Introduction
Tracing the evolution of the Diagnostic and Statistical Manual of Mental Disorders (DSM) reveals a complex history, marked by significant shifts in the understanding of mental health and the influence of external factors on psychiatric diagnosis. From financial conflicts of interest to the ongoing efforts to address privacy concerns, the DSM-5 has had a profound impact on the field of mental health. Understanding the history, organization, and key components of the DSM-5 is crucial for healthcare professionals and researchers alike.
In this article, we will explore the history and evolution of the DSM-5, its organization and structure, the key components of diagnostic criteria and codes, the role of specifiers and diagnostic features, cultural and gender considerations, and the practical applications and limitations of the DSM-5. We will also delve into the commonly diagnosed mental disorders and revisions in the DSM-5-TR, as well as future developments and updates in the field of mental health diagnostics. Join us as we navigate the intricacies of the DSM-5 and its impact on the well-being of millions.
History and Evolution of DSM-5
Tracing the evolution of the Diagnostic and Statistical Manual of Mental Disorders (DSM) reveals a complex history, marked by significant shifts in the understanding of mental health and the influence of external factors on psychiatric diagnosis. The transition from the previous edition of the diagnostic manual to the current one was not just an academic process; it was closely connected with matters like financial conflicts of interest. Studies have highlighted the concerning links between the pharmaceutical industry and the panel members responsible for crafting the DSM's diagnostic criteria, particularly in areas where medication is the primary treatment.
In response to these findings, the American Psychiatric Association, the body overseeing the DSM, instituted a conflict of interest policy in 2007. Yet, follow-up research conducted in 2012, on the eve of the DSM-5 release, demonstrated that financial entanglements persisted, with a majority of panel members still having ties to the pharmaceutical industry. This was especially prevalent in panels dealing with disorders treated pharmacologically.
The historical perspective of psychiatry is crucial for understanding these developments, offering insights into the varied approaches to psychological illness over time. Medical education often lacks this historical context, focusing instead on current models and facts, sometimes at the expense of appreciating the nuances and uncertainties that have shaped the field. Comprehending the past of psychological well-being categorization can enlighten existing debates and steer forthcoming enhancements in the area. Moreover, engaging with this history can enrich the path of medical students pursuing psychiatry, providing a more rounded and critical view of the profession.
Recent updates from the American Psychiatric Association, including changes to their privacy policy and terms of use, reflect an ongoing effort to address privacy concerns, particularly for individuals in the European Economic Area. These efforts are part of a broader attempt to maintain trust and integrity within the field.
The importance of this historical understanding is underscored by the continuous prevalence of mental health issues and the need for accurate diagnosis and effective treatment. For instance, the recommendation by the United States Preventive Services Task Force to screen for anxiety from childhood through adulthood, including during pregnancy and postpartum periods, is based on systematic reviews confirming the accuracy of screening tools and the benefits of treatment.
Organization and Structure of DSM-5
Leading experts through the intricacies of psychiatric diagnosis, the structure of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, is meticulously organized. It features a systematic layout that includes various sections, categories, and subcategories, each designed to enhance the precision of diagnosis. The manual's framework is not only user-friendly but also rigorously informed by current research, ensuring that those utilizing it can effectively navigate its criteria. For instance, the importance of evaluating the validity and reliability of diagnoses is emphasized, underscoring the manual's commitment to evidence-based practice.
The organization of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders reflects its dual function as both a clinical tool and a research reference. It is designed to facilitate an understanding of psychological disorders based on symptoms and behaviors, which is essential for accurate identification and treatment. Hence, a clear comprehension of its layout is fundamental for healthcare providers and researchers alike.
Considering the latest advancements in the industry, such as the implementation of state-of-the-art screening and monitoring technologies by companies like Darmiyan and BrainSee, the significance of the diagnostic manual remains in flux. These advancements emphasize the continuous requirement for accuracy in diagnostics related to the mind, which the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders aims to assist.
Moreover, the credibility of the manual is maintained through strict conflict of interest guidelines established by the American Psychiatric Association. Despite concerns highlighted in studies regarding financial ties influencing previous editions of the DSM, efforts have been made to enhance transparency and reduce potential biases in the latest edition.
As we struggle with the societal impact of psychological well-being, statistics from the National Institute of Mental Health (NIMH) provide a sobering reminder of the prevalence of emotional affliction and the imperative for reliable diagnostic tools. With almost 20% of adults in the United States living with a condition related to the mind, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders continues to be an essential tool in confronting these difficulties and promoting the welfare of millions.
Key Components of DSM-5
The criteria from the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders play a crucial role in diagnosing and comprehending mental health conditions. This structured guideline includes diagnostic criteria that outline symptoms and behaviors, diagnostic codes that facilitate the identification and classification of disorders, specifiers that detail particular disorder characteristics, and diagnostic features that offer an in-depth look at clinical presentations. To ensure the DSM-5's relevance and accuracy, a study titled 'Reconstructing Psychopathology' took a data-driven approach to reorganize symptoms in the DSM-5, highlighting the importance of a quantitative structure in psychiatric classification.
For instance, the study, which is part of the development of the Hierarchical Taxonomy of Psychopathology (HiTOP), analyzed responses from a diverse sample of 14.8K participants. This research underscores the dynamic nature of psychopathology and the need for continuous evaluation of diagnostic tools. Moreover, the acknowledgment of Group Psychology and Group Psychotherapy as a formal specialty by the American Psychological Association in 2018 emphasizes the changing landscape of psychological treatment and diagnosis.
Considering the intricacy of psychological disorders, it is essential to acknowledge that nearly 20 percent of adults in the United States are living with a condition related to their mind, with a substantial portion experiencing severe illnesses of the mind. These statistics not only highlight the prevalence of psychological well-being challenges but also the requirement for strong and precise diagnostic criteria. Therefore, the criteria of the DSM-5 manual and its continuous updates have a crucial role in guiding healthcare professionals in diagnosing and treating conditions of the mind across the nation.
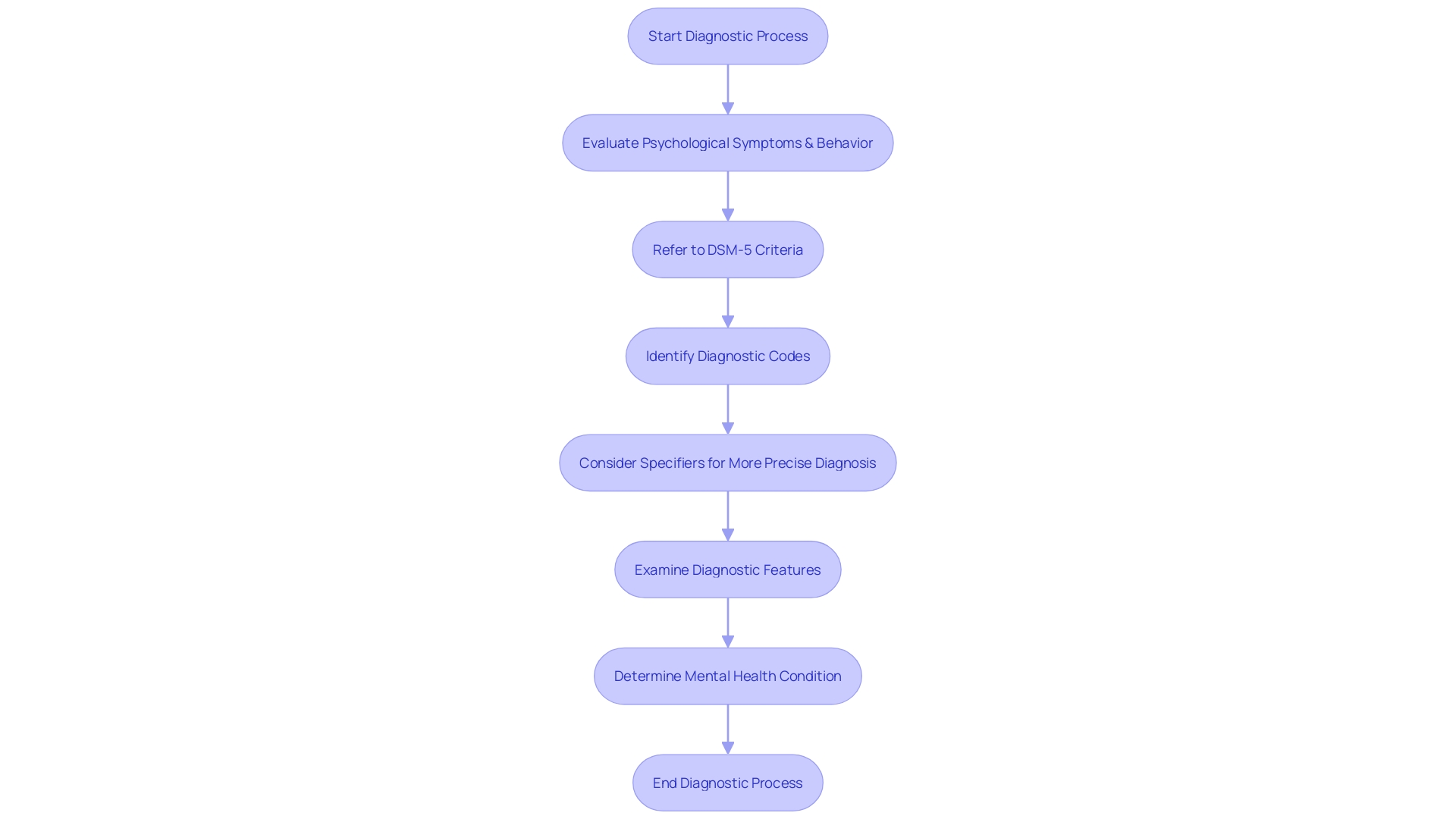
Diagnostic Criteria and Codes
The DSM-5 serves as a critical guide for healthcare professionals, offering a comprehensive system of diagnostic criteria and codes. These components are not only foundational for diagnosis but also pivotal for treatment planning. Let's delve into the intricacies of how these criteria are developed and the significance of diagnostic codes in the diagnostic process.
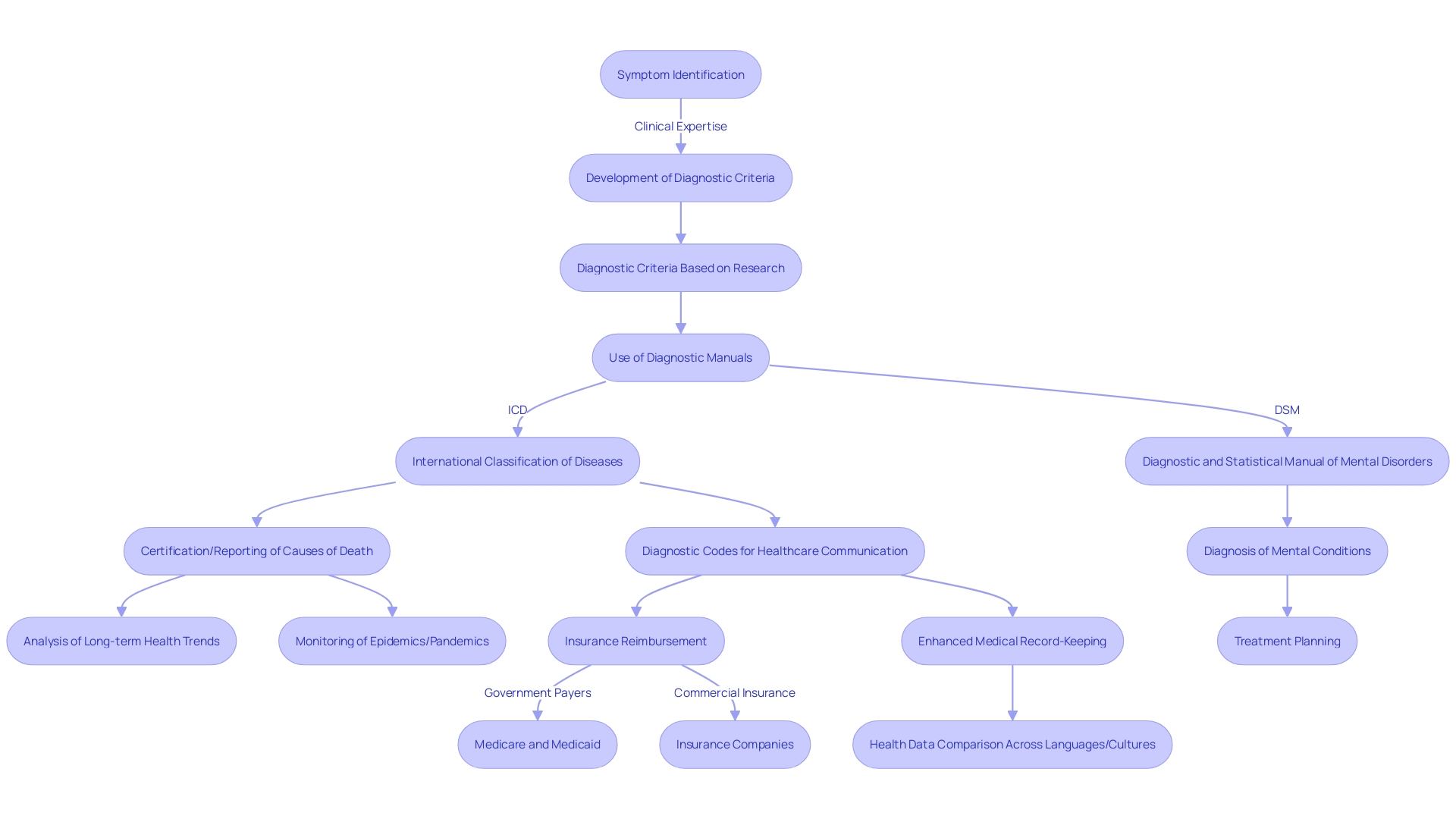
Diagnostic criteria are carefully developed based on rigorous research and clinical expertise, ensuring they accurately encapsulate the symptoms and behaviors associated with specific mental conditions. The recent FDA rule on presenting drug information clearly underscores the importance of understandable language in healthcare communications, a principle that equally applies to the crafting of diagnostic criteria.
Diagnostic codes, meanwhile, are essential for a myriad of reasons. They facilitate clear communication among healthcare providers and are instrumental in the process of insurance reimbursement. For instance, codes are used extensively by government payers like Medicare and Medicaid, as well as commercial insurance companies, to describe healthcare services for reimbursement purposes.
Furthermore, diagnostic codes provide the framework for recording and analyzing epidemiological data, which is crucial for tracking long-term trends and monitoring situations like epidemics or pandemics. They also support morbidity coding and reporting at all levels of healthcare, from primary to tertiary care.
The integration of diagnostic codes into healthcare systems marks a significant advance in medical record-keeping, enabling the compilation and comparison of health data across different languages and cultures. With such a system in place, healthcare professionals and researchers can access up-to-date scientific knowledge, ensuring that patient care is informed by the latest clinical best practices worldwide.
Understanding Specifiers and Diagnostic Features
Understanding the diverse specifiers and diagnostic features outlined in the diagnostic manual can be instrumental in creating a finely-tuned diagnosis. Specifiers are additional labels that clinicians can use to better describe the nuances of an individual's condition beyond the basic diagnosis. As an illustration, the DSM-5 incorporates specifiers for conditions such as ADHD, enabling a more customized treatment plan that takes into account the presence or absence of hyperactivity, impulsivity, or inattention. Diagnostic features, on the other hand, delve deeper into the clinical presentation of a condition, offering insights into the severity and characteristics of symptoms. This not only aids in creating a comprehensive picture of the individual's challenges but also paves the way for more effective intervention strategies. As research continues to evolve, such as the studies approved by the Danish Data Protection Agency, it's clear that ethical considerations remain paramount in the pursuit of understanding and treating neurodevelopmental conditions like autism. Moreover, with the ongoing conversation about compensation strategies in autism and their place in diagnostic settings, there is a growing need to refine these concepts. Discussions among clinicians, researchers, and advocates are vital to shaping a consensus on definitions and support for the spectrum of autism, including profound autism, which is recognized for its distinct needs and outcomes. By embracing these intricate layers of diagnosis, parents and professionals are equipped with the knowledge to support individuals with neurodevelopmental challenges more effectively.
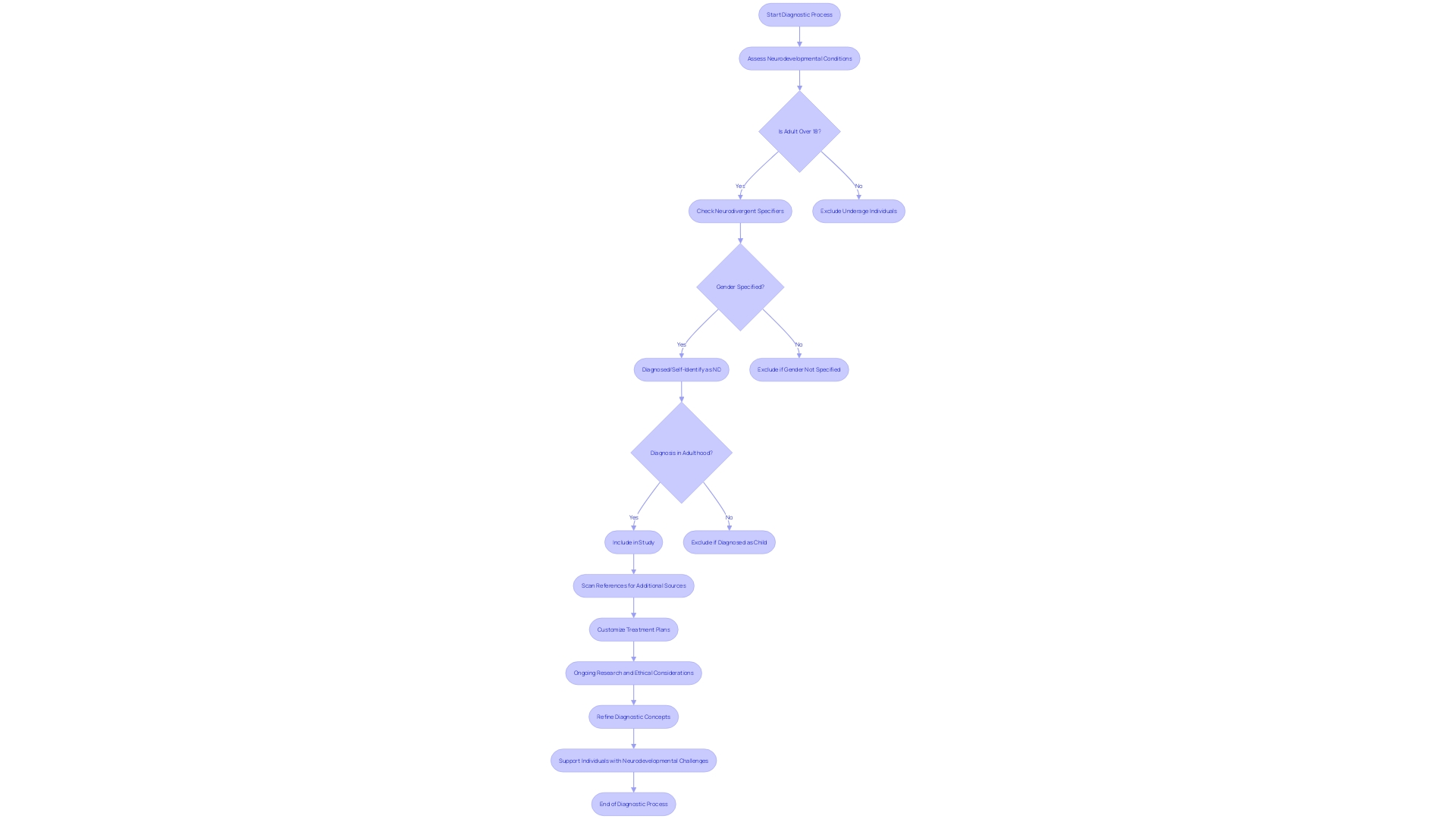
Cultural and Gender Considerations in DSM-5
Autism spectrum disorder (ASD) is marked by a complex interplay of symptoms that can vary significantly across individuals, influenced by factors such as culture and gender. The DSM-5 includes the Cultural Formulation Interview, which guides clinicians in understanding how cultural contexts shape the presentation and recognition of symptoms. For instance, research has pointed out disparities in diagnosis among females, with 80% of autistic females remaining undiagnosed or misdiagnosed by age 18. The consequences of this are profound, as autistic women and non-binary individuals are at greater risk for ill-health compared to their male counterparts. By age 25, 77% of autistic women have been diagnosed with a psychiatric condition, underlining the need for gender-sensitive diagnostic approaches.
Gender diversity also intersects with autism in ways that are only beginning to be understood. While sex is a biological concept with a continuum of traits, gender is a social construct that encompasses a range of identities beyond the male-female binary. Terms like transgender, genderqueer, and agender reflect this spectrum of identities, with transgender individuals often facing unique challenges that can complicate the diagnostic process.
Experts like Sarper Taskiran, a senior child and adolescent psychiatrist, emphasize the importance of considering cultural differences in psychiatric diagnoses. Taskiran's multicultural medical training has shown him the stark contrasts in how psychosis, a condition that can co-occur with autism, is diagnosed and treated across countries. His insights remind us that gender and cultural sensitivity are not merely academic concerns but have tangible consequences on the well-being of individuals.
Statistics reveal that conditions related to the well-being of the mind are widespread, with 19.86 percent of adults in the United States living with a condition pertaining to mental well-being in 2022. These numbers underscore the urgency of adopting inclusive and culturally competent diagnostic practices. By doing so, parents and professionals can better support the diverse needs of individuals on the autism spectrum, ensuring that no one is overlooked due to cultural or gender biases.
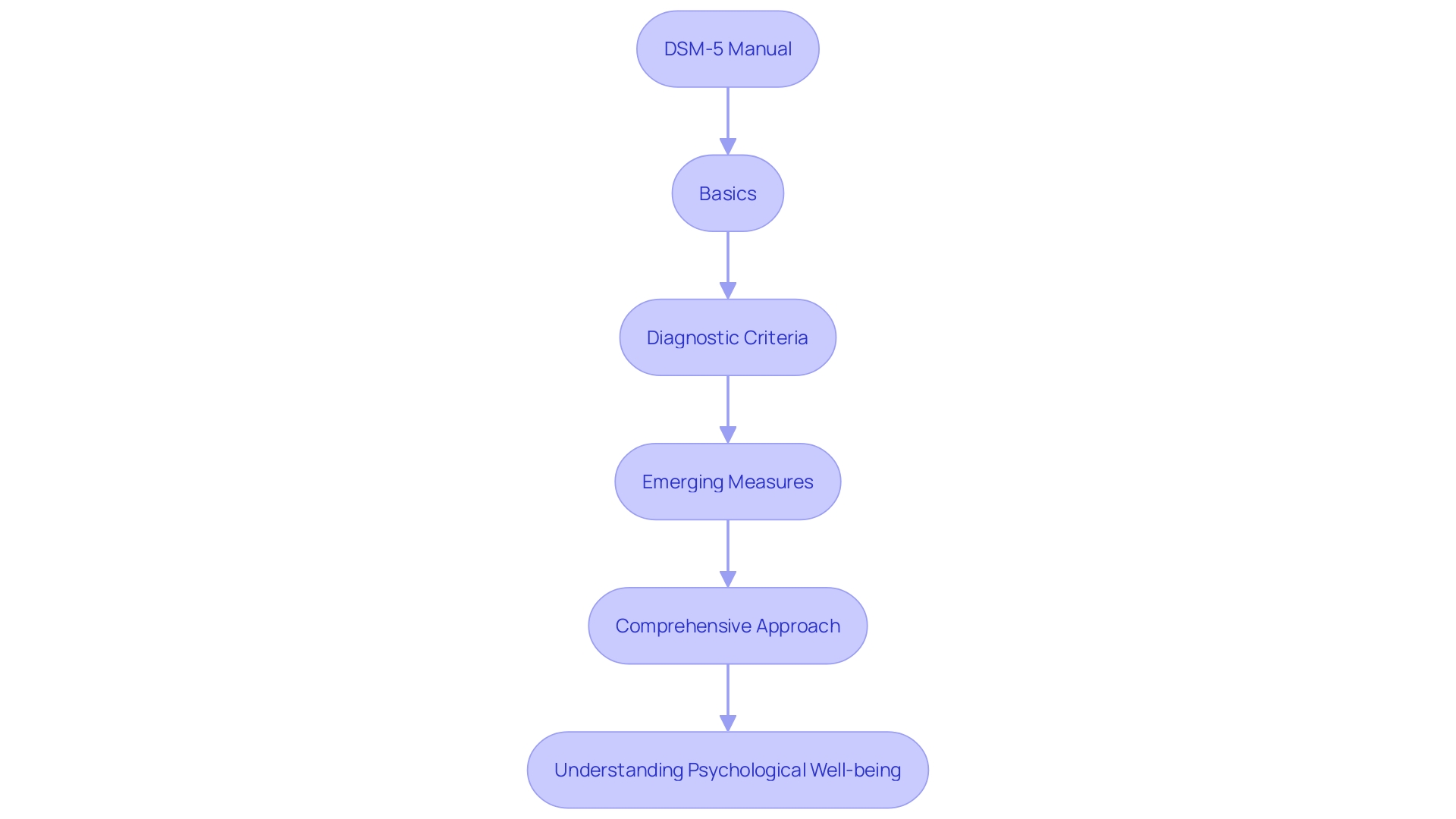
DSM-5 Sections: Basics, Diagnostic Criteria, and Emerging Measures
The DSM-5, an essential instrument in the realm of psychological well-being, is organized into separate sections, each designed to serve a distinct purpose. The first segment we'll explore is the 'Basics' section, which lays the groundwork by defining key terms and concepts. It's a foundational part of the manual that supports a deeper understanding of subsequent content. Next, the 'Diagnostic Criteria' section is the core of the manual, where each psychological disorder is meticulously characterized by specific criteria that clinicians must consider for an accurate diagnosis. This section is informed by extensive research and ongoing debates regarding the validity and reliability of psychiatric diagnosis, reflecting the complexity of categorizing psychological well-being conditions.
Additionally, the 'Emerging Measures' section provides a dynamic space where the latest scales and assessments are presented. These tools are designed to advance the precision of diagnoses and are often accompanied by rigorous data analysis, as shown in the WONDER database reports. This changing area reflects the moving terrain of psychological treatment and the incorporation of new discoveries and approaches, much like the groundbreaking field of psychedelic medicine is questioning conventional paradigms and demonstrating inventive therapeutic alternatives.
Comprehending the content and purpose of each section in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, is crucial for professionals to efficiently navigate the manual, guaranteeing they deliver the highest level of care. The manual's structure reflects the ongoing dialogue in the field, as it must reconcile the traditional medical model with emerging perspectives and societal changes, such as the evolving understanding of gender identity. The DSM-5 is more than a static document; it's a living reflection of current knowledge and societal norms, shaping how we perceive and address psychological well-being.
Commonly Diagnosed Mental Disorders and Revisions in DSM-5-TR
The DSM-5-TR, the most recent update of the Diagnostic and Statistical Manual of Disorders, reflects the developing understanding of cognitive conditions. It serves as a critical tool for both clinicians and researchers in diagnosing and classifying these conditions. The revisions in the DSM-5-TR involve a reassessment of the diagnostic criteria for different conditions, guaranteeing that they correspond with the most recent discoveries in psychological research.
Data shows that around 19.86% of adults in the United States live with a condition related to the mind, and nearly half will encounter one at some stage in their lives. It's also noted that over one in five youth have faced a seriously debilitating condition affecting their mind. These figures underscore the importance of accurate diagnostic criteria, as they guide treatment and support for millions.
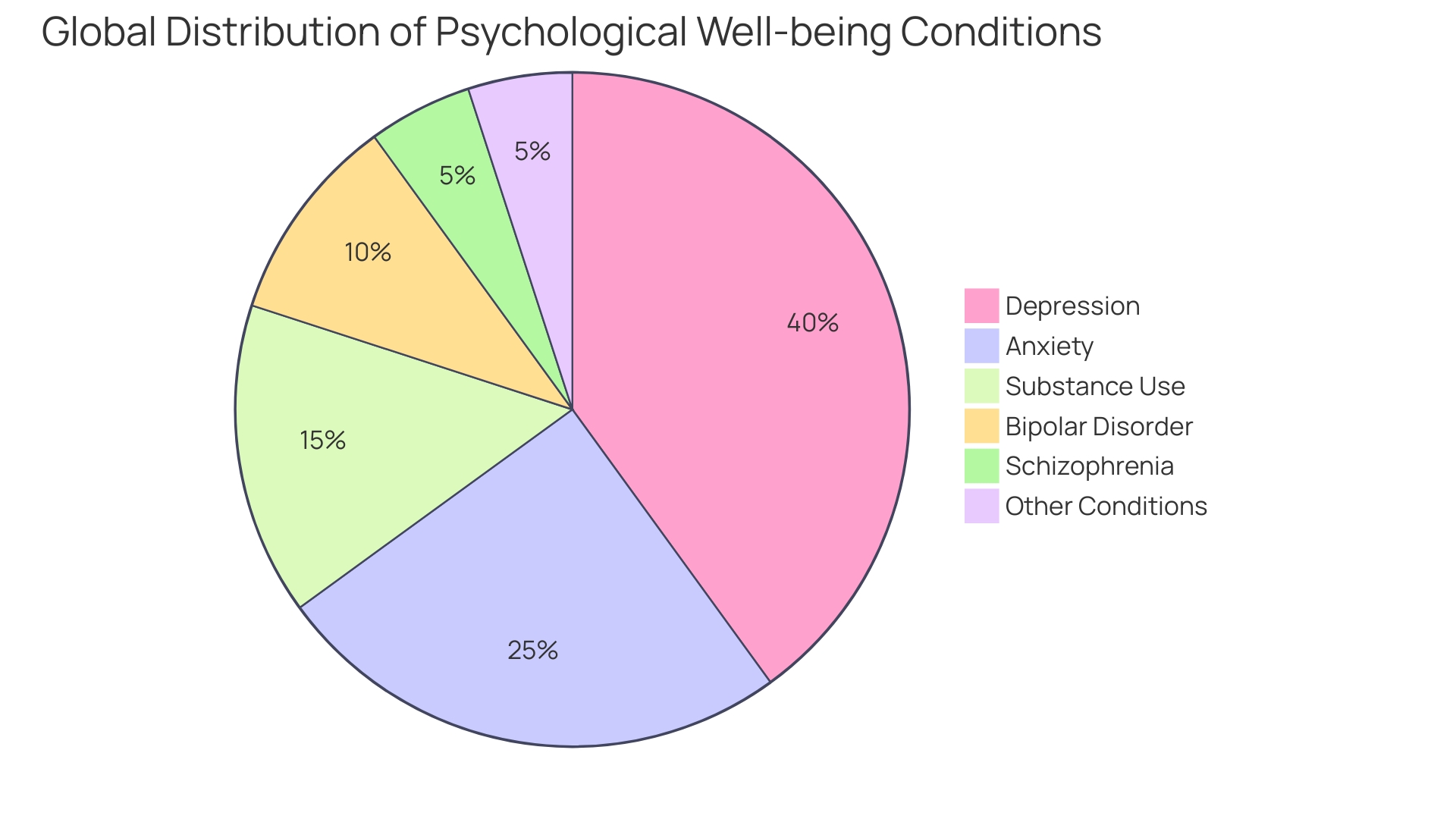
Recent updates, like the new segment on anxiety problems, emphasize the dedication to offering comprehensive guidance in mind well-being. The World Health Organization (WHO) highlights that psychological, neurological, and substance use conditions are important factors in global illness and death. Therefore, the DSM-5-Tr's updates reflect a delicate balance between potential benefits and harms, considering evidence certainty, cost-effectiveness, and resource availability.
The DSM’s evolution over the past 2,000 years has seen a shift from phenomenology to etiology and now to a more inclusive approach, considering the individual's interaction with society. This approach is further supported by the United States Preventive Services Task Force's recent recommendation for anxiety screening in individuals ages 8 to 65, acknowledging the condition's prevalence and the moderate benefits of timely treatment.
Moreover, the DSM-5-TR’s development involved an extensive review of literature by over 200 experts, ensuring the latest edition is informed by nearly a decade of research advancements. This meticulous process reflects the significance of the manual in shaping care for the mind and its profound impact on individuals and families navigating conditions related to their mental well-being.
Practical Applications and Limitations of DSM-5
This manual serves as an essential instrument in the mental health field, crucial for evaluating and diagnosing psychiatric conditions. It provides a common language for clinicians to communicate about their patients' conditions, assisting in treatment planning and guiding research. As mentioned by Burlingame & Strauss (2021), the criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders have greatly contributed to the enhancement of protocols for psychiatric conditions in the evidence-based group treatment literature.
Meta-analyses, like those summarized by Rosendahl et al. (2021), have reinforced the effectiveness of these group treatments. The formal recognition of Group Psychology and Group Psychotherapy as a specialty by the American Psychological Association further emphasizes the influence of the diagnostic and statistical manual in shaping treatment approaches and standards.
However, the manual is not without its challenges. There's an ongoing need to update and refine its content to reflect the latest research, as evidenced by the substantial effort of over 200 experts reviewing literature for the DSM-5-TR update. The history of psychological disorder classification, with its varying emphasis on phenomenology, etiology, and course, speaks to the complexities involved in creating a comprehensive yet practical diagnostic manual.
In terms of legal and societal impact, the criteria of the DSM-5 intersect with definitions of disability under laws such as the Americans with Disabilities Act (ADA). The ADA employs terms like 'cognitive or emotional impairment' and 'major life activities' to define disability—concepts that are also fundamental to understanding the conditions listed in the manual for mental disorders.
While the DSM-5 contributes significantly to the field, it is essential to consult with a medical professional before making any decisions based on its information. The manual is a guide, not a replacement for professional judgment, and should be used as part of a comprehensive approach to emotional well-being that includes clinical expertise and patient values.
Future Developments and Updates
Advancements in psychological well-being diagnostics are crucial for providing effective support to individuals with psychological well-being conditions. The Diagnostic and Statistical Manual of Mental Disorders (DSM), which underwent its latest revision with the DSM-5-TR, is a dynamic document that continues to evolve as new insights and technologies emerge. One area of substantial interest is the incorporation of Artificial Intelligence (AI) into the psychological well-being domain. AI has the potential to enhance diagnostic precision, but it raises important questions regarding the balance between technological reliance and human expertise. Ethical considerations and the risks of false results are challenges that experts, like Rodriguez, emphasize must be carefully navigated.
On the research front, groundbreaking studies like those using Deep Brain Stimulation (DBS) devices to record brain activity during everyday activities, rather than just in controlled laboratory tasks, bring research closer to the natural experiences of individuals with cognitive well-being conditions. This approach has the potential to revolutionize diagnosis and treatment, as seen in studies on disorders like Alzheimer's and severe, treatment-resistant OCD.
The NIMH has a crucial function in offering support and involving stakeholders in research related to psychological well-being, with an annual budget of around $1.8 billion. This dedication supports research that leads to important advancements in care for the mind, such as the initial medication for postpartum depression and screening for the risk of suicide.
Statistical data from NIMH and the World Health Organization (WHO) emphasize the continuous global burden of cognitive, neurological, and substance use conditions. With psychological conditions rising from the 12th to the 7th primary reason for loss of well-being globally since 1990, the necessity for efficient categorizations and therapies is evident. The Who's latest guidelines stress the importance of balancing benefits against potential harms and emphasize cost-effectiveness and feasibility.
Dr. Alize Ferrari emphasizes that gaining knowledge from worldwide emergencies, like the COVID-19 pandemic, is crucial for readiness in the face of forthcoming shocks affecting the prevalence of psychological well-being. Addressing recognized risk factors, increasing awareness, and reducing stigma are proactive steps in alleviating the burden of psychological disorders. Thorough evaluations of literature on psychological well-being, such as those commissioned by the Flourishing Minds Fund, demonstrate that psychological disorders make up a substantial part of the worldwide disease load and that the disparity in occurrence is a crucial aspect to consider for interventions.
As the DSM continues to adapt to new findings and technologies, staying informed about these developments is vital for parents and professionals dedicated to supporting those with mental health issues. By doing so, they can ensure the most accurate and compassionate care for their loved ones.
Conclusion
In conclusion, the DSM-5 has a complex history shaped by shifts in understanding mental health and external influences. Efforts have been made to address financial conflicts of interest, and understanding the historical context is crucial for guiding future improvements. The DSM-5's organization and structure enhance diagnosis precision, and its key components provide a critical framework for understanding mental health disorders.
Cultural and gender considerations are important for inclusive diagnostic practices. The DSM-5's sections fulfill different functions, and updates in the DSM-5-TR reflect the evolving understanding of mental health conditions. The practical applications of the DSM-5 are significant, providing a common language for clinicians and guiding treatment planning.
Ongoing updates are needed to reflect the latest research. Future developments, including the integration of AI and advancements in research techniques, hold promise for enhancing diagnostic precision and treatment. Staying informed about these developments is essential for supporting individuals with mental health issues.




