Introduction
Understanding the DSM-5 Criteria for Autism
Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder that affects communication and behavior. The DSM-5 serves as a critical framework for clinicians diagnosing ASD, outlining specific criteria that must be met for a formal diagnosis. These criteria include challenges in social communication and social interaction, as well as restricted, repetitive patterns of behavior, interests, or activities.
Early childhood onset and impairment in everyday functioning are also key factors.
Diagnosing ASD can be complex, with recent discussions highlighting the evolving understanding of the disorder. The ICD-11 introduces a broader range of potential features for diagnosis, sparking debate over its clinical utility. Additionally, the neurodiversity movement emphasizes the worth of autistic individuals and advocates for broader acceptance of neurological differences.
Statistically, autism affects as many as 1 in 36 individuals, emphasizing the importance of early diagnosis and intervention. In Australia, comprehensive assessments by a team of professionals are conducted without age restrictions. Early diagnosis enhances the potential for successful intervention and support, supported by initiatives like the National Disability Insurance Scheme (NDIS).
Education and inclusion play vital roles in supporting children with ASD, and Australia has made significant advancements in support services. However, challenges in diagnosis, access to interventions, and societal acceptance persist. The goal is to create a more inclusive environment for individuals with ASD and their families by examining these factors.
By understanding the DSM-5 criteria and the evolving landscape of autism diagnosis, we can better navigate challenges and ensure the well-being of individuals with ASD.
Understanding the DSM-5 Criteria for Autism
The DSM-5 serves as a critical framework for clinicians diagnosing autism spectrum disorder (ASD), detailing specific criteria that must be met for a formal diagnosis. These criteria include persistent challenges in social communication and social interaction across multiple contexts, as well as restricted, repetitive patterns of behavior, interests, or activities. These symptoms must be present from early childhood and limit or impair everyday functioning.
Recent discussions in the field have highlighted the complexity of diagnosing ASD. The ICD-11, for instance, introduces a broader range of potential features for an ASD diagnosis, some of which may not be immediately observable. This approach has sparked debate over its clinical utility, given the subjective nature of certain concepts like 'compensation' and 'symptoms only apparent in retrospect.'
Moreover, the neurodiversity movement emphasizes the intrinsic worth of autistic individuals, advocating for a broader acceptance of neurological differences. As understanding evolves, diagnostic models and societal perceptions continue to be challenged and refined.
Statistically, autism is estimated to affect as many as 1 in 36 individuals. In Australia, diagnosing ASD involves a comprehensive assessment by a team of professionals, with no age restrictions for evaluation. Early diagnosis is pivotal, enhancing the potential for successful intervention and support.
The National Disability Insurance Scheme (NDIS) in Australia underscores the importance of tailored support, ensuring that individuals with ASD receive the necessary resources to thrive.
Education and inclusion play vital roles in fostering the potential of children with ASD. With the rise in autism awareness, Australia has made significant advancements in support services, although challenges in diagnosis, access to interventions, and societal acceptance persist. By examining these factors, the goal is to create a more inclusive environment for individuals with ASD and their families.
Criteria A: Persistent Deficits in Social Communication and Social Interaction
A crucial aspect of autism diagnosis centers around consistent challenges in social interaction and communication. These include a difficulty with give-and-take in social settings, understanding nonverbal cues, and cultivating relationships. Studies have shown that individuals on the autism spectrum may process social signals differently, which can affect their ability to engage in social learning and social cognition.
For instance, the subtleties of genuine versus posed smiles, which play a key role in social communication, can be particularly challenging to discern. This is significant because social signals like smiles convey crucial emotional information. Intergroup bias research highlights that even minimal group settings can influence the perception of such social signals, which may be even more pronounced for individuals with autism due to their unique social processing characteristics.
With the prevalence of autism estimated by the CDC to be as high as 1 in 36 individuals, understanding these social difficulties is vital for early diagnosis and intervention. Early detection enables access to resources that can significantly enhance the quality of life. Autism is characterized by a diverse array of behaviors and is often referred to as a spectrum condition.
The DSM-5 outlines specific criteria for diagnosis, emphasizing persistent differences in communication, social interactions, and restricted, repetitive behaviors across multiple environments.
It's important to note that brain scans have revealed differences in the shape and structure of the brain in individuals with autism compared to neurotypical development. While the exact cause of autism remains under investigation, the consensus is that it involves variations in brain structure or function, rather than being linked to vaccines, parenting styles, or nutrition.
When concerns arise regarding a child's development, parents often initiate the diagnostic journey through their primary physician, who may then refer them to specialists for further evaluation. These assessments incorporate descriptions from parents or caregivers and observations by professionals to form a comprehensive understanding of the child's behavior. There are many tools available to assess autism in young children, but no single tool should be used as a definitive basis for diagnosis.
Furthermore, it's pertinent to acknowledge that despite the challenges in social interaction, autistic adults can benefit from and enjoy social interaction-based learning as much as their neurotypical counterparts. This insight reinforces the importance of tailored educational approaches and further validates the diverse capabilities within the autism community. Understanding these elements is not only crucial for the diagnosis process but also for fostering environments that support the well-being and development of individuals with autism.
Criteria B: Restricted, Repetitive Patterns of Behavior, Interests, or Activities
Autism Spectrum Disorder (ASD) diagnosis, as outlined in the DSM-5, requires the identification of not only difficulties in social communication but also the presence of restricted and repetitive behaviors, interests, or activities. These repetitive behaviors manifest in various forms, including specific routines or rituals, intense special interests, and repetitive motor behaviors like hand-flapping. Factor analysis of the Autism Diagnostic Interview-Revised (ADI-R) reveals two subtypes: 'repetitive motor behaviors' and 'insistence on sameness' behaviors, which encompass specialized interests or rituals.
Research suggests that repetitive behaviors may serve as a means to alleviate anxiety, a hypothesis supported by numerous empirical studies. For example, repetitive listening to a certain song or engaging in stimming behaviors such as humming or hand-flapping can have a calming effect on the nervous system, reducing anxiety for individuals with autism.
Further studies, including recent advances involving AI and machine learning, have utilized large datasets to predict significant behaviors in individuals with ASD. These insights, derived from extensive data collected at institutions like The Center for Discovery, enable better interventions to mitigate the impact of these behaviors.
Moreover, the MOBSE framework developed by Dr. Smile's research team at Holland Bloorview emphasizes the influence of parent-child relationships and parental anxiety around feeding on all aspects of feeding, including medical and nutritional factors. This is particularly pertinent considering that children with autism are reported to have gastrointestinal issues at a higher rate than their neurotypical peers.
Understanding the multifaceted nature of repetitive behaviors and interests in autism is crucial. It not only enhances our diagnostic capabilities but also informs our approach to supporting individuals with ASD and their families. This includes considering various moderating variables such as intellectual disability and age, which may affect the relationship between anxiety and repetitive behaviors.
Criteria C: Symptoms Must Be Present Since Early Developmental Period
Recognizing autism spectrum disorder (ASD) early in a child's development is pivotal for effective intervention. The National Institute of Health defines ASD as a range of complex neurodevelopmental disorders caused by variances in the brain influencing communication and behavior. The spectrum nature of ASD means that symptoms, abilities, and skills can vary widely among individuals, impacting how they function in various life areas such as school and work, and can lead to societal misunderstandings and challenges.
Particularly concerning is the misconception that ASD primarily affects children in Western countries, which has only recently begun to be challenged by research in other regions. However, a scarcity of data from non-Western countries persists. This global oversight underscores the importance of recognizing the early signs of autism, such as challenges with eye contact or response to one's name by 9 months old, which are critical for timely diagnosis and support.
Innovations in technology are aiding in the early detection of ASD. A study utilizing a US database, SPARK, used machine learning to analyze children's information before 24 months of age, resulting in the 'AutMedAI' model, which identified 80% of children with autism. Moreover, research from JAMA Network Open and the Journal of the American Medical Association demonstrates that automated measures of children's looking behavior during social interaction videos can predict diagnostic outcomes.
These advancements are revolutionizing the approach to early diagnosis, allowing for interventions to commence much sooner.
Researchers like Warren Jones, PhD, and Ami Klin, PhD, have emphasized the importance of early intervention. With autism affecting 1 in 36 children in the U.S., the development of tools like 'the Marcus Test' for autism aims to diagnose children earlier. The combination of early identification, diagnosis, and subsequent intervention can greatly enhance the quality of life for individuals with ASD and their families.
As research continues to uncover the interplay between genetic and environmental factors in ASD, the goal remains clear: to enable early diagnosis and intervention for the best possible outcomes. This objective is not only a scientific pursuit but also a commitment to the well-being of children and families across the globe.
Criteria D: Degree to Which Autism Affects Daily Functioning
In the nuanced journey of autism diagnosis, the DSM-5 serves as a critical framework for assessing the extent to which autism affects an individual's daily life. By examining the influence of autism on key areas such as communication, social interaction, and adaptability, clinicians can tailor interventions and support to the unique needs of each person. Dr. David (Dan) R. Offord's conviction, "I do not mind if my children are in a race as long as the race is fair," aligns with the imperative of equitable treatment for autistic individuals, ensuring they receive the resources necessary to thrive in all life domains.
In line with the DSM-5, it's important to recognize the strengths and challenges that autistic individuals bring to their communities. The IACC's mission to enhance autism research and services complements this approach, as it collaborates with various stakeholders to foster inclusion and minimize health disparities. Autistic individuals face a higher risk of concurrent physical and mental health issues, underscoring the importance of comprehensive, ongoing support.
Indeed, the prevalence of autism, estimated by the CDC to occur in as many as 1 in 36 individuals, speaks to the critical need for accurate diagnosis and support. As diagnostic criteria evolve, it remains essential to balance behavioral observations with an understanding of the internal experiences and identities of those on the autism spectrum. This holistic view is instrumental in crafting effective interventions that address both the visible symptoms and the less apparent, yet significant, aspects of autism.
Criteria E: Traits Not Better Explained by Intellectual Disability
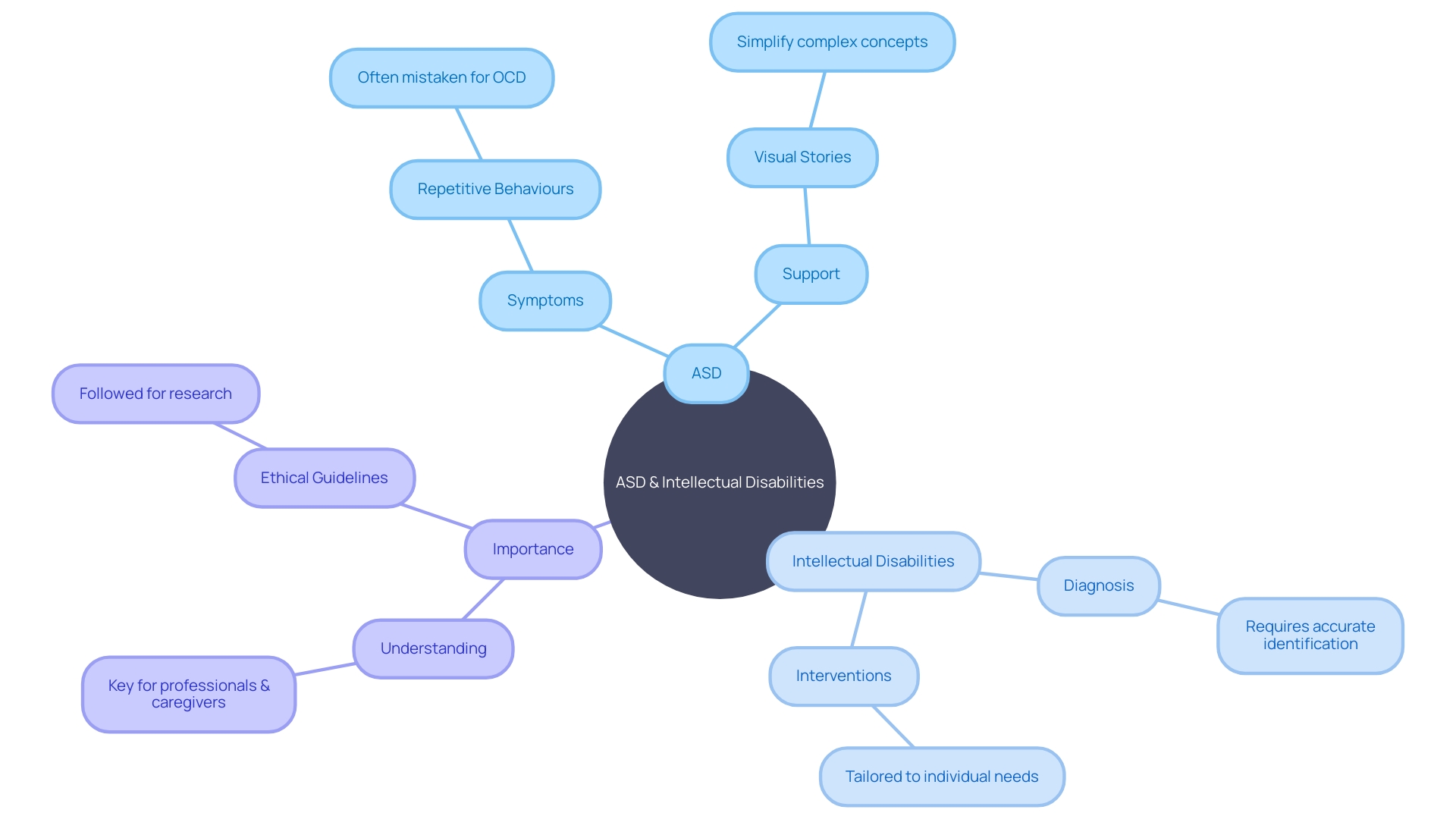
When differentiating autism spectrum disorder (ASD) from intellectual disabilities, it's imperative to recognize that while they may share overlapping symptoms, their root causes and implications for support are distinct. Intellectual disability, defined by limitations in intellectual functioning and adaptive behaviors, manifests before adulthood, affecting learning, reasoning, and problem-solving. In contrast, ASD is characterized by challenges in social communication and repetitive behaviors, regardless of intellectual capability.
Distinguishing ASD from intellectual disability is not merely a diagnostic nuance but a step towards tailored interventions. For example, individuals with high functioning autism, despite having average or above-average intellectual abilities, still experience significant social and sensory challenges. In the UK, where intellectual disability is termed 'learning disability,' studies indicate that individuals with such disabilities face healthcare disparities, leading to conditions like cancer being diagnosed later due to misconceptions or communication barriers.
Diagnosing ASD, therefore, involves a multifaceted approach that includes parent and caregiver insights and professional observation, guided by criteria like those outlined in the DSM-5. No single tool is definitive for diagnosis, emphasizing the need for a comprehensive evaluation by specialists. In countries like Australia, the diagnosis process incorporates a team of professionals and stresses early intervention, supported by systems such as the National Disability Insurance Scheme (NDIS), to optimize development and inclusion for those with autism.
Understanding the nuanced differences between intellectual disability and ASD is crucial for accurate diagnosis and ensuring individuals receive the personalized support necessary for their well-being.
Importance of Early Diagnosis and Support
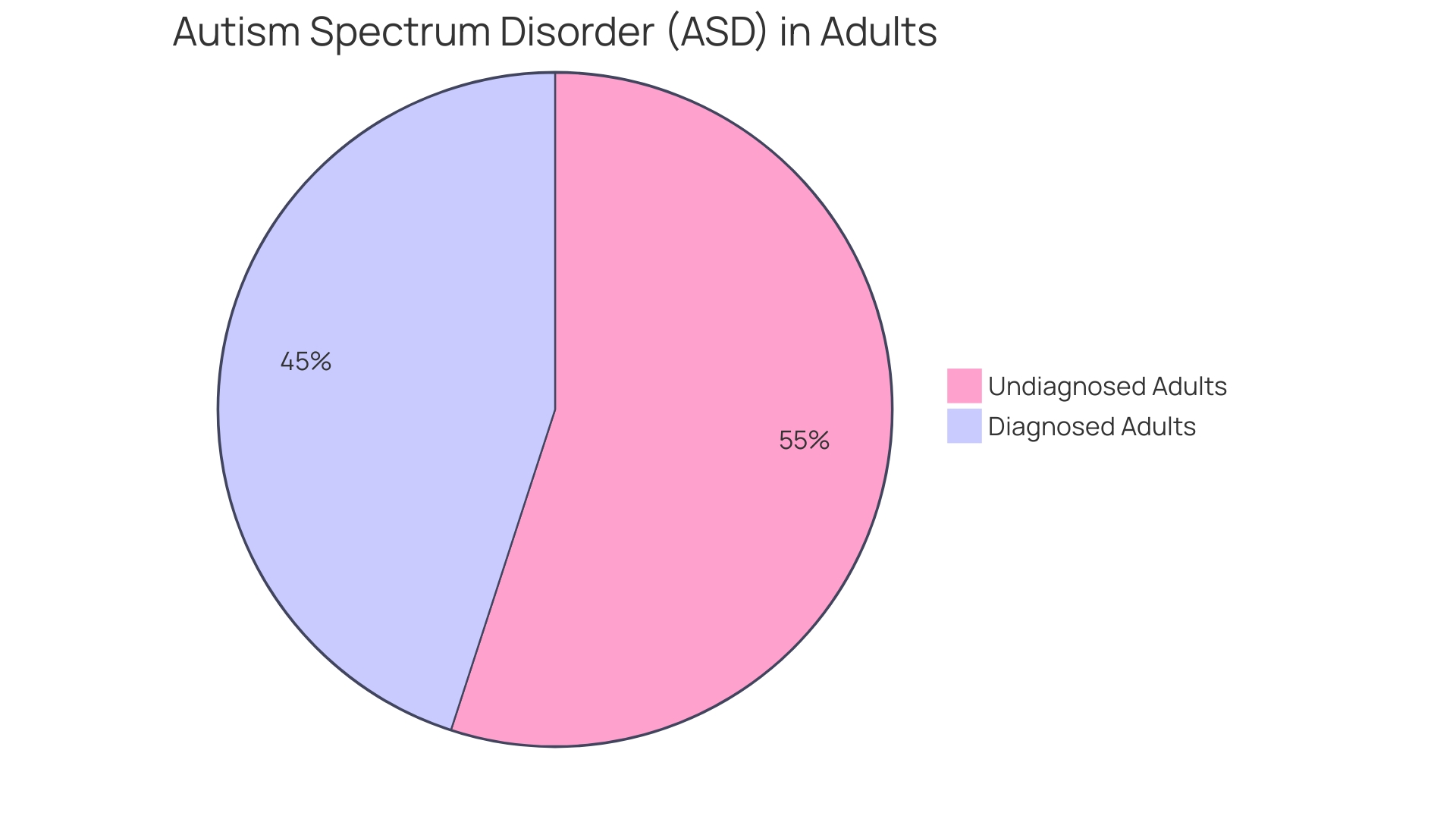
Understanding the benefits of early identification and support for autism spectrum disorder (ASD) can be transformative for affected individuals and their families. Early diagnosis is more than just labeling; it's about opening doors to tailored interventions and support systems that can dramatically alter developmental trajectories. With only 10-20 percent of individuals diagnosed with ASD before the age of 5 capable of living independently in adulthood, the stakes are high.
Researchers like Naviaux have illuminated the complex interplay of genetics and environmental factors in the onset of ASD symptoms, stressing the urgent need for early detection.
Intervention strategies, especially those providing at least 10 hours of weekly clinical support, have shown promise in enhancing family engagement and responsiveness to the needs of autistic children, thus benefiting the entire family unit. However, disparities in access to these services remain, as evidenced by the situation in New Zealand, where a fifth of families receive no such support, and the average is merely 2 hours per week.
The urgency for early and accurate diagnosis is further emphasized by organizations like The Autism Community in Action (TACA) and NeuroQure. TACA's reach extends to thousands of families, advocating for early behavioral therapy to optimize outcomes. NeuroQure's innovative approach aims to significantly reduce the stressful and drawn-out process of obtaining an ASD diagnosis to just a few weeks after birth, particularly for those with an increased familial risk.
The technological advances in diagnostics are also noteworthy, with new automated devices being tested at leading autism centers. These devices analyze children's eye movements to social stimuli, showing potential to predict the results of expert clinical assessments with high accuracy.
A neurodiversity-affirming perspective celebrates autism as a natural variation of human neurology rather than a defect, advocating for supportive environments over a cure-centric approach. This view acknowledges autism as a disability without undermining the need for support and services.
In conclusion, as we journey through the complexities and nuances of high-functioning autism, it's clear that the term captures a wide spectrum of experiences and abilities. From facing social challenges to navigating sensory sensitivities, individuals with high-functioning autism require a range of supports. Through a combination of early intervention, technology, community support, and a neurodiversity-affirming approach, we can foster environments where individuals with ASD can thrive.
Cultural and Individual Variations in Autism Presentations
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental disorder, characterized by diverse symptoms that affect communication and behavior. This diversity is not only present in the range of symptoms but also across different ethnic, racial, and socioeconomic groups worldwide. The variance in autism symptoms and the impact on daily functioning can lead to societal misconceptions and stigma, which can affect individuals and their families differently depending on their cultural context.
In many Western countries, ASD is diagnosed following a comprehensive assessment comprising pediatricians, psychologists, speech therapists, and occupational therapists who gather information from various sources, including observation of the child's behavior. In contrast, research and diagnosis of ASD in regions like West Africa have historically been limited, highlighting the need for a broader understanding of ASD in non-Western contexts.
Despite the challenges, recent developments in the field of neurodiversity suggest new ways to conceptualize neurodevelopmental conditions. The concept of neurodiversity appreciates the individual differences and complexities of those with ASD, recognizing the 'broader phenotype' of variation across the entire population. This approach emphasizes the importance of personalized support plans and inclusive practices that cater to the unique needs of each individual.
For instance, in Australia, the National Disability Insurance Scheme (NDIS) provides tailored support plans for children with autism, focusing on areas such as communication, social skills, and behavior management. This individualized approach is essential for enhancing development and functioning, as it takes into account the nuances of ASD presentation among different individuals.
Furthermore, the diagnosis of ASD in Australia emphasizes early detection and intervention, with no specific age restrictions for autism diagnosis. This aligns with research indicating the benefits of early intervention in improving outcomes for children with autism.
Understanding the nuances of ASD presentation across cultures and individuals is crucial for ensuring precise diagnoses and effective support. This requires ongoing research and education to foster inclusive environments where neurodiverse individuals can thrive.
Critiques and Limitations of the DSM-5 Criteria
The Diagnostic and Statistical Manual (DSM-5) serves as a critical tool for the assessment and diagnosis of autism spectrum disorder (ASD). Yet, its criteria are not without contention and limitations. For instance, the International Classification of Diseases 11th Revision (ICD-11) introduces a broader range of potential features for ASD diagnosis, which may not always be observed directly.
This raises concerns about the clinical utility of such broad criteria, as they could overlap with other mental disorders or autism-like traits, making precise diagnosis challenging. These criticisms suggest a move away from a purely neurodevelopmental perspective to a more subjective, social model of ASD, which incorporates concepts like identity and experiences that may not be quantifiable.
According to the Centers for Disease Control and Prevention (CDC), ASD may occur in as many as 1 in 36 individuals, emphasizing the need for accurate and effective diagnostic methods. While behaviors such as repetitive actions or difficulties in social interactions are key indicators, the DSM-5 emphasizes the importance of viewing each individual within the spectrum as distinct, with varying degrees of impact on their daily lives.
The pursuit of more precise diagnoses is echoed by experts who highlight the necessity of a multi-faceted approach to ASD assessment, one that goes beyond a single set of guidelines. As experts strive to refine the diagnostic process, it is crucial for those involved with ASD—whether as caregivers, educators, or medical professionals—to remain informed and adapt to the evolving understanding of what constitutes autism and how it can be identified.
Conclusion
Understanding the DSM-5 Criteria for Autism is crucial for diagnosing and supporting individuals with autism spectrum disorder (ASD). Early diagnosis is key, as it enhances the potential for successful intervention and support. Challenges in diagnosis, access to interventions, and societal acceptance persist, but the goal is to create a more inclusive environment for individuals with ASD and their families.
The DSM-5 criteria highlight challenges in social communication, social interaction, and restricted, repetitive behaviors. Brain scans reveal differences in the brains of individuals with autism, emphasizing the need for early intervention and tailored education.
Recognizing repetitive behaviors is crucial for diagnosis and support, as they can help alleviate anxiety. Early detection of ASD, aided by technology like machine learning, significantly improves outcomes for individuals and their families.
Differentiating between ASD and intellectual disability is important for tailored interventions. Early identification and support are transformative, and a neurodiversity-affirming perspective fosters inclusive environments.
Cultural and individual variations in autism presentations require a broader understanding of ASD. Tailored support plans and inclusive practices cater to unique needs. The DSM-5 criteria have limitations, and a multi-faceted approach is needed for precise diagnoses.
Understanding the DSM-5 criteria and the evolving landscape of autism diagnosis helps navigate challenges and ensure the well-being of individuals with ASD. Empowering Parent Advocates is our mission in supporting their children with ASD.




