Introduction
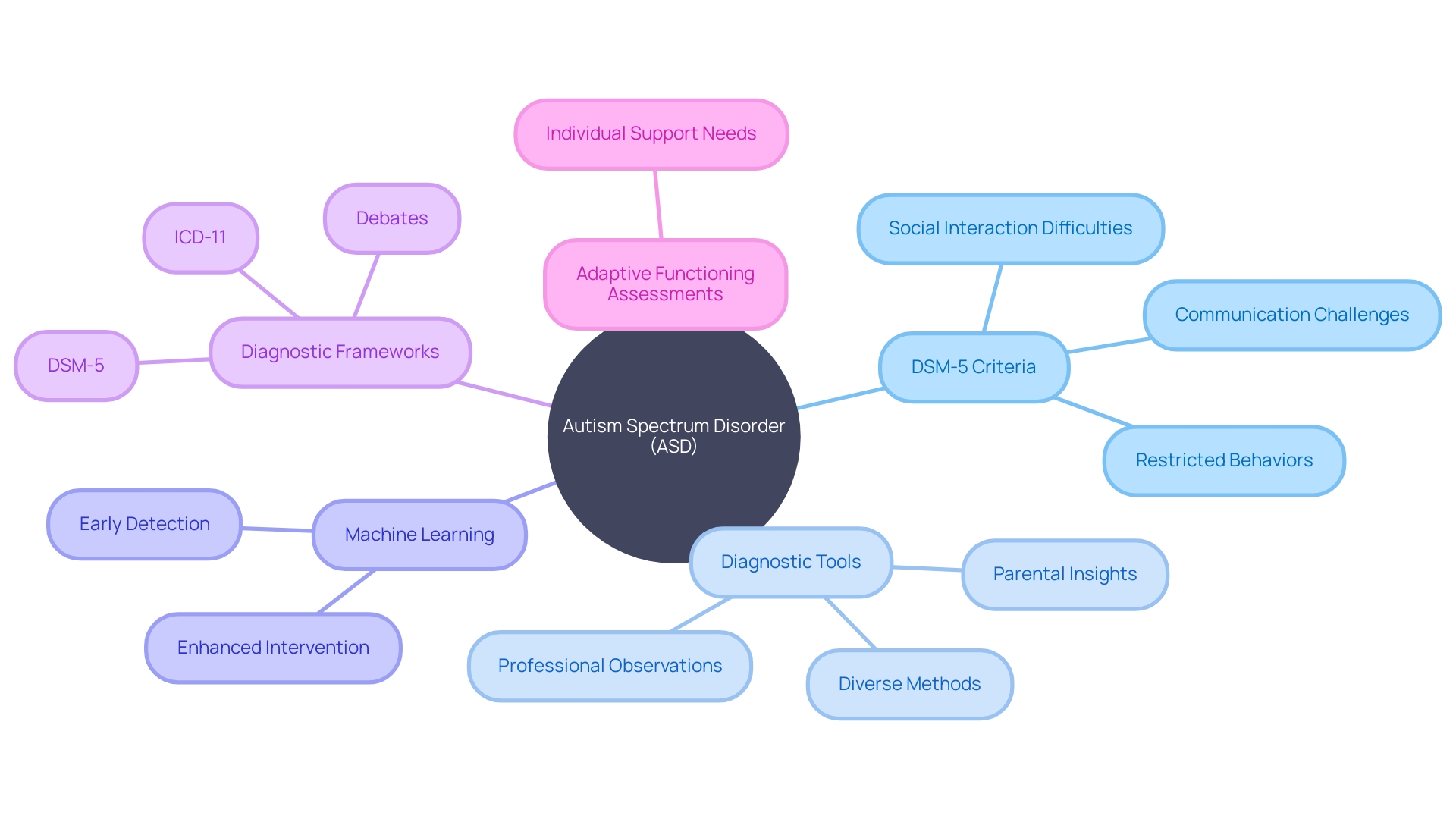
Autism spectrum disorder (ASD) is a complex condition that affects individuals in unique ways, impacting their social skills, communication, and behavior. To identify ASD, clinicians rely on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), which outlines specific criteria. Understanding these criteria is crucial for early diagnosis and providing essential resources and support.
Despite common misconceptions, research has shown that autism is not linked to vaccines, parenting styles, or nutrition. Genetic and neurological differences play a significant role in ASD. Advances in machine learning offer promise in refining diagnostic methods and improving outcomes through timely interventions.
However, debates continue regarding the classification of ASD and the need for objective frameworks. By appreciating the spectrum nature of autism, we can ensure that individuals receive the tailored support necessary for their well-being and success.
Understanding the DSM-5
Autism spectrum disorder (ASD) is a complex condition that manifests in a variety of behaviors, affecting social skills, communication, and behavior in ways unique to each individual. Clinicians rely on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), to identify ASD through a detailed set of criteria. According to the DSM-5, key characteristics of autism include persistent challenges in social interaction and communication across multiple contexts, and restricted, repetitive patterns of behavior or interests.
Examples of these traits are echolalia (the repetition of sounds or phrases), rigid routines, intense specific interests, and varying sensitivity to sensory input.
The CDC estimates that autism may affect as many as 1 in 36 individuals, making early and precise diagnosis pivotal for providing essential resources and support. Despite common misconceptions, autism is not linked to vaccines, parenting styles, or nutrition, but research suggests genetic and neurological differences play a crucial role. Advances in machine learning promise to further refine diagnostic methods, potentially improving outcomes for individuals with ASD and their families by facilitating timely interventions.
As we navigate the nuances of ASD diagnosis, it is critical to acknowledge the debates surrounding the classification of the disorder. Some argue that the ICD-11's broad and non-mandatory feature set for ASD diagnosis might blur the lines between autism and other mental disorders or autism-like traits. This highlights the importance of objective, behavioral, and neurodevelopmental frameworks in diagnosing ASD.
Ultimately, understanding ASD's spectrum nature helps us appreciate the individual experiences of those with autism, ensuring they receive the tailored support necessary to thrive throughout their lives.
Importance of Diagnostic Criteria for Autism
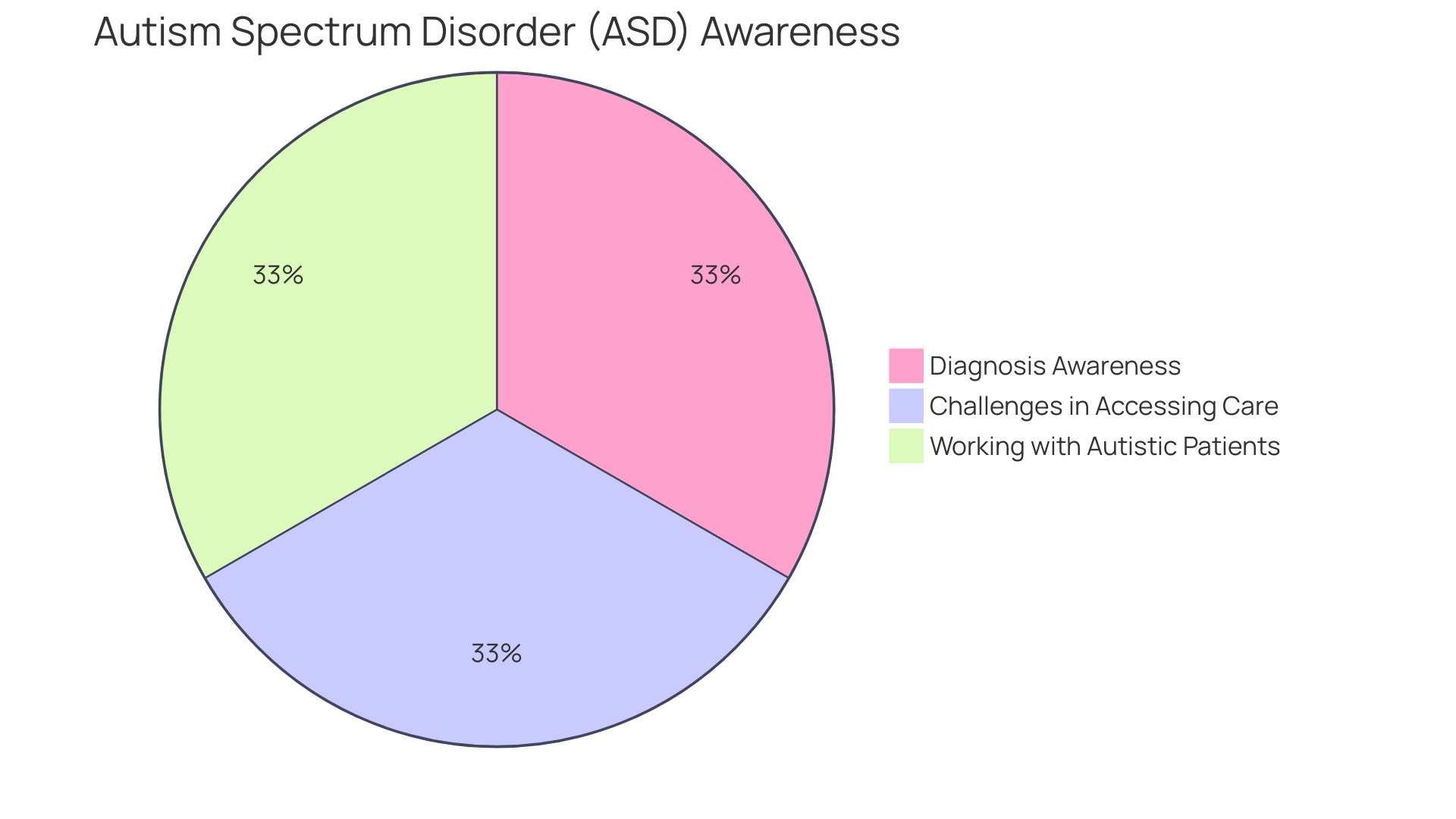
Understanding the nuances of autism spectrum disorder (ASD) is crucial for accurate diagnosis and support. The American Psychiatric Association's Diagnostic and Statistical Manual, Fifth Edition (DSM-5), provides essential criteria that healthcare professionals use to assess the presence and severity of ASD symptoms. These criteria focus on persistent differences in communication, social interaction, and restricted, repetitive behaviors across various environments, such as difficulty with transitions or extreme sensitivity to sensory stimuli.
The DSM-5's standardized approach is pivotal in distinguishing ASD from other developmental issues, given the complexity and spectrum nature of autism.
Recent analyses emphasize the diversity of ASD symptoms and the need for a variety of diagnostic tools. With an estimated 1 in 36 individuals affected by autism, it's clear that no single tool or observation can capture the full range of autistic experiences. Professionals rely on a combination of parental insights and their own observations to form a diagnosis, which may involve referrals to specialists such as neurodevelopmental pediatricians or geneticists.
Furthermore, research in machine learning offers promising advancements in diagnostic solutions, with the potential to enhance early detection and intervention. However, debates continue regarding the clinical utility of current diagnostic frameworks, such as the ICD-11, which some argue may blur the distinction between ASD and other mental disorders due to its broad, non-mandatory features.
Clinicians and researchers alike strive for precision in diagnosis, acknowledging the importance of adaptive functioning assessments, which consider an individual's practical abilities, from self-care to understanding money and time. Such comprehensive evaluations are essential for tailoring support to each person's unique needs, enabling them to navigate life with the necessary resources.
DSM-5 Diagnostic Criteria for Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is understood through the lens of the DSM-5, which outlines two core areas: ongoing difficulties in social communication and interaction, and fixed, repetitive patterns of behavior or interests. ASD is often seen as a 'spectrum condition,' meaning it manifests uniquely in each person and to varying extents. Brain scans have uncovered structural differences in individuals with ASD compared to typical development, although the exact cause remains under investigation, with genetics and environmental factors being key areas of focus.
Despite misconceptions, there is no evidence linking vaccines to ASD. Early identification of ASD is crucial, as it enables access to resources that empower individuals to lead fulfilling lives. Current estimates suggest that up to 1 in 36 people may be on the autism spectrum, highlighting the importance of awareness and understanding of this condition that persists throughout a person's life, impacting behavior, social skills, and communication.
Criteria A: Persistent Deficits in Social Communication and Social Interaction
Individuals with autism often experience profound and persistent challenges in social communication and interaction. This can manifest as difficulty with back-and-forth conversation, limited sharing of interests or emotions, and struggles with initiating or responding to social interactions. Nonverbal communicative behaviors, such as eye contact and body language, can also be affected, making it hard to read and convey cues.
Establishing and maintaining relationships can be particularly challenging due to difficulties in understanding social norms, making friends, or adjusting behavior to suit different social contexts.
Studies have highlighted that, despite these challenges, autistic individuals can process social information and benefit from social learning, just like neurotypical individuals. This suggests that with the right support and educational approaches, such as those facilitated by online learning environments, autistic adults can enjoy and benefit from social interactions. The promotion of social cognition and interaction in a supportive context is thus critical, not only for personal development but also for educational attainment.
Autism's impact on social interaction is backed by statistical evidence. For instance, it is estimated that 1 in 45 adults in the U.S. have been diagnosed with autism spectrum disorder (ASD). Public health outreach and increased screening have raised awareness, but many adults with autism may remain undiagnosed or misdiagnosed.
Recognizing the signs of autism is the first step toward understanding and addressing the condition.
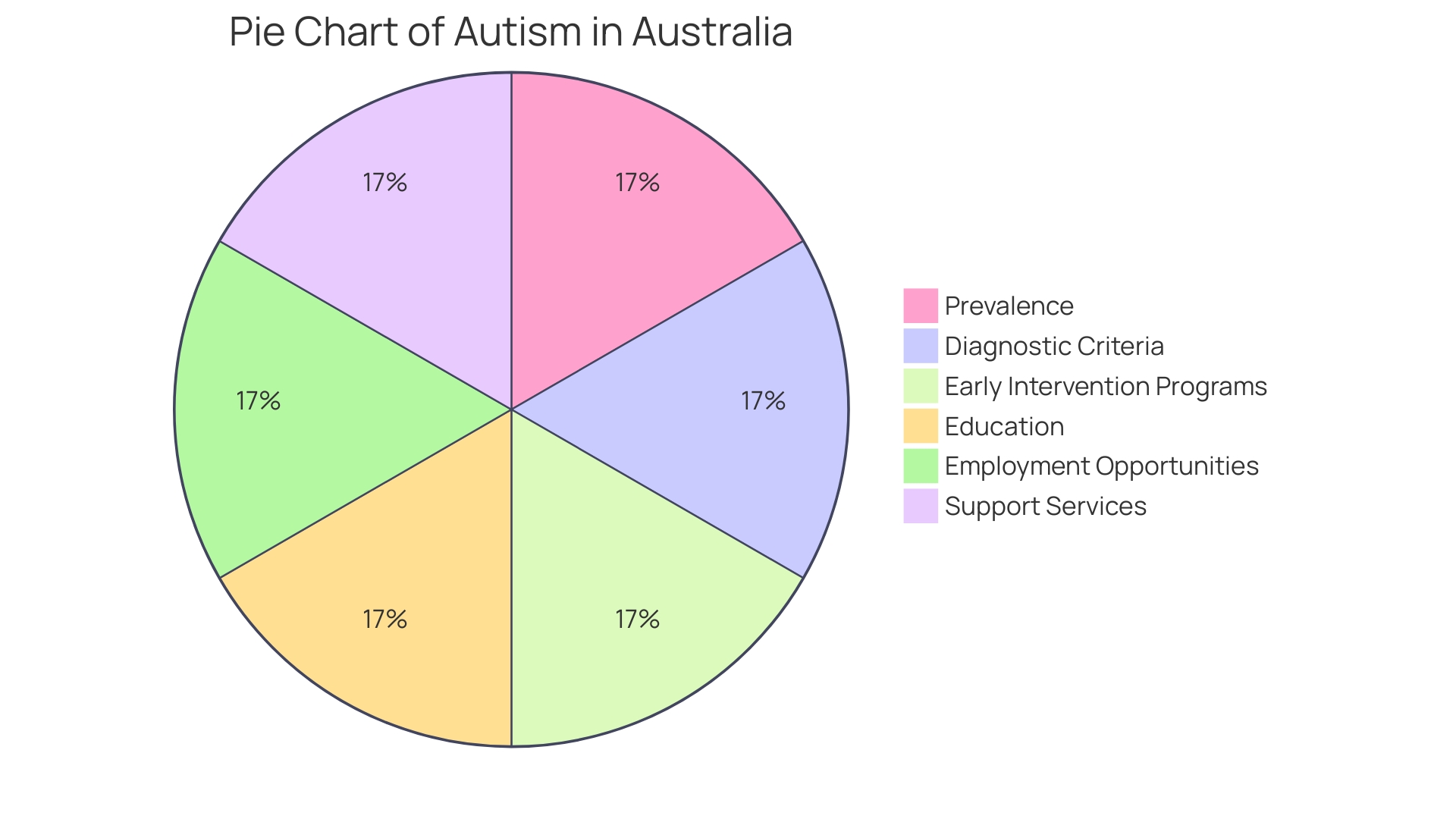
Autism is often referred to as a spectrum condition due to the variation in how it affects individuals. The American Psychiatric Association's Diagnostic and Statistical Manual (DSM-5) characterizes autism by persistent differences in communication and interpersonal relationships across various settings, as well as restricted and repetitive behaviors. According to the Centers for Disease Control and Prevention (CDC), autism may occur in as many as 1 in 36 individuals, highlighting the importance of early diagnosis and intervention.
In places like Australia, a comprehensive assessment is required for an autism diagnosis, involving professionals such as pediatricians and psychologists. Early intervention is key, with programs focusing on areas such as communication, social skills, and behavior management. The National Disability Insurance Scheme (NDIS) in Australia, for example, provides funding for services and supports, including early intervention for children with autism.
Education serves as a fundamental right, and inclusive education is integral for nurturing the potential of every individual with autism. The accurate identification of autistic individuals has led to improved data on its prevalence and a better understanding of the condition. With the continuous rise in prevalence, the need for inclusive and supportive environments for individuals with ASD is more significant than ever.
Deficits in Social-Emotional Reciprocity
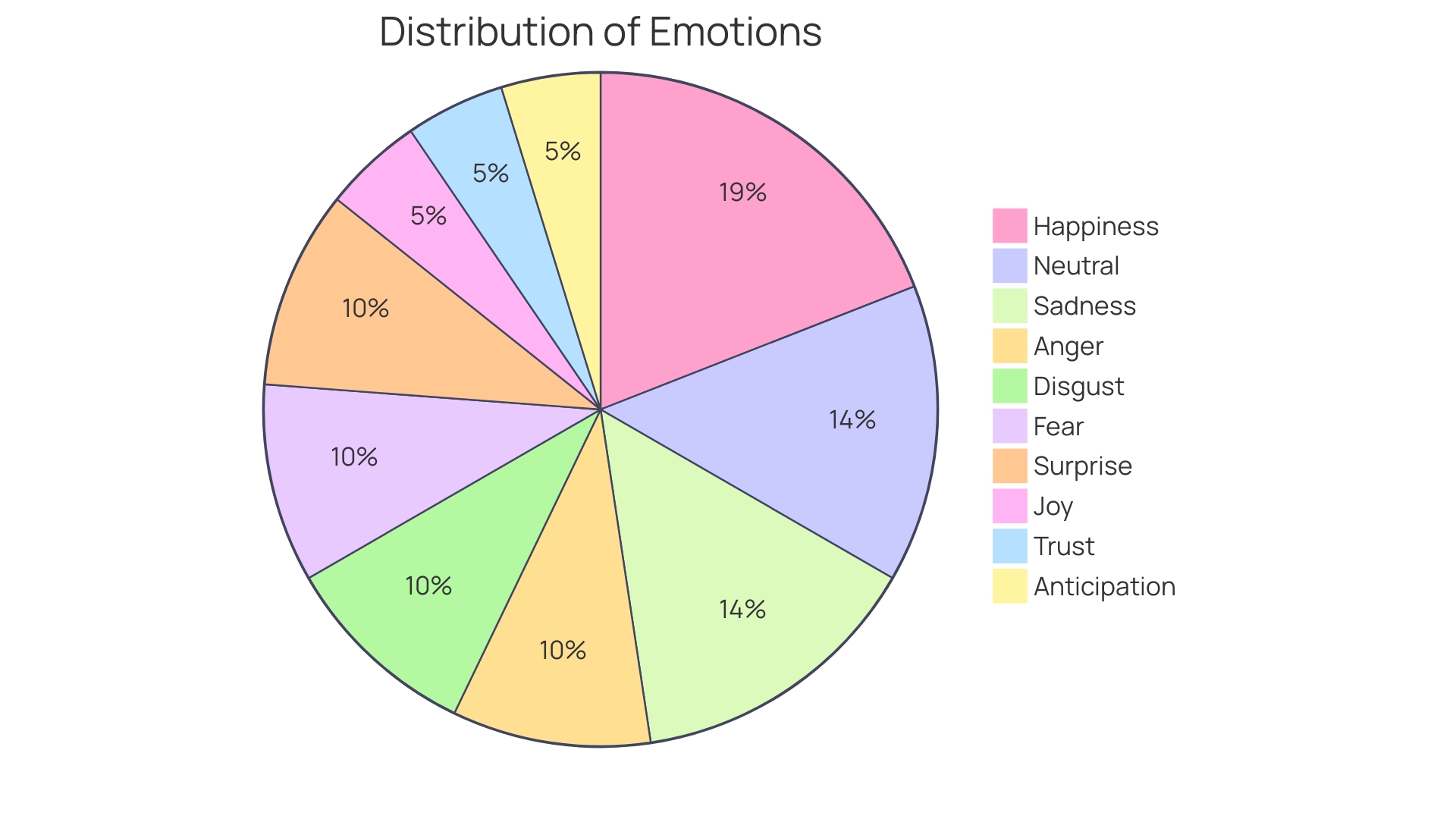
Autism Spectrum Disorder (ASD) presents unique challenges in social communication for those affected. Understanding emotions, engaging in conversations, and responding to social cues can be particularly challenging. Studies have shown that individuals with ASD often have difficulty recognizing and predicting the emotions of others, which can hinder social success.
This difficulty in understanding emotional transitions can be influenced by factors such as personal emotional experiences and external social cues.
Emotion production and mimicry are important concepts when considering social interactions in ASD. While neurotypical individuals might naturally express and imitate emotions, this can be less intuitive for individuals with autism, affecting their ability to connect and communicate effectively. The Wheel of Emotions model helps to categorize primary and secondary emotions, providing a framework for understanding the complex emotional experiences of those with ASD.
Recent advancements in technology, such as artificial intelligence, offer promising tools for early diagnosis and understanding of autism. These technologies have the potential to analyze social interactions and emotional expressions, contributing to more effective support and intervention strategies. For instance, data from children's games on tablets are being used to detect early signs of autism, which could lead to timely and tailored interventions.
The impact of the COVID-19 pandemic has underscored the vulnerability of individuals with ASD to external stressors, highlighting the need for robust support systems. Research during the pandemic indicated a deterioration in the well-being of people with ASD, as well as increased anxiety and stress among their parents, signaling an urgent need for effective coping strategies and support.
The mental health of individuals with autism is a critical concern, with many experiencing co-occurring conditions that are not always appropriately identified or supported. As research continues to evolve, it's important to focus on the entire lifespan of autistic individuals, including adults, where there is currently a significant knowledge gap.
In the context of social learning, studies have revealed that autistic adults, much like their neurotypical peers, benefit from social interactions during learning experiences. This finding challenges the misconception that social learning is less important for autistic individuals and emphasizes the universal value of engaging in social contexts for learning and development.
In summary, ASD affects social interaction in complex ways, but with a deeper understanding of emotional processing and the use of innovative tools for diagnosis and support, individuals with autism can achieve improved social integration and mental health outcomes.
Deficits in Nonverbal Communication
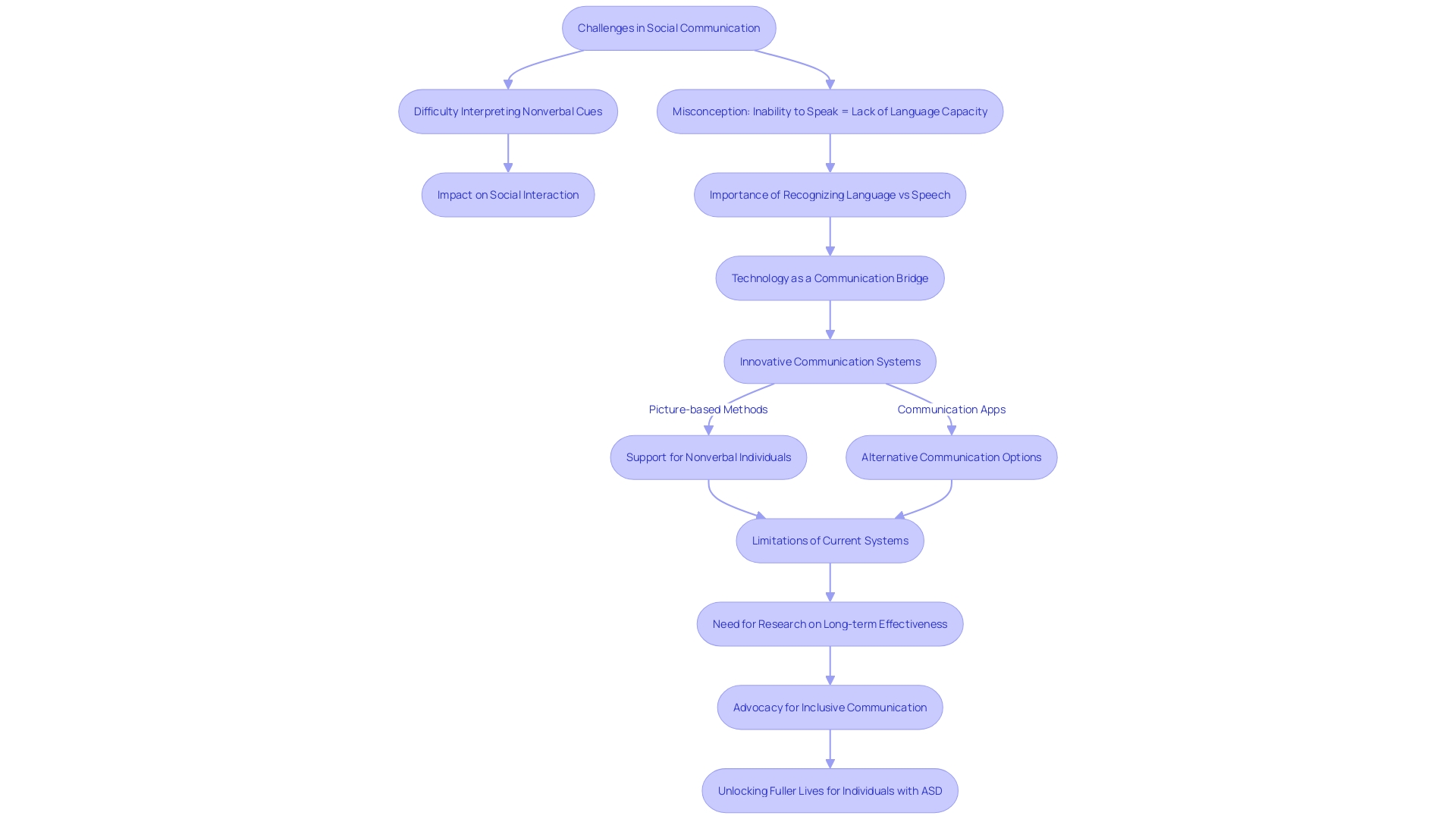
Autism spectrum disorder (ASD) encompasses a range of neurodevelopmental conditions, prominently characterized by challenges in social communication. For many individuals with ASD, nonverbal cues such as facial expressions, gestures, and body language can be particularly difficult to interpret and use effectively. This can significantly impact their ability to engage in social interactions, as nonverbal communication is often a fundamental aspect of human connection.
Around one-third of children and adults with autism may not develop effective speech, even after extensive interventions (DiStefano et al., 2016; Tager-Flusberg & Kasari, 2013). Their struggles with speech do not, however, equate to an absence of language or intellect. For instance, nonverbal individuals can and do find alternative means to express complex thoughts and emotions.
Deaf individuals, for example, can convey nuanced language through sign language given the right support and instruction.
Despite the potential for alternative communication methods, there remains a pervasive misconception that the inability to speak reflects a lack of cognitive capacity for language. This conflation of speech with language can lead to significant barriers for nonspeaking individuals, who are often not provided access to effective language-based communication alternatives (Gernsbacher, 2004). Without these tools, opportunities for education, employment, and social engagement can be severely limited.
Innovative communication systems, like picture-based methods, have been developed for those who do not speak. However, these systems are not without limitations. They are often used primarily for making requests, and the vocabulary available is typically chosen by someone other than the user, which can restrict expressive capabilities (Ostryn et al., 2008).
The long-term effectiveness of these systems also lacks robust evidence (Howlin et al., 2007).
The potential of technology to bridge these communication gaps is becoming increasingly recognized. For example, the story of Gregory Tino, who was presumed to have limited intellectual ability due to his nonverbal status, highlights the transformative power of technology. With the help of communication programs, Tino learned to write, unveiling his intellectual capacity and offering insight into the experiences of nonverbal autistic individuals.
Moreover, recent studies have explored how nonspeaking autistic individuals interact with written language. A study by Professor Vikram Jaswal of the University of Virginia employed a method akin to the game Whac-a-Mole, asking participants to tap on letters on a tablet. The findings suggested that, similar to literate non-autistic individuals, nonspeaking autistic participants could anticipate the sequence of letters in previously heard sentences, indicating their understanding of language and its written form.
The narrative of Jordyn Zimmerman, a non-verbal autistic woman who uses technology to advocate for disability rights, further exemplifies the potential within each individual when given the means to communicate. With the aid of a communication app on an iPad, Zimmerman has become an educator and a voice for many who are similarly challenged in speech.
The importance of recognizing the distinction between language and speech, and providing effective communication options for those with ASD, cannot be overstressed. By doing so, we can unlock doors to fuller, more inclusive lives for individuals with autism, allowing them to share their thoughts, feelings, and perspectives with the world.
Deficits in Developing and Maintaining Relationships
Navigating the social world can be particularly challenging for individuals on the autism spectrum. They often face difficulties in forming connections, grasping social norms, and establishing mutual friendships. Research underscores the unique challenges autistic individuals experience, especially as they transition into adulthood.
Dr. Gregory Wallace, an associate professor at The George Washington University, states, "We know the most about the transition period into young adulthood," but as they grow older, "we know almost nothing." Despite these challenges, strategies like setting clear boundaries and guidelines can be effective. For example, Dr. Sultan suggests that discussing preferred communication styles and comfort levels in social settings from the outset can mitigate uncertainties.
This approach aligns with the concept that autistic individuals may prefer routine and structure over the unpredictable nature of social interactions.
Statistics reveal autism's growing prevalence, with recent reports estimating that 1 in 36 children are diagnosed, marking a significant increase. This shift necessitates a deeper understanding of social dynamics among autistic people. Studies exploring the link between social communication and peer relationships have shown that mood disorders in autism may manifest as moral distress or impaired social communication, emphasizing the importance of nuanced support and education.
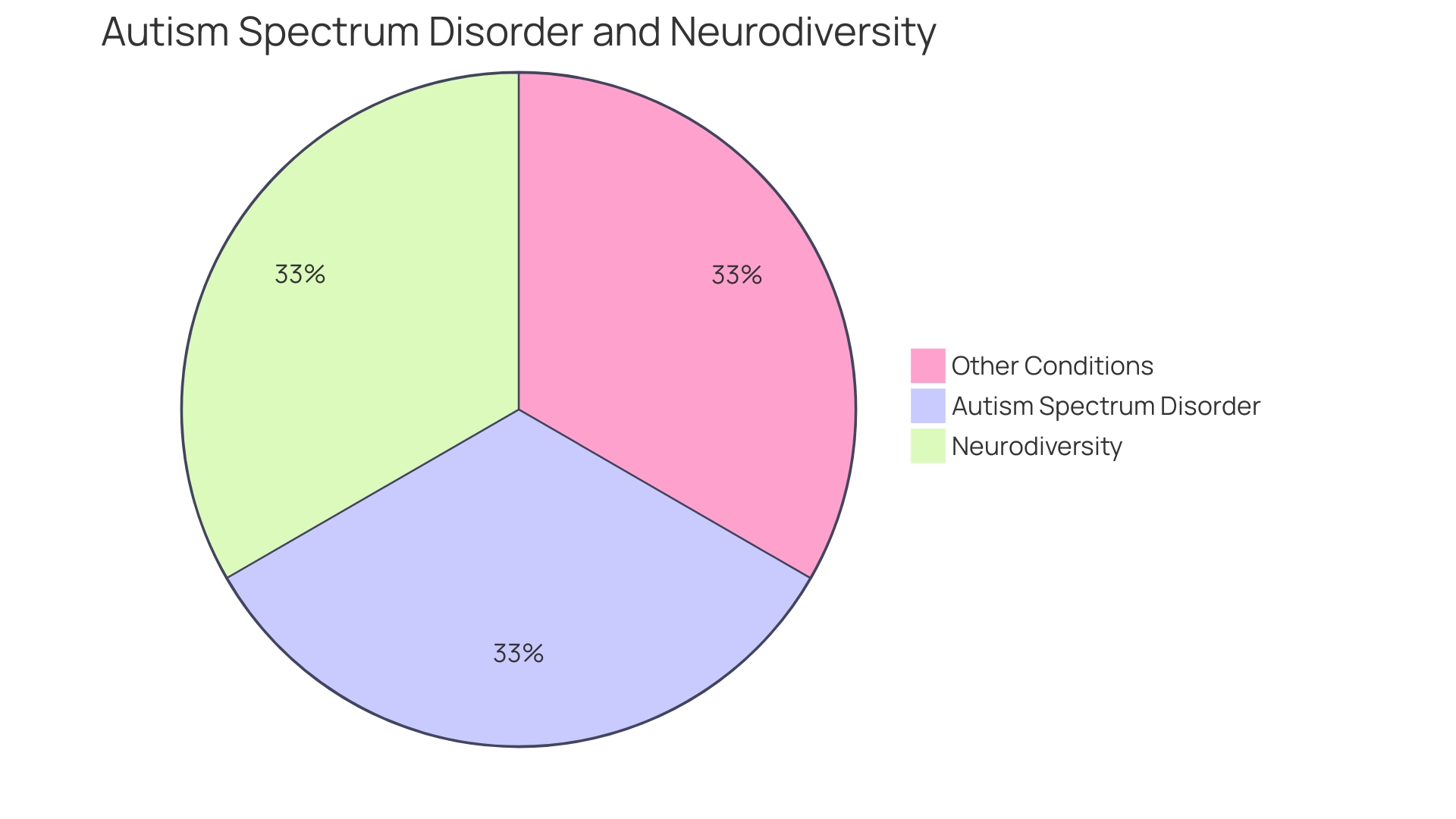
Historically, the medical model of disability has predominantly influenced the conceptualization of autism, distinguishing between 'normal' and 'pathological.' However, modern perspectives are shifting towards social models of disability, which view differences not as pathologies but as variations that society can accommodate. As a result, there's a growing recognition of neurodiversity, particularly in academic settings, which is supported by legislation like the Americans with Disabilities Act and Section 504 of the Rehabilitation Act.
The evolving understanding of autism is also reflected in the way autistic adults learn and engage. They can benefit from social interactions in educational settings just as much as their neurotypical peers, challenging the notion that they are disinterested in social learning. These insights suggest that with the right support and accommodations, individuals with autism can not only navigate but also thrive in social environments.
Criteria B: Restricted, Repetitive Patterns of Behavior, Interests, or Activities
Autism Spectrum Disorder (ASD) is a complex condition that manifests through a variety of behaviors, affecting individuals differently and to varying degrees. One of the core characteristics of ASD, as outlined in the American Psychiatric Association's Diagnostic and Statistical Manual (DSM-5), includes the presence of restricted, repetitive patterns of behavior, interests, or activities. These can take the form of an intense focus on specific topics, inflexible adherence to certain routines, repetitive physical movements, or an atypical response to sensory input, such as indifference to pain/temperature or adverse reactions to specific sounds or textures.
According to the Centers for Disease Control and Prevention (CDC), ASD occurs in approximately 1 in 36 individuals. Early diagnosis is crucial as it opens the door to valuable resources and interventions that enrich the lives of those on the spectrum. Despite extensive research, the precise cause of ASD remains unknown.
However, evidence suggests that genetic and neurological differences play a significant role. It's important to dispel myths concerning the origins of ASD; it is not a result of parenting styles, vaccines, or nutritional choices.
Families often begin the journey to diagnosis by discussing concerns with a primary care physician, who may then refer them to specialists for further assessment. Research continues to reveal more about ASD, with advanced techniques such as brain scans showing variances in brain structure between individuals with ASD and neurotypical individuals. As science progresses, understanding of ASD deepens, paving the way for better support and quality of life for those affected.
Examples of Restricted and Repetitive Behaviors
Autism spectrum disorder (ASD) is characterized by a range of behaviors that can affect daily life. One of the core aspects of ASD is the presence of restricted and repetitive behaviors. These can include physical movements such as hand flapping or rocking, a strong preference for routines, intense interests in specific topics, and heightened or reduced sensitivity to sensory input like touch and sound.
Understanding these behaviors is crucial as they can influence an individual's ability to navigate their environment.
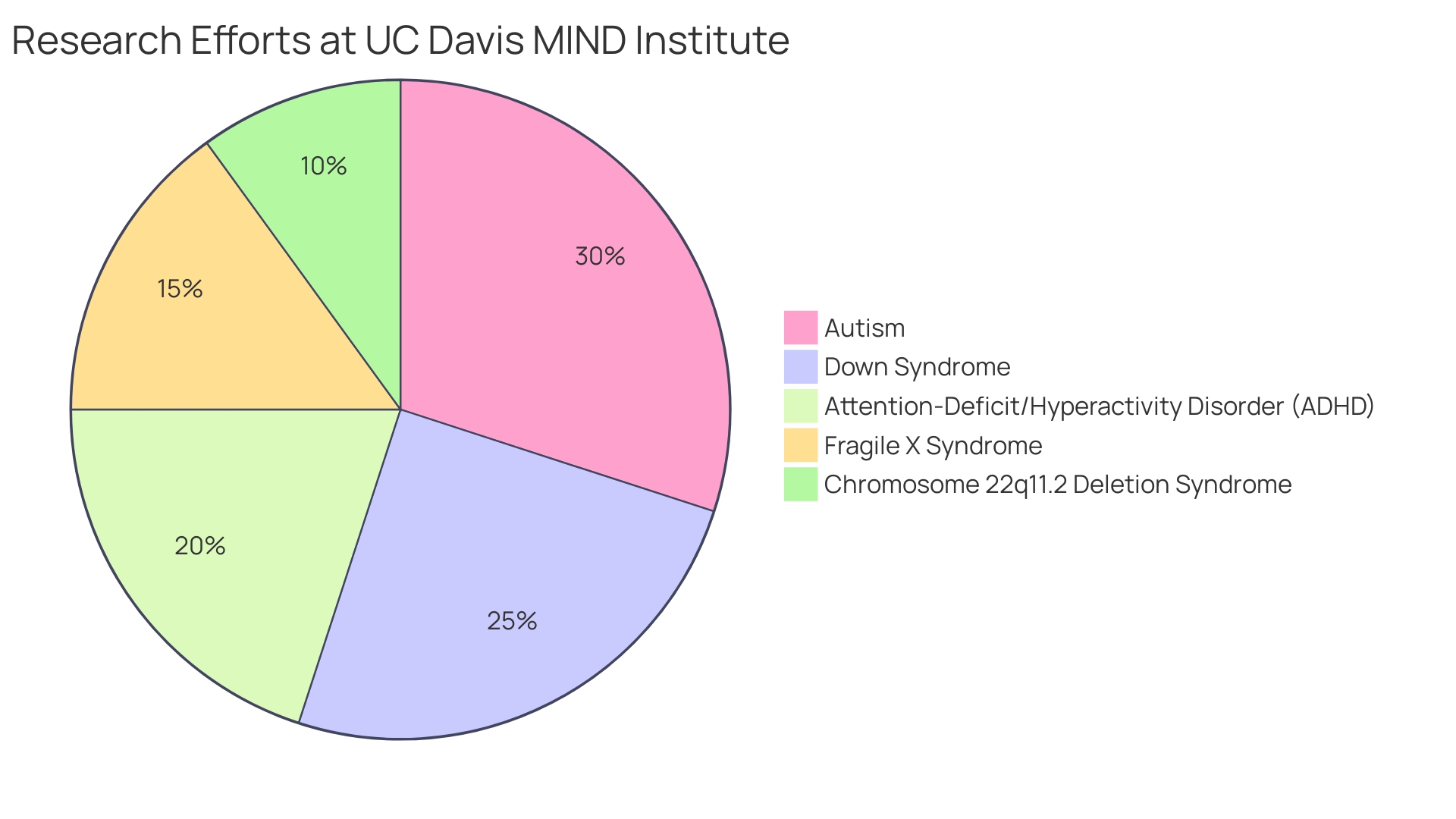
With 60–70% of individuals with autism also experiencing intellectual disability, research suggests that cognitive abilities, such as IQ, may influence how anxiety manifests in those with ASD. It's important to consider these factors when addressing the needs of autistic individuals. Additionally, the UC Davis MIND Institute emphasizes the importance of personalized support systems, acknowledging the diversity within the autism spectrum and the various ways it intersects with other developmental conditions.
Notably, repetitive and restricted behaviors, which may seem problematic to observers, are not always harmful. In fact, the drive to reduce these behaviors without understanding their purpose can overlook their significance for the individual. For example, a study analyzing 48 interventions aimed at decreasing such behaviors found that many did not consider the potential side effects or the reasons behind the behaviors.
Highlighting the potential of autistic individuals, projects like "Neurodivergent in STEM" showcase the unique contributions of neurodivergent people in scientific fields, celebrating the diversity of thought and approach they bring. These perspectives are integral to advancing our understanding of autism and fostering environments where autistic individuals can thrive.
Severity Levels of Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is characterized by a diverse range of symptoms and abilities, which the DSM-5 classifies into three severity levels to better tailor support and interventions. Level 1, 'Requiring Support,' indicates that an individual may face challenges with social communication and may exhibit behaviors that hinder their functionality in a typical environment. Level 2, 'Requiring Substantial Support,' suggests more pronounced difficulties in communication and social interactions, as well as a greater propensity for repetitive behaviors.
The highest level, Level 3, 'Requiring Very Substantial Support,' is designated for individuals who encounter severe challenges in these areas and require significant support to perform daily activities.
Understanding the severity levels is essential for healthcare professionals to provide the right resources that can offer individuals with autism the opportunities to live fully, as emphasized by the CDC's estimate that ASD affects up to 1 in 36 individuals. This framework facilitates a more personalized approach to managing the condition, recognizing that each person with ASD has unique needs and strengths, and contributes to the broader goal of ensuring that all individuals on the spectrum receive the support they need to thrive.
Updates and Revisions in DSM-5 Criteria
Revisions to the criteria for diagnosing autism spectrum disorder (ASD) in the DSM-5 have been pivotal in enhancing the precision of diagnoses. With a focus on observable and measurable behaviors, the DSM-5 criteria encompass persistent challenges in social communication and interaction across various contexts, coupled with restricted and repetitive patterns of behavior or interests. This approach underlines the importance of direct observation in identifying the characteristics of ASD and distinguishes it from other mental disorders with similar traits.
The changes aim to clarify the diagnosis by defining a set of behaviors indicative of ASD, acknowledging its diverse manifestations across the spectrum. The emphasis on early diagnosis is crucial, as it enables individuals to access resources that support their full participation in life. Statistics indicate that autism is present in as many as 1 in 36 individuals, highlighting the need for thorough and accessible screening processes.
Experts in the field continue to scrutinize the criteria, engaging in debates to refine the diagnostic process further. This ongoing discussion underscores the complexity of ASD and the necessity for evolving definitions that cater to the uniqueness of each individual's experience.
Elimination of Subtypes
The DSM-5 revision to autism spectrum disorder (ASD) diagnosis represented a significant shift in understanding this complex condition. Previously recognized subtypes, including Asperger's syndrome and pervasive developmental disorder-not otherwise specified (PDD-NOS), were integrated into the overarching category of ASD. This change underscores the dynamic nature of ASD and acknowledges the broad range of abilities and challenges faced by individuals on the spectrum.
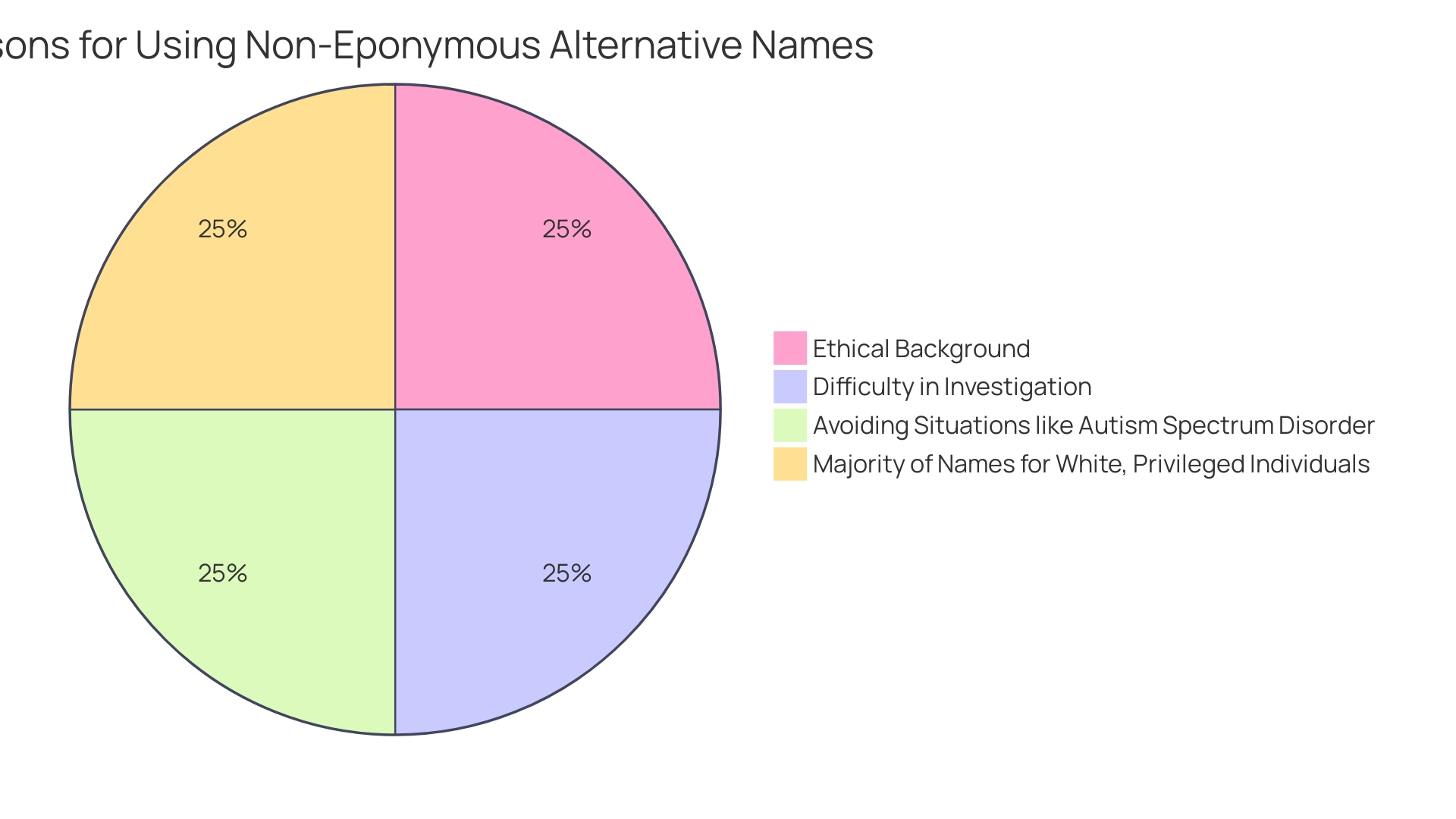
The decision to move away from eponymous labels within the medical community, as advocated by Pediatric Research, reflects a commitment to ethical standards and inclusivity. The use of non-eponymous titles eliminates potential biases and ensures a focus on the observable traits and behaviors essential for accurate diagnosis and support.
Moreover, the evolving guidelines, such as those developed by Austroads in partnership with the National Transport Commission and medical advisors, aim to enhance the management of individuals with ASD in various aspects of life, including driving. These guidelines recognize the unique considerations necessary for supporting those on the spectrum, emphasizing the importance of tailored approaches in healthcare and beyond.
In line with this progression, researchers are continually developing new tools and methodologies for early detection and intervention. Pediatricians are encouraged to incorporate autism screening into routine health visits, recognizing the pivotal role early identification plays in connecting families to vital resources and support systems.
As the understanding of ASD advances, it is increasingly clear that the condition is not solely defined by a set of symptoms but is influenced by environmental factors and individual experiences. This holistic perspective allows for a more nuanced approach to diagnosis and care, moving towards a model that respects the diversity of the autism experience.
Focus on Symptoms and Severity
The DSM-5, the American Psychiatric Association's cornerstone manual, refines the process of identifying autism spectrum disorder (ASD) by focusing on the presence and intensity of symptoms. This approach is designed to capture the unique challenges and necessary supports for each individual. Diagnosing ASD is multifaceted, often starting with the observations of parents or caregivers and followed by professional evaluation.
Specialists, such as neurodevelopmental pediatricians and child neurologists, may be involved to delve deeper into a child's behavior and development.
Research underscores the gravity of precise and early diagnosis. Current findings indicate a greater prevalence of certain medical conditions in autistic individuals, including central sensitivity syndromes like IBS and fibromyalgia. This emphasizes the need for early recognition and ongoing health monitoring to manage these comorbidities effectively.
Innovations in diagnosis are on the horizon. For instance, artificial intelligence is being explored to analyze retinal scans as a potential tool for autism detection. These advances promise to improve access to diagnosis, particularly for underserved populations.
Moreover, it's crucial to understand autism as a spectrum, where each person experiences it uniquely. With the CDC estimating autism's occurrence in 1 in 36 individuals, the DSM-5's nuanced criteria aim to ensure that each person's specific needs are identified and met, paving the way for resources and support that align with their distinct experiences of the world.
Inclusion of Additional Criteria
Recognizing that autism spectrum disorder (ASD) manifests uniquely across various ethnicities, races, and social backgrounds, the DSM-5 incorporates criteria that account for cultural and linguistic diversity. This is a crucial step forward, as it broadens our understanding that the presentation of autism's characteristics can be influenced by an individual's cultural context. For example, the National Institute of Health defines ASD as a set of complex neurodevelopmental disorders that can significantly affect communication and behavior.
These challenges may be perceived differently across cultures, impacting individuals' functioning in daily life and potentially contributing to societal misconceptions.
Studies have shown that while autism occurs globally, research and awareness are disproportionately focused on Western populations. Only about 40 years ago, ASD was predominantly associated with Western children, but today, we're expanding our scope to include diverse populations. Despite this progress, there remains a significant gap in our knowledge of autism in non-Western countries, which is deeply concerning.
Estimates of ASD prevalence in Africa vary, with reports of 2.3% in Nigeria and 0.68% in Uganda, highlighting the need for further research to understand autism within these contexts.
As we continue to investigate the complexities of ASD, it's essential to consider the genetic and neurological aspects. For instance, two common genetic mutations associated with ASD can lead to similar symptoms through different cellular mechanisms. Understanding these nuances is crucial to improving the quality of life for those with autism, including addressing sensory hypersensitivities like auditory processing difficulties.
By acknowledging the vast spectrum of autism and its global impact, we can better support individuals with ASD and their families, ensuring they receive the care and resources necessary to thrive.
Criticisms and Limitations of DSM-5 Criteria
The diagnosis of autism spectrum disorder (ASD), as characterized by the American Psychiatric Association's Diagnostic and Statistical Manual (DSM-5), is based on observed behaviors, including persistent challenges in social interaction and communication, as well as restricted and repetitive behaviors. Despite being the current standard, this framework has been met with critiques. Concerns have been raised about the DSM-5's ability to encompass the full diversity of autism presentations, which may lead to underdiagnosis or misdiagnosis in individuals.
As the International Classification of Diseases 11th Revision (ICD-11) suggests, ASD features a broad array of possible symptoms that are not always directly observable, casting doubt on the clinical utility of the current diagnostic criteria.
In an effort to address these issues, ongoing discussions in the medical and research community aim to refine the diagnostic criteria. The CDC estimates that ASD occurs in as many as 1 in 36 individuals, indicating the importance of accurate and precise diagnosis for early intervention. While there is no single known cause for autism, it is generally accepted to be associated with variations in brain structure or function.
Brain scans have revealed differences between individuals with ASD and neurotypical development, although the exact causes remain under investigation. It is clear that autism is not linked to vaccines, parenting styles, or nutrition, but rather a complex interplay of genetic and environmental factors.
Editors and commentators in medical publications like Pediatric Research have called for the use of non-eponymous names for conditions like ASD, both to avoid ethical issues and to move away from historical biases that favor white, privileged individuals' names as eponyms. Such changes reflect a broader shift in the medical community toward more inclusive and ethical practices. With a focus on improving the lives of those affected by ASD, the debate continues to evolve, informed by research and the lived experiences of individuals with autism and their families.
Conclusion
In conclusion, autism spectrum disorder (ASD) is a complex condition that affects individuals in unique ways, impacting their social skills, communication, and behavior. Clinicians rely on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), to identify ASD through specific criteria. Understanding these criteria is crucial for early diagnosis and providing essential resources and support.
Research has debunked common misconceptions, showing that autism is not linked to vaccines, parenting styles, or nutrition. Instead, genetic and neurological differences play a significant role in ASD. Advances in machine learning hold promise for refining diagnostic methods and improving outcomes through timely interventions.
By recognizing the spectrum nature of autism, tailored support can be provided to ensure the well-being and success of individuals. Early diagnosis is pivotal, as it enables access to resources that empower individuals to lead fulfilling lives. Professionals consider parental insights and their own observations to form a diagnosis, often involving referrals to specialists.
The spectrum nature of autism emphasizes the importance of personalized support and interventions. Each individual with ASD has unique needs and strengths, requiring resources that align with their distinct experiences. By acknowledging their individuality, we can ensure they receive the necessary support to thrive.
In conclusion, a confident, supportive, and empowering tone is used to provide guidance and resources to Parent Advocates. Understanding the criteria for diagnosing ASD, debunking misconceptions, and appreciating the spectrum nature of autism are key in providing the tailored support necessary for the well-being and success of individuals with ASD.




