Introduction
Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) are two distinct conditions that present unique challenges and characteristics. Understanding these differences is crucial for providing effective care and support. ASD is a developmental condition that affects social interaction, communication, and behavior, often noticeable from early childhood.
On the other hand, BPD is a mental health disorder marked by emotional instability, impulsive behaviors, and unstable relationships. While both conditions may exhibit overlapping symptoms, such as challenges with social interactions, it is important to recognize the nuances. This article explores the key differences between autism and BPD, including social interaction and communication differences, repetitive behaviors and interests, emotional regulation and mood stability, comorbidity and misdiagnosis risks, empathy and sensitivity, suicidality and self-harm risks, the importance of accurate diagnosis and tailored interventions, and treatment approaches.
By understanding these distinctions, healthcare professionals and advocates can provide more informed and personalized care for individuals with autism and BPD.
Key Differences Between Autism and BPD
Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) present unique characteristics and identification challenges. Each has its own set of symptoms and criteria that, when understood, allow for more effective and individualized care. For instance, ASD is a developmental condition often noticeable from early childhood, characterized by difficulties with social interaction and communication, as well as restricted and repetitive behaviors. It is a 'spectrum' disorder, meaning symptoms can vary widely from person to person, often making it a 'hidden condition.' On the other hand, BPD is a mental health disorder that typically emerges in adolescence or early adulthood, marked by intense emotional instability, impulsive behaviors, and a pattern of unstable relationships.
While both conditions can exhibit overlapping symptoms, such as challenges with social interactions and mood swings, it's important to recognize the nuances. For example, repetitive behaviors in ASD are often mistaken for obsessive-compulsive tendencies associated with BPD. Clarifying these differences is crucial, as a paramedic, like David, who encounters patients with autism, must adapt their approach to provide patient-centered care. This customization of treatment and comprehension is crucial for ensuring that people receive the support they require.
Moreover, the prevalence of ASD is significant, with recent statistics noting 1 in 45 adults in the U.S. diagnosed with the condition. Therefore, it's not uncommon for healthcare professionals to encounter adults who may have been undiagnosed or misdiagnosed in the past. Enhancing awareness and education about ASD and BPD among medical professionals, as well as the general public, is a step towards better recognition, diagnosis, and support for those affected by these conditions.
Social Interaction and Communication Differences
Autism Spectrum Disorder (ASD) encompasses a variety of challenges in social interaction and communication. For many people, understanding social signals, participating in nonverbal interaction, and establishing meaningful connections can be particularly challenging. By contrast, Borderline Personality Disorder (BPD) manifests through intense emotions, turbulent relationships, and a deep-seated fear of abandonment, which can lead to impulsive actions and significant mood swings.
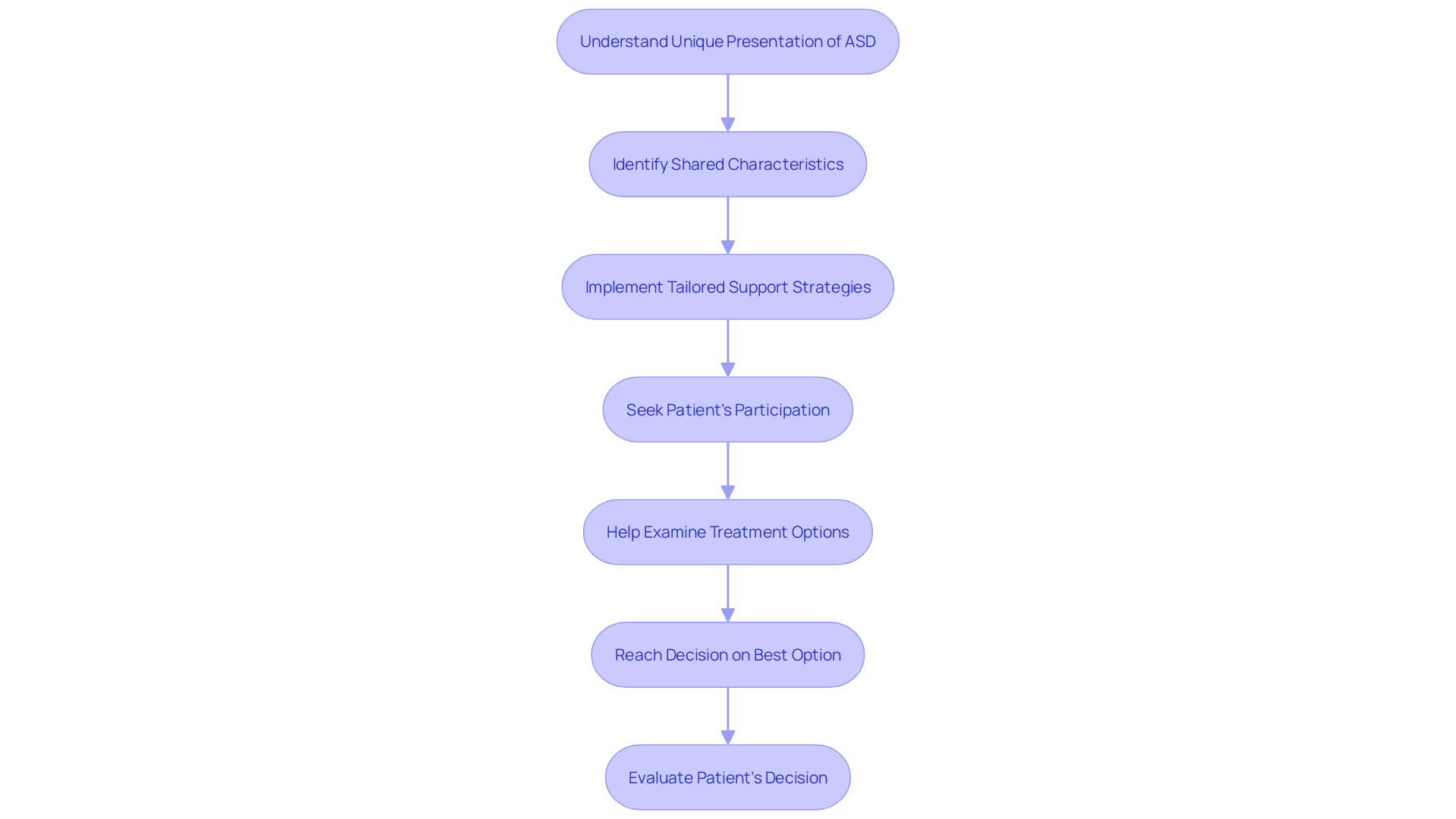
When healthcare professionals, such as paramedics, interact with individuals with ASD, they must adapt their approach to offer patient-centered care that acknowledges the unique presentation of ASD as a 'hidden condition.' Identifying the shared characteristics linked to the condition can aid in improved handling during medical interactions, guaranteeing that patients receive the most efficient care.
Moreover, research suggests that the social differences attributed to the condition need not be viewed solely as deficits. In specific cases, people with a certain condition might be less affected by societal expectations in dysfunctional or unethical circumstances, which could be seen as a possible advantage. This reframing promotes a more nuanced comprehension of autism, one that acknowledges the diverse capabilities and contributions of people across the autism spectrum.
While each condition presents its own set of challenges, it is crucial for healthcare providers, educators, and the community to differentiate between ASD and BPD. Such distinctions not only foster a deeper comprehension of each condition but also inform tailored support strategies that affirm the strengths and address the needs of those affected.
Repetitive Behaviors and Interests
Spectrum Disorder (ASD) is characterized by a range of behaviors, including an inclination towards repetitive actions and a deep-seated need for consistency in daily routines. Individuals with ASD might also exhibit an extraordinary concentration on particular subjects of interest. These characteristics sharply differ from Borderline Personality Disorder (BPD), where people may participate in impulsive actions and self-harming behaviors. These behaviors in BPD are often a desperate attempt to manage overwhelming feelings of emotional turmoil, and can manifest in various ways, such as substance misuse or uncontrolled eating.
Emotional Regulation and Mood Stability
Understanding and managing emotions present unique challenges in individuals with Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD), each displaying distinctive patterns of emotional regulation. In Autism, people may find it challenging to interpret and express their emotions, which can result in intense experiences and responses such as meltdowns or shutdowns when confronted with sensory overload or unforeseen alterations. These responses are often misunderstood, yet they are a reflection of someone's attempt to cope with the intense and confusing input from their environment.
Contrastingly, BPD is characterized by intense, fluctuating emotions that can escalate quickly and lead to impulsive actions, self-harm, or even suicidal ideation. The emotional turmoil experienced by people with BPD is profound, and the rapid shifts can cause significant distress. As mentioned by Dr. Aguirre, a central aspect of treating BPD with Dialectical Behavior Therapy (DBT) is the practice of validation—recognizing and accepting a person's feelings as understandable within their life context, without judgment. This approach is instrumental in helping individuals with BPD feel heard and supported, which can be a crucial step in learning to manage their emotions more effectively.
While emotional challenges in individuals with Autism Spectrum Disorder and Borderline Personality Disorder can manifest in ways that may seem similar, such as intense reactions to stress, the underlying causes and appropriate coping strategies differ. For individuals with a certain condition, strategies may involve sensory integration techniques and structured environments, while for another condition, DBT and other therapeutic interventions that focus on emotional regulation and relationship skills are often helpful. Dealing with these emotional regulation issues is not only essential for the well-being of people with these conditions but also for their families, who are seeking to comprehend and support their loved ones.
Comorbidity and Misdiagnosis Risks
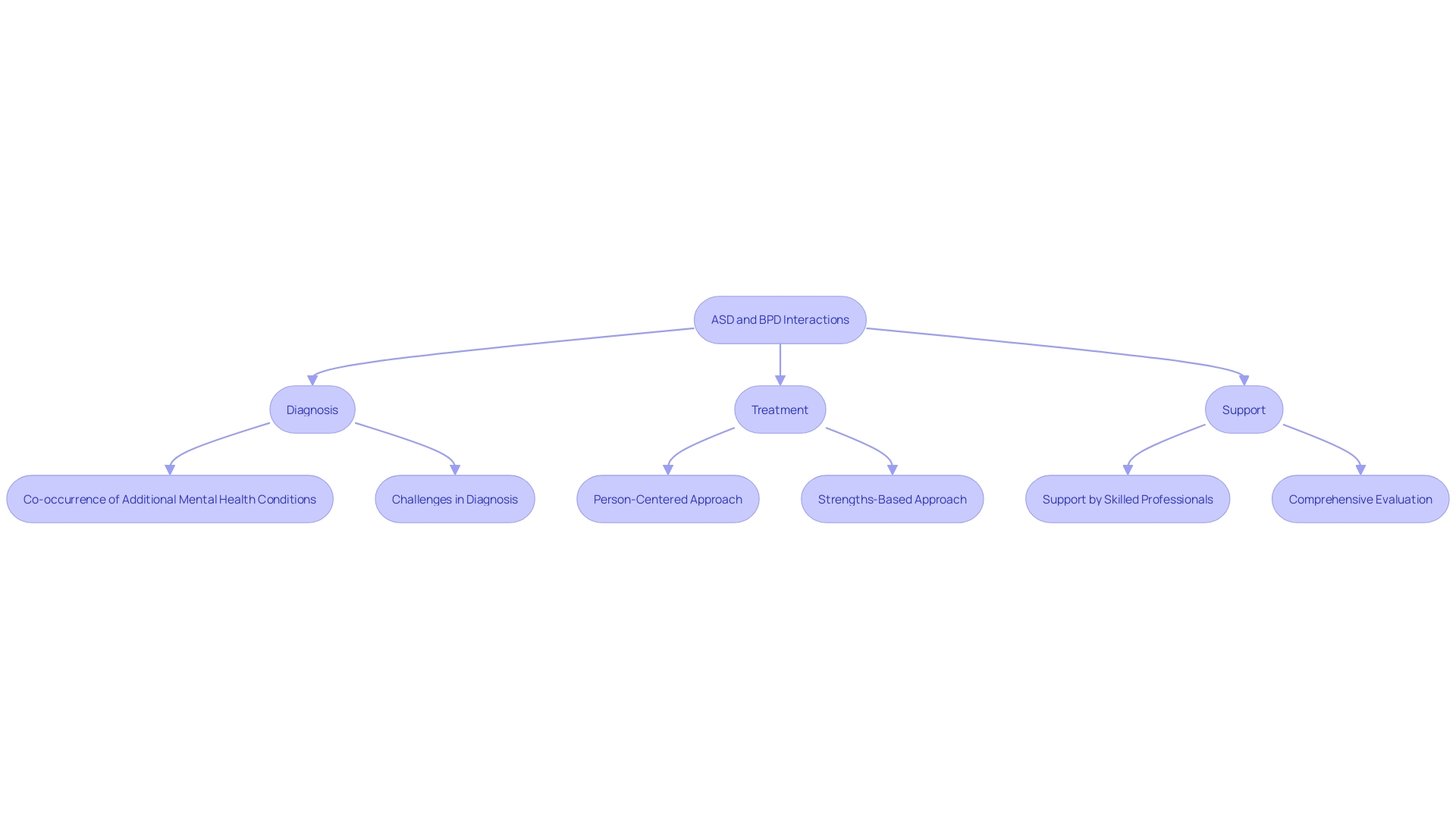
The convergence of Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) presents a complex clinical picture, with the potential for co-occurrence of additional mental health conditions. Misdiagnosis is a risk, especially because of the symptom overlap that may occur, notably among people with high-functioning Autism or BPD. It's emphasized that a person-centered and strengths-based approach is crucial, honoring the person's experience as more than a collection of symptoms. The neurodiversity movement, advocating for the perspective of autism as a natural variation of the human brain instead of a disorder to be cured, emphasizes the importance of this viewpoint. A thorough evaluation by a skilled professional is essential for an accurate diagnosis, offering a gateway to appropriate interventions and support that maximize positive outcomes.
Understanding the nuances and interplay between ASD and BPD is key to providing effective care and support. The intricate dance of diagnosis and treatment is further complicated by the potential for co-occurring conditions, making the expertise of professionals who are adept at navigating these complexities invaluable. In this vein, the neurodiversity-affirming practice does not minimize the challenges that come with autism but rather seeks to foster environments that support people on the autism spectrum. The statistics on the use of the International Classification of Diseases (ICD) illustrate the broader significance of proper diagnosis and recording of health information, which has far-reaching implications for monitoring trends and addressing public health concerns. As such, it is not only critical to diagnose accurately but also to appreciate the full context of an individual's life, ensuring they receive the care and support needed to thrive.
Empathy and Sensitivity in Autism and BPD
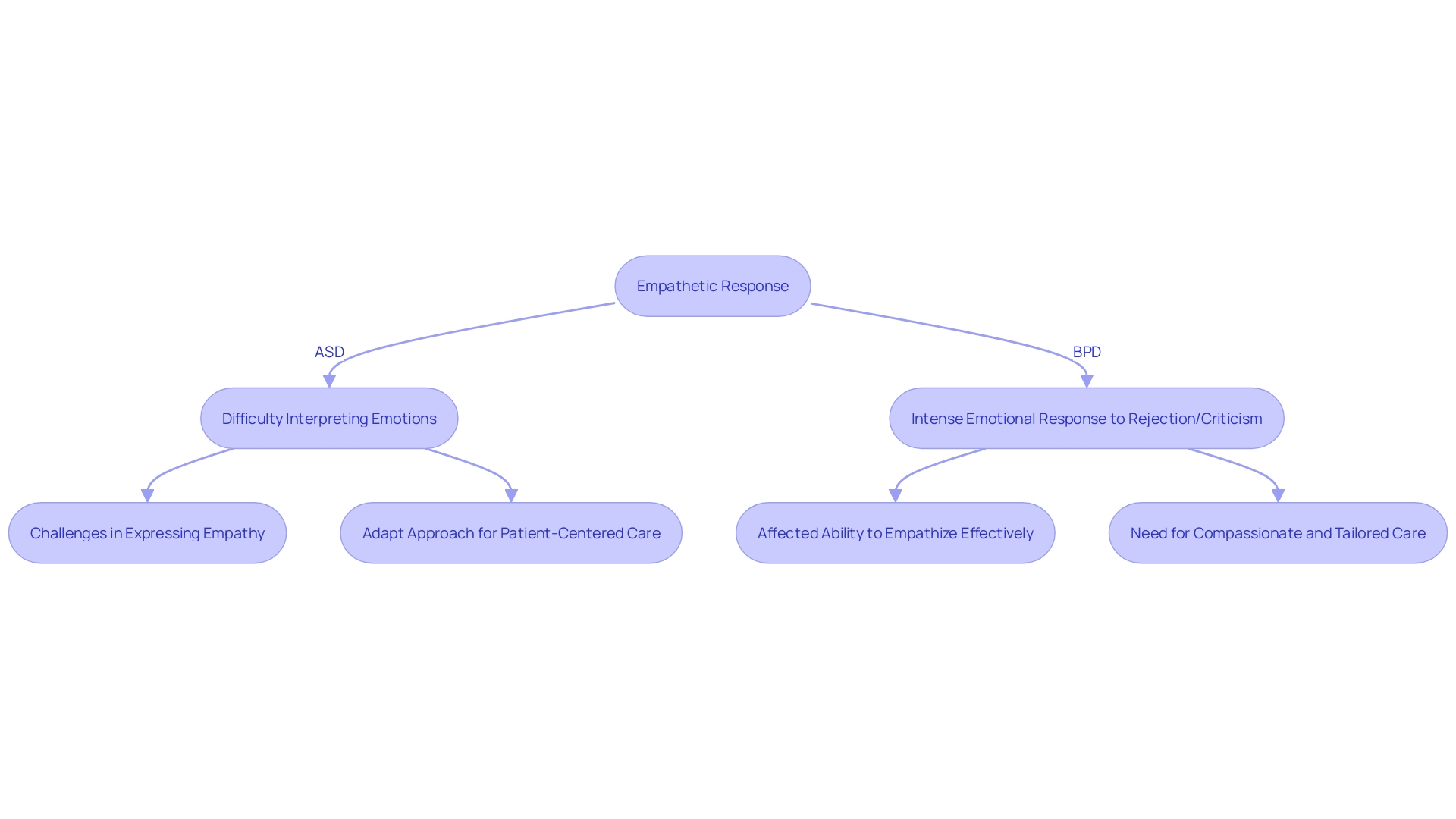
Understanding emotional responses and expressions of empathy is crucial, especially when comparing Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD). People who are on the spectrum may find it challenging to interpret others' emotions and social signals, which can make expressing empathy difficult for them. It's not that they lack empathy, but rather that the way they process and express it is different. On the other hand, people with BPD might be extremely sensitive to feelings of rejection or criticism, often leading to powerful emotional responses that can complicate their personal relationships.
One of the most important things for healthcare providers, such as paramedics, to remember is that ASD is a varied condition, often referred to as a 'hidden condition' because it doesn't have a fixed set of symptoms. This means that professionals like David, a paramedic dedicated to raising awareness about autism, must be adaptable and patient-centered in their care approach. Comprehending these intricacies is not only theoretical; it has real-life consequences for how people with ASD are treated in different environments, including urgent medical circumstances. Recognizing the diverse presentations of empathy in conditions like ASD and BPD is a step towards more compassionate and tailored care.
Suicidality and Self-Harm Risks
Recognizing the dangers of self-harm and suicidal tendencies is crucial in providing support for people with Borderline Personality Disorder (BPD). Research has highlighted that two-thirds of people with autism have contemplated suicide, with one-third having planned or attempted to take their own life, often due to the overwhelming challenges they face in social communication and heightened sensory sensitivities. Meanwhile, BPD is associated with a high incidence of self-harm, which serves as a maladaptive strategy to cope with intense emotional pain. Groups of specialists, including those at the Center of Excellence for individuals with autism at Cambridge, are actively working to dismantle obstacles and societal disapproval, highlighting the necessity for customized interventions that address the distinct encounters of every person. In particular, adolescents have been found to be at the highest risk, with around 17% of teenagers reporting self-harm, and the average age of the first incident being 13 years old. These alarming statistics underscore the importance of early and effective support systems to prevent these crisis and safeguard the wellbeing of those affected by Autism Spectrum Disorder (ASD) and BPD.
Importance of Accurate Diagnosis and Tailored Interventions
Early detection and intervention are crucial for individuals with Autism Spectrum Disorder or BPD to prosper. For Autism, interventions initiated at a young age can markedly enhance social capabilities and overall adaptive functioning. On the parallel, BPD can be effectively managed with validated treatments like Dialectical Behavior Therapy, which aims to improve emotional stability and interpersonal skills. Embracing a person-centered approach, which emphasizes strengths and acknowledges specific challenges, is essential for delivering impactful support and treatment.
In the realm of autism, the neurodiversity movement underscores the importance of perceiving autism as a natural variation in human neurology rather than a defect to be cured. This point of view is crucial for nurturing settings that include instead of exclude people on the autism spectrum. Programs like the Kevin and Avonte Program demonstrate the profound impact of specialized strategies to safeguard those prone to wandering, a common and perilous behavior in individuals with Autism.
The role of federal committees like the IACC and support from agencies such as the FDA is crucial in advancing research and services for individuals with autism spectrum disorder. These bodies, encompassing a diverse group of stakeholders, shape policies and recommendations that reflect a deep understanding of the multifaceted nature of individuals with the condition. Meanwhile, initiatives such as state Medicaid plans play a critical role in facilitating access to care and services, reflecting the profound influence state-specific approaches have on the autism community.
In light of these developments, it becomes clear that personalized treatment plans, backed by agencies like the NIMH, are vital. Network theory suggests that personalized strategies can break the reinforcing cycles of symptoms found in mental disorders, leading to more effective and enduring outcomes. This underscores the necessity of treatments that are as unique as the individuals they serve, moving beyond one-size-fits-all solutions to embrace the complexity of human diversity.
Treatment Approaches for Autism and BPD
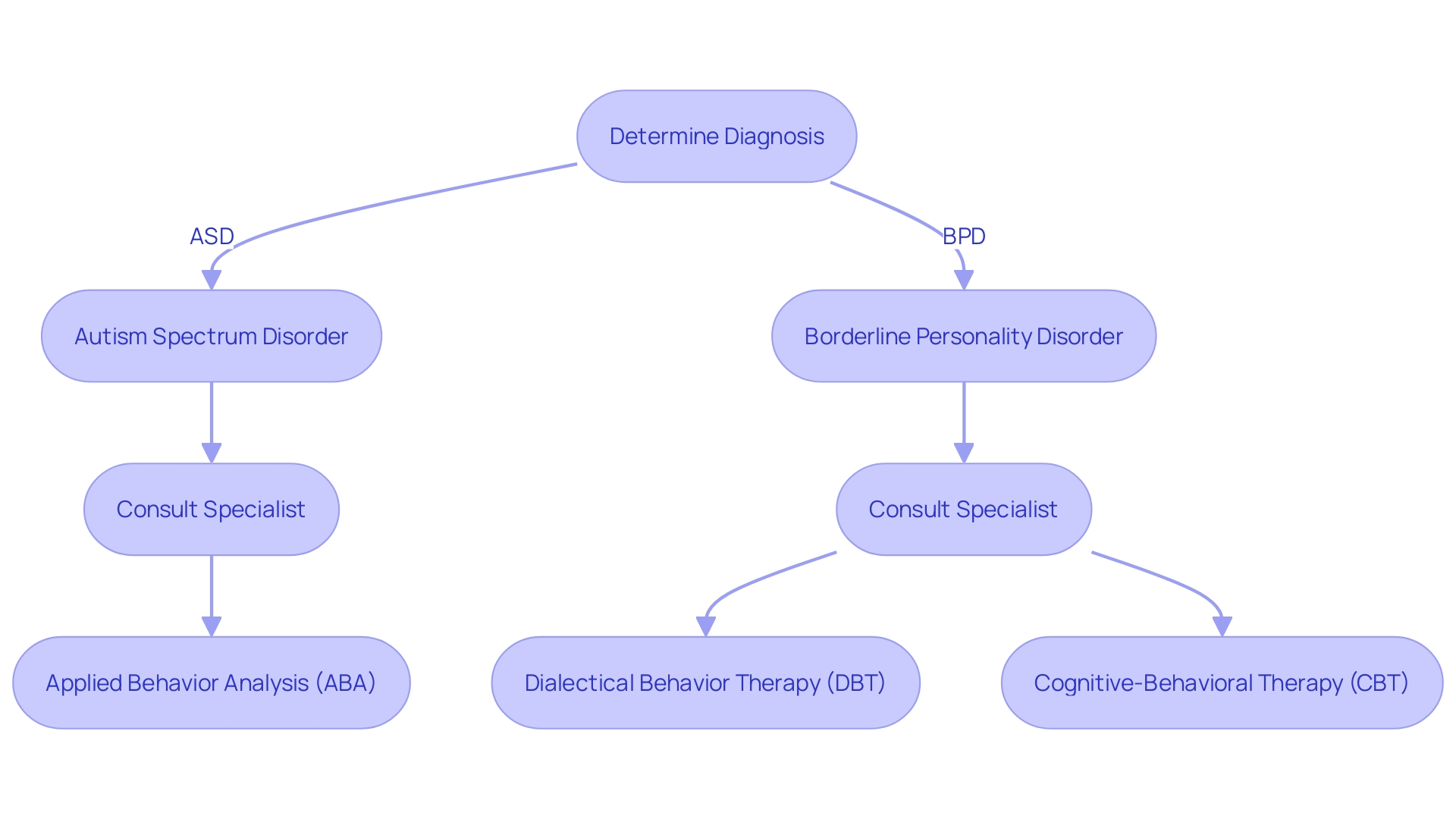
When addressing the challenges of individuals with Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD), it is crucial to adopt treatment strategies tailored to the specific nuances of each condition. For individuals with Autism Spectrum Disorder, Applied Behavior Analysis (ABA) stands out as a leading intervention, focusing on the enhancement of essential skills, modifying behaviors, and elevating social communication abilities. The recent release of the third edition of the ABA Practice Guidelines by the Council of Autism Service Providers underscores the commitment to excellence in this treatment, emphasizing the necessity for high-quality implementation to maximize efficacy.
BPD treatment, meanwhile, often necessitates a different approach, employing psychotherapeutic strategies such as Dialectical Behavior Therapy (DBT) or Cognitive-Behavioral Therapy (CBT). DBT, in particular, is constructed on a basis of validation, acknowledging and affirming the profound emotions and beliefs of people with BPD as expressed by Dr. Aguirre. This empathetic stance forms the core of DBT, facilitating a therapeutic environment where personal experiences are honored rather than dismissed.
Beyond these traditional therapies, neurofeedback presents a promising, non-invasive option that has demonstrated significant improvements in the cognitive abilities, mood regulation, and attention challenges often associated with autism. This technique fosters lasting changes within the brain, contributing to a more balanced and focused state of being.
Ultimately, the well-being of children and youth with these conditions is deeply intertwined with their ability to engage meaningfully in daily life across various domains. The wisdom of Dr. David (Dan) R. Offord reminds us that equity and mental health are achieved not just by recognizing the unmet needs but also by appreciating the intrinsic assets these individuals bring to their communities. To navigate this complex landscape, consultation with specialized professionals is indispensable for determining the most suitable treatment approach, thereby ensuring a 'fair race' for every child and adolescent on their unique journey.
Conclusion
In conclusion, understanding the differences between Autism Spectrum Disorder (ASD) and Borderline Personality Disorder (BPD) is crucial for providing effective care and support. While both conditions may share overlapping symptoms, recognizing the nuances is essential.
ASD is characterized by challenges in social interaction and communication, as well as repetitive behaviors and interests. BPD, on the other hand, is marked by emotional instability, impulsive behaviors, and unstable relationships. Tailoring interventions to address these specific characteristics is important.
Emotional regulation and mood stability differ in ASD and BPD. Individuals with ASD may struggle to interpret and communicate their feelings, while those with BPD experience intense, fluctuating emotions. Providing strategies for emotional regulation and relationship skills is crucial for individuals with BPD.
Comorbidity and misdiagnosis risks exist between ASD and BPD. Accurate diagnosis is essential to provide appropriate interventions and support. Understanding the nuances of each condition and seeking guidance from skilled professionals is crucial.
Empathy and sensitivity also differ in ASD and BPD. Individuals with ASD may find it challenging to interpret others' emotions and express empathy, while individuals with BPD may be highly sensitive to rejection or criticism. Recognizing these differences is important for delivering compassionate and tailored care.
Addressing the risks of suicidality and self-harm is crucial for individuals with ASD and BPD. Early detection and intervention are key to supporting their well-being. Tailored interventions, such as Applied Behavior Analysis for ASD and Dialectical Behavior Therapy for BPD, have shown effectiveness in improving social capabilities and emotional stability.
In conclusion, understanding the distinctions between ASD and BPD allows healthcare professionals and advocates to provide more informed and personalized care. Early detection, accurate diagnosis, and tailored interventions are essential for ensuring the well-being of individuals with these conditions. Embracing a person-centered approach and recognizing the strengths and challenges of each individual is key in supporting their unique journey.




