop effective interventions. Advocacy, community engagement, and sharing experiences are crucial in overcoming existing challenges and creating an inclusive environment.
By providing individualized support, we can empower individuals with PDD-NOS to lead fulfilling lives. Collaboration, research, advocacy, and community engagement are essential in overcoming barriers and enhancing outcomes for individuals with PDD-NOS. Together, we can create a more inclusive society that allows individuals with PDD-NOS to thrive and reach their full potential.




